The Republic of Croatia, with a gross domestic product per capita of US$11,554 in 2008, is an economically less-developed Western country. The goal of the present investigation was to prove that a well-organized primary percutaneous coronary intervention network in an economically less-developed country equalizes the prospects of all patients with acute ST-segment elevation myocardial infarction at a level comparable to that of more economically developed countries. We prospectively investigated 1,190 patients with acute ST-segment elevation myocardial infarction treated with primary PCI in 8 centers across Croatia (677 nontransferred and 513 transferred). The postprocedural Thrombolysis In Myocardial Infarction flow, in-hospital mortality, and incidence of major adverse cardiovascular events (ie, mortality, pectoral angina, restenosis, reinfarction, coronary artery bypass graft, and cerebrovascular accident rate) during 6 months of follow-up were compared between the nontransferred and transferred subgroups and in the subgroups of older patients, women, and those with cardiogenic shock. In all investigated patients, the average door-to-balloon time was 108 minutes, and the total ischemic time was 265 minutes. Postprocedural Thrombolysis In Myocardial Infarction 3 flow was established in 87.1% of the patients, and the in-hospital mortality rate was 4.4%. No statistically significant difference was found in the results of treatment between the transferred and nontransferred patients overall or in the subgroups of patients >75 years, women, and those with cardiogenic shock. In conclusion, the Croatian Primary Percutaneous Coronary Intervention Network has ensured treatment results of acute ST-segment elevation myocardial infarction comparable to those of randomized studies and registries of more economically developed countries.
In 2002, 5,525 Croatians experienced acute myocardial infarction, and approximately 4,000 had ST-segment elevation myocardial infarction (STEMI). Of these patients, 54% were treated in county institutions with <100 acute myocardial infarctions annually and without intervention capabilities. Of these 4,000 patients, 62% were men, 39% were capable of working actively (22% of women and 49% of men), and more were affected by arterial hypertension and diabetes than patients in other European countries. Such a high percentage of STEMI could be explained by the underdiagnosis and underreporting of non-STEMI during that period. In 2007, 6,420 Croatians were hospitalized because of acute myocardial infarction but with a trend toward decreasing cardiovascular mortality overall.
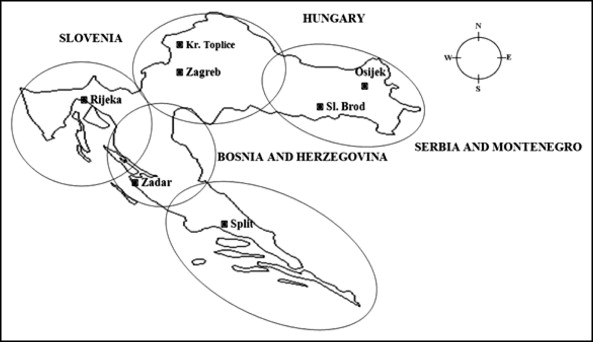
Having recognized these problems related to treating acute STEMI in Croatia, and knowing the world trends and recommendations, in the middle of 2005, the Croatian Cardiac Society introduced the Croatian Primary Percutaneous Coronary Intervention (PCI) Network into the healthcare system of the Republic of Croatia. The main goal was to achieve equal quality treatment of acute STEMI in all parts of Croatia. At present, 8 high-volume PCI centers throughout Croatia are included in this network and cover about 75% of the population ( Figure 1 ).
The main goals of the present investigation were to (1) evaluate the treatment results of the patients with acute STEMI treated with primary PCI in the Croatian Primary PCI Network; (2) compare these results with those from published randomized studies and registries; and (3) prove the equality of the treatment results for all Croatian primary PCI network patients, even those at greater risk (i.e., older patients, women, and patients with cardiogenic shock). The main hypothesis was that a well-organized primary PCI network, even in an economically less-developed country, could equalize the prospects of all patients with STEMI throughout the country at a level comparable to that in more economically developed countries.
Methods
The present investigation prospectively studied 1,190 consecutive patients with acute STEMI treated from September 1, 2005 to March 1, 2007 with primary PCI at 8 PCI centers throughout Croatia (4 with and 4 without on-site cardiac surgery capabilities) included in the Croatian Primary PCI Network. In 677 investigated patients, acute STEMI was diagnosed in one of the centers with an on-site PCI laboratory (catheterization laboratory), where primary PCI was performed (nontransferred patients). In the remaining 513 patients, acute STEMI was diagnosed in the hospitals without an on-site catheterization laboratory, and they were urgently transferred by ambulance to 1 of the 4 PCI centers for primary PCI (transferred patients). The diagnosis of STEMI was established and primary PCI performed using the criteria of the European Cardiac Society. In brief, patients with an episode of chest discomfort within the previous 12 hours and ST-segment elevation on the electrocardiogram in ≥2 consecutive leads were included. Immediately after the diagnosis, the patients waiting for transfer (transferred patients) or primary PCI (nontransferred patients) received a loading dose of 300 mg salicylic acid, 600 mg clopidogrel. During the procedure, they received 70 to 100 IE/kg of unfractionated heparin and, according to judgment of interventional cardiologist, a glycoprotein IIb/IIIa inhibitor.
After primary PCI, the patients were hospitalized an average of 2 to 3 days in the coronary care unit in the PCI centers with continuous monitoring and treatment. Afterward, they finished their hospital treatment in the cardiac departments of those hospitals (nontransferred patients) or were transferred back to their county hospitals (transferred patients). During their first hospital stay, general information (name, age, and gender) and data on the time of the first symptoms, time of arrival in the first hospital and/or PCI center, time of the first balloon insufflation during primary PCI, affected myocardial wall and coronary artery, postprocedural flow, and, eventually, cardiogenic shock and lethal outcome were collected. At 6 months after discharge, data on major adverse cardiovascular events (pectoral angina, restenosis, reinfarction, mortality, coronary artery bypass graft surgery, and cerebrovascular accidents) were collected for the investigated patients during their examination by checking the medical documentation or by telephone interview with the patients, their family members, or home physicians. Including the follow-up period, the present investigation occurred from September 1, 2005 to August 3, 2007.
Cardiogenic shock was defined as a clinical state of hypoperfusion characterized by a systolic blood pressure of <90 mm Hg and/or a capillary wedge pressure of >20 mm Hg and/or a cardiac index of <1.80 L/min/m 2 . The total ischemic time or symptom onset-to-balloon time was calculated as the interval between the first symptoms and balloon insufflation during primary PCI, the door-to-balloon time as the interval between the patient’s arrival in the first hospital (with or without an on-site catheterization laboratory) and balloon insufflation during primary PCI, and the symptom onset-to-door time as the interval between the first symptoms and arrival in the first hospital (with or without an on-site catheterization laboratory).
Postprocedural flow was classified according to the Thrombolysis In Myocardial Infarction (TIMI) grading system using a scale of 0 to 3.
Nominal (categorical) variables were analyzed using Pearson’s chi-square test and Fisher’s exact test. Quantitative variables were analyzed using the Mann-Whitney U test. Differences between subgroups with elimination of the influence of other variables were analyzed using multivariate log-linear analysis. The value of p <0.05 was considered statistically significant for all tests. Statistical analysis was performed using Statistica, version 6.0 (StatSoft, Tulsa, Oklahoma).
The investigation was performed in accordance with the ethical standards in the Declaration of Helsinki and was approved by the appropriate institutional review committees.
Results
The descriptive statistical data and intervals to reperfusion for all investigated patients, transferred and nontransferred, are listed in Table 1 , with the results of their treatment listed in Table 2 . No significant differences were found between the transferred and nontransferred patients in the investigated descriptive parameters. Also, the greater incidence of cardiogenic shock among nontransferred patients was insignificant. The average transfer distance for the subgroup of transferred patients was 72 km. The latter group of patients had longer door-to-balloon and symptom onset-to-balloon times, as expected because the transfer time was included in these 2 times to reperfusion. In the Croatian Primary PCI Network during the investigated period, 37% of all investigated patients received primary PCI within the recommended 90 minutes after arrival at the first hospital. For the nontransferred patients, this percentage was 47% and for the transferred patients was 25%. The transferred patients in the present investigation showed a trend toward better treatment results than the nontransferred patients, but the difference was not statistically significant at the multivariate level. During primary PCI, 93% of patients received stents. The follow-up rate was 89%.
| Variable | All Patients | Transferred Patients | Nontransferred Patients | p Value |
|---|---|---|---|---|
| Age (years) | 0.08 ⁎ | |||
| Median | 60 | 59 | 60 | |
| Range | 24–95 | 29–95 | 24–92 | |
| Gender | 0.15 † | |||
| Male | 73.3% | 75.7% | 71.7% | |
| Female | 26.7% | 24.5% | 28.3% | |
| Myocardial wall infarct | 0.12 † | |||
| Anterior | 42.6% | 39.8% | 44.8% | |
| Inferior | 57.4% | 60.2% | 55.2% | |
| Coronary artery | 0.27 † | |||
| Left anterior descending artery | 41.7% | 40.6% | 42.5% | |
| Circumflex coronary artery | 13.8% | 15.6% | 12.3% | |
| Right coronary artery | 43.4% | 42.7% | 44.0% | |
| Left main artery | 0.7% | 0.4% | 1.0% | |
| Bypass graft | 0.5% | 0.7% | 0.2% | |
| Cardiogenic shock | 6.7% | 5.5% | 7.6% | 0.19 † |
| Symptom onset-to-door time (min) | 0.45 ⁎ | |||
| Median | 130 | 135 | 130 | |
| Range | 15–1,365 | 15–1,230 | 15–1,365 | |
| Door-to-balloon time (min) | <0.01 ⁎ | |||
| Median | 108 | 123 | 96 | |
| Range | 10–540 | 35–540 | 10–465 | |
| Symptom onset-to-balloon time (min) | <0.01 ⁎ | |||
| Median | 265 | 298 | 255 | |
| Range | 45–702 | 84–702 | 45–695 |
⁎ Mann-Whitney U test (transferred vs nontransferred patients).
| Variable | All Patients | Transferred Patients | Nontransferred Patients | p Value ⁎ | |
|---|---|---|---|---|---|
| Chi-Square Test | Multivariate Log-Linear Analysis | ||||
| Postprocedural Thrombolysis In Myocardial Infarction 3 flow | 87.1% | 89.9% | 85.2% | 0.03 | 0.05 |
| Mortality rate | |||||
| In-hospital | 4.4% | 2.9% | 5.4% | 0.04 | 0.20 |
| At 6-month follow-up | 1.2% | 0.5% | 1.7% | 0.24 | 0.82 |
| Pectoral angina (6-month follow-up) | 12.1% | 11.4% | 12.6% | 0.70 | 0.13 |
| MACE, other (6-month follow-up) | 6.4% | 5.8% | 7.1% | 0.59 | 0.08 |
The descriptive statistical data and intervals to reperfusion for the subgroups of patients >75 years, women, and those in cardiogenic shock are listed in Table 3 and their results in Table 4 . Compared to all investigated patients, the subgroup of those >75 years old had a greater percentage of patients with cardiogenic shock, especially in the nontransferred group, and their intervals to reperfusion were longer. No significant differences were found in the results of treatment between the transferred and nontransferred older patients; however, the results for both subgroups were worse than those for all investigated patients. Compared to the results for all investigated patients, the female patients were older, with longer intervals to reperfusion, and somewhat worse treatment results. Patients with cardiogenic shock were, on average, older with the culprit lesion more frequently at the left main level than for all investigated patients. The results of their treatment and their prognosis were more serious than those of patients without this complication.
| Variable | Age >75 Years | Women | Cardiogenic Shock | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Transferred Patients | Nontransferred Patients | p Value | Transferred Patients | Nontransferred Patients | p Value | Transferred Patients | Nontransferred Patients | p Value | |
| Age (years) | |||||||||
| Median | — | — | — | 66 | 67 | 0.07 ⁎ | 65 | 70 | 0.25 † |
| Range | 29–92 | 24–89 | 52–81 | 40–89 | |||||
| Gender | |||||||||
| Male | 66.0% | 53.0% | <0.01 ⁎ | — | — | — | 75.0% | 66.7% | 0.67 ⁎ |
| Female | 34.0% | 47.0% | 25.0% | 33.3% | |||||
| Myocardial wall infarct | |||||||||
| Anterior | 37.2% | 43.6% | 0.05 ⁎ | 35.5% | 45.4% | 0.14 ⁎ | 50.0% | 40.0% | 0.60 ⁎ |
| Inferior | 62.8% | 56.4% | 64.5% | 54.6% | 50.0% | 60.0% | |||
| Coronary artery | |||||||||
| Left anterior descending artery | 37.3% | 45.1% | 0.37 ⁎ | 38.2% | 41.7% | 0.47 ⁎ | 45.8% | 27.5% | 0.32 ⁎ |
| Circumflex coronary artery | 7.7% | 11.3% | 15.2% | 10.6% | 16.7% | 12.5% | |||
| Right coronary artery | 51.0% | 38.0% | 45.7% | 45.9% | 33.3% | 47.5% | |||
| Left main artery | 2.0% | 5.6% | 0.9% | 1.2% | 4.2% | 12.5% | |||
| Bypass graft | 2.0% | 0 | 0 | 0.6% | 0 | 0 | |||
| Cardiogenic shock | 15.9% | 22.6% | 0.40 ⁎ | 5.8% | 8.9% | 0.48 ⁎ | — | — | — |
| Symptom onset-to-door time (minutes) | |||||||||
| Median | 171 | 155 | 0.27 † | 171 | 150 | 0.71 † | 120 | 180 | 0.07 † |
| Range | 30–1,230 | 15–1,080 | 20–1,230 | 30–1,080 | 45–780 | 25–1,080 | |||
| Door-to-balloon time (minutes) | |||||||||
| Median | 162 | 110 | 0.02 † | 130 | 100 | <0.01 † | 125 | 95 | 0.18 † |
| Range | 23–540 | 10–330 | 28–501 | 10–355 | 40–240 | 35–285 | |||
| Symptom onset-to-balloon time (minutes) | |||||||||
| Median | 348 | 283 | <0.01 † | 318 | 270 | <0.01 † | 230 | 255 | 0.77 † |
| Range | 120–650 | 45–570 | 84–690 | 60–660 | 145–650 | 105–510 | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


