47 Renal Artery Stenosis
Etiology and Pathogenesis
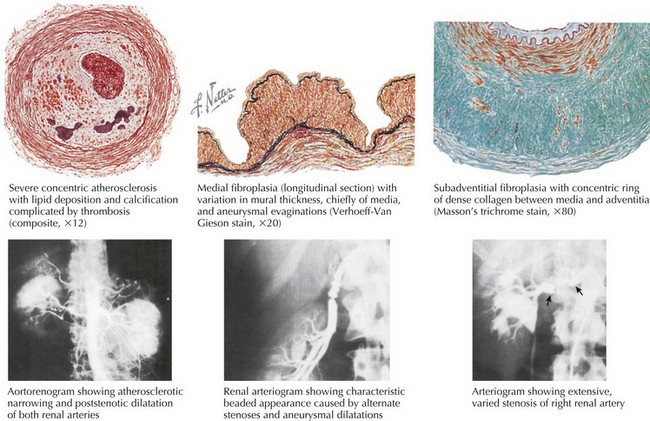
The predominant cause of obstructive RAS is atherosclerosis (Fig. 47-1). The atherosclerotic process can involve the renal artery or the aorta, with disease of the latter affecting the ostium of the renal artery. Rarely, obstructive RAS is caused by fibromuscular dysplasia (FMD; <10% of cases of RAS).
FMD is a collection of vascular diseases characterized by intimal or medial hyperplasia. It is commonly bilateral and affects women more often than men. The middle and distal portions of the vessel are the most commonly involved sites, with a typical angiographic appearance of “beads on a string” (see Fig. 47-1). FMD can cause hypertension but rarely leads to major loss of renal function, although progressive renal impairment has been described in smokers with FMD.
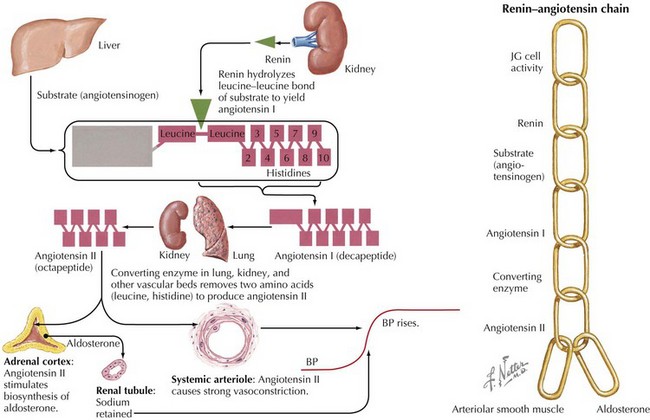
Regardless of its underlying pathologic cause, decreased renal perfusion results in compensatory activation of the renin-angiotensin system (Fig. 47-2), which can cause systemic hypertension, salt retention, and activation of the neurohormonal system. RAS also causes ischemic changes within the kidney (ischemic nephropathy) and increased systemic markers of oxidative stress. Other pathologic effects have been postulated but not proven to result from RAS.
Clinical Presentation
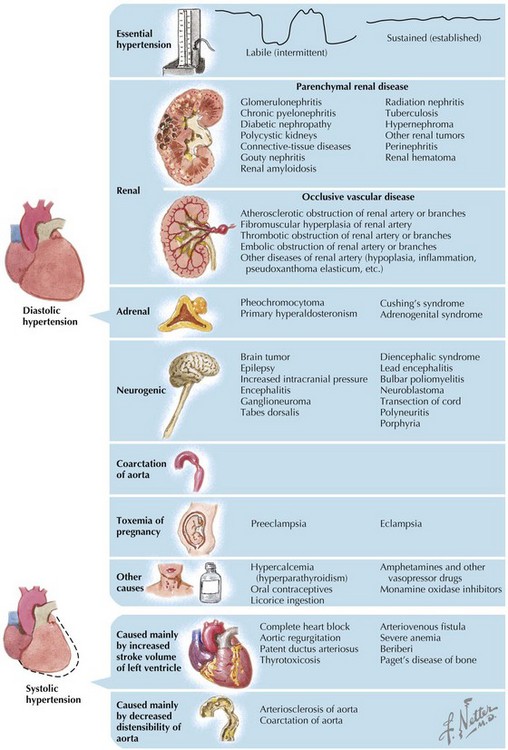
The vast majority of patients with hypertension have essential hypertension. Overall, renovascular disease is the etiology in 0.5% to 2% of patients with hypertension (Fig. 47-3), but it is more common in patients who present with new-onset, severe hypertension. RAS is more common in white than in black individuals, and the prevalence increases with age. Clinical factors that increase the likelihood of RAS include age, recent onset or sudden worsening of hypertension, and the presence of an abdominal bruit. The prevalence of RAS is also higher in patients with atherosclerosis in other vascular beds. Hemodynamically significant RAS is found in 6% to 23% of patients with hypertension who are undergoing cardiac catheterization. Significant RAS has been found in 10.4% of patients at autopsy after a cerebrovascular accident.
Differential Diagnosis
The primary entity in the differential diagnosis is essential hypertension (Chapter 46), although several other less common causes of hypertension must also be considered (see Fig. 47-3). The point at which renal artery atherosclerosis becomes physiologically significant and leads to increased BP and ischemic nephropathy is incompletely understood. Recognition of lesions that compromise blood flow to the kidney is essential to identify patients whose conditions will improve with renal revascularization. This is especially important, because there is also a high rate of essential hypertension in patients with RAS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree