Repair of Penetrating and Blunt Cardiac Trauma
Chad N. Stasik
John H. Calhoon
Traumatic cardiac injuries occur during both penetrating and blunt trauma. The focus of this chapter is those injuries requiring operative repair. The primary survey and initial resuscitation is performed according to Advanced Trauma Life Support (ATLS) protocols.
Penetrating Cardiac Injury
Penetrating cardiac injury is highly lethal. It is estimated that 80% to 90% of patients sustaining gunshot wounds (GSWs) to the heart die before hospital arrival. Most GSWs to the heart result in exsanguination, whereas cardiac stab wounds are more likely to cause tamponade. Bedside ultrasonography (the cardiac portion of the focused assessment with sonography in trauma [FAST] examination) by a trained operator has a sensitivity approaching 100% and specificity of greater than 97% for detecting fluid in the pericardial space. The FAST examination has supplanted subxiphoid pericardial exploration as the diagnostic test of choice for traumatic cardiac injury. The presence of hemopericardium in a patient with penetrating chest trauma who arrives to the hospital alive is an indication for surgical exploration and repair.
Patients who present without signs of life after having undergone cardiopulmonary resuscitation in the field have almost no chance of survival and the decision to perform resuscitative thoracotomy requires careful consideration. That being said, while the overall survival rate for resuscitative thoracotomy for trauma is as low as 2%, survival is the best following penetrating chest trauma and may approach 30% in this group when vital signs are lost in the resuscitation bay or during a brief transport period.
Blunt Cardiac Injury
Blunt cardiac injuries range in severity from insignificant myocardial contusion to rupture of the pericardium or a cardiac chamber resulting in tamponade or exsanguination.
Blunt cardiac injury is most commonly caused by motor vehicle crashes, followed by pedestrians struck by motor vehicles, and then falls. An unstable patient with a positive cardiac portion of the FAST examination following blunt chest trauma should be immediately transferred to the operating room for repair. The success rate for resuscitative thoracotomy following blunt trauma is almost nil and as such it should be reserved for patients who lose vital signs in the trauma bay. Pericardiocentesis for trauma probably results in more injuries than it diagnoses or temporizes, and for that reason it generally should not be performed in the acutely injured patient.
Blunt cardiac injury is most commonly caused by motor vehicle crashes, followed by pedestrians struck by motor vehicles, and then falls. An unstable patient with a positive cardiac portion of the FAST examination following blunt chest trauma should be immediately transferred to the operating room for repair. The success rate for resuscitative thoracotomy following blunt trauma is almost nil and as such it should be reserved for patients who lose vital signs in the trauma bay. Pericardiocentesis for trauma probably results in more injuries than it diagnoses or temporizes, and for that reason it generally should not be performed in the acutely injured patient.
The induction of general anesthesia results in a loss of sympathetic tone and causes vasodilation that can lead to hemodynamic collapse in a patient with any amount of hemopericardium. The surgeon and entire surgical team must be prepared for this, and the patient should be prepped and draped prior to the induction of anesthesia. In patients already exhibiting signs of tamponade, a subxiphoid pericardial window can be performed under local anesthesia to relieve the tamponade, after which time general anesthesia can more safely be induced.
Transesophageal echocardiography (TEE) is not necessary preoperatively, but a probe may be placed by an experienced anesthesiologist once the tamponade is addressed and bleeding controlled, to evaluate for valvular injuries, intracardiac shunts, or retained intracardiac missiles. While most cardiac trauma cases can be completed without pump support, there are rare occasions in which cardiopulmonary bypass (CPB) may be needed, such as in a coronary artery bypass graft (CABG) operation for a transected proximal left anterior descending (LAD) artery or to repair a torn left atrium (LA) at the pulmonary vein confluence. For these select scenarios, perfusion support should be available, and is required in all level I trauma centers. However, even when a valvular injury or septal defect is discovered on intraoperative TEE, delayed repair may be preferred in the absence of hemodynamic collapse mandating immediate operative intervention. In fact, some penetrating septal injuries, predominantly from stab wounds, will close spontaneously over time.
Other practical considerations are to ensure the presence of a functioning sternal saw with either a battery pack or working air supply, sternotomy and thoracotomy retractors and instrument sets, internal defibrillator paddles, and type-specific or O negative blood and products from the blood bank.
Positioning
The patient is positioned supine and prepped and draped from the chin to the knees and down to the table bilaterally. General anesthesia is induced and a standard single lumen endotracheal tube is placed.
Technique
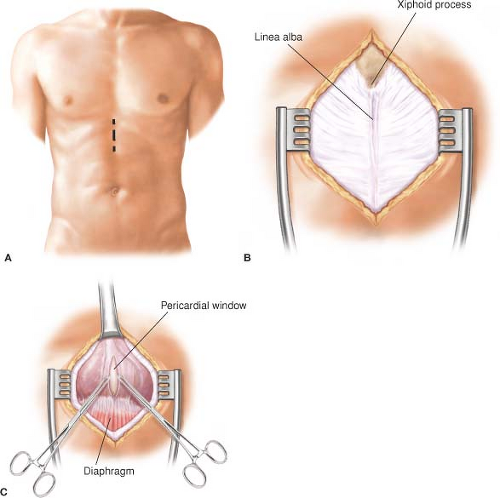
Once the diagnosis of traumatic hemopericardium (penetrating or blunt) has been made, median sternotomy is the incision of choice. If a resuscitative thoracotomy has already been performed through the left anterior fourth or fifth intercostal space it can be extended transversely across the sternum with heavy scissors or a saw, if necessary. If the diagnosis is still in question, a subxiphoid pericardial exploration can be performed and converted to a sternotomy if hemopericardium is identified (Fig. 23.1). A 6- to 8-cm midline incision is made extending over the xiphoid process onto the upper abdomen. The linea alba is divided and the xiphoid process is retracted or excised. Blunt dissection
is carried into the retrosternal space and the pericardium is identified. The pericardium is grasped between Allis clamps and incised. If blood or clot is present, it is evacuated and median sternotomy is performed.
is carried into the retrosternal space and the pericardium is identified. The pericardium is grasped between Allis clamps and incised. If blood or clot is present, it is evacuated and median sternotomy is performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree