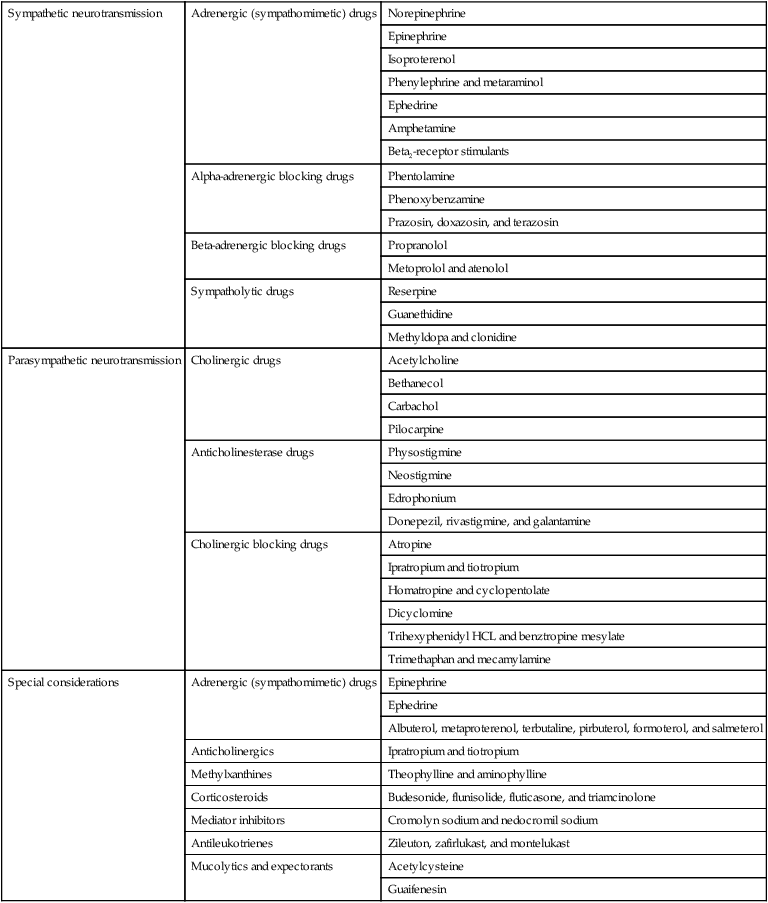
This chapter describes much of the basic respiratory and cardiovascular physiology that underlies the action of the drugs presented, with the goal of elucidating the relationship between basic physiology and the drug mechanism of action (Table 45-1). Some of the trade names of the medications mentioned in the text will be changing, but the generic names will remain the same. Not all pharmacological interventions for the respiratory and cardiovascular systems are covered. Certainly, no attempt has been made to describe the pharmacology of other systems or disease states. For further study, any of the texts listed in the reference section at the end of the chapter are highly recommended. Table 45-1 Respiratory and Cardiovascular Drugs This expression, cardiac output, is a common one, and it constitutes half of the blood pressure regulation equation: CO × TPR = BP, where CO is cardiac output, TPR is total peripheral resistance, and BP is blood pressure. TPR is determined by vasoconstriction or vasodilation in the arterioles. For example, vasoconstriction increases resistance; therefore TPR and BP go up. As mentioned above, there are several drugs that act primarily at the beta2 smooth muscle receptor site, causing selective actions in the bronchioles and arterioles but not in the heart (Box 45-1). These drugs will produce a bronchodilation without increasing cardiac output. This particular lack of cardiovascular effect makes them safer than drugs like isoproterenol or ephedrine in treatment of bronchial asthma. This class of drugs is currently part of the mainstay of treatment for asthma and chronic obstructive pulmonary disease (COPD).
Respiratory and Cardiovascular Drug Actions
Sympathetic neurotransmission
Adrenergic (sympathomimetic) drugs
Norepinephrine
Epinephrine
Isoproterenol
Phenylephrine and metaraminol
Ephedrine
Amphetamine
Beta2-receptor stimulants
Alpha-adrenergic blocking drugs
Phentolamine
Phenoxybenzamine
Prazosin, doxazosin, and terazosin
Beta-adrenergic blocking drugs
Propranolol
Metoprolol and atenolol
Sympatholytic drugs
Reserpine
Guanethidine
Methyldopa and clonidine
Parasympathetic neurotransmission
Cholinergic drugs
Acetylcholine
Bethanecol
Carbachol
Pilocarpine
Anticholinesterase drugs
Physostigmine
Neostigmine
Edrophonium
Donepezil, rivastigmine, and galantamine
Cholinergic blocking drugs
Atropine
Ipratropium and tiotropium
Homatropine and cyclopentolate
Dicyclomine
Trihexyphenidyl HCL and benztropine mesylate
Trimethaphan and mecamylamine
Special considerations
Adrenergic (sympathomimetic) drugs
Epinephrine
Ephedrine
Albuterol, metaproterenol, terbutaline, pirbuterol, formoterol, and salmeterol
Anticholinergics
Ipratropium and tiotropium
Methylxanthines
Theophylline and aminophylline
Corticosteroids
Budesonide, flunisolide, fluticasone, and triamcinolone
Mediator inhibitors
Cromolyn sodium and nedocromil sodium
Antileukotrienes
Zileuton, zafirlukast, and montelukast
Mucolytics and expectorants
Acetylcysteine
Guaifenesin
Sympathetic Neurotransmission

Adrenergic (Sympathomimetic) Drugs
Norepinephrine
Beta2-Receptor Stimulants
Respiratory and Cardiovascular Drug Actions











