Knowledge of the role of the soluble receptor for advanced glycation end products (sRAGEs) in chronic heart failure (CHF) is very limited. In the present study, we measured plasma sRAGE levels in patients with CHF and examined whether plasma sRAGE predicts prognosis in patients with HF independently of validated scores as the Seattle Heart Failure Score (SHFS). We measured plasma sRAGE in 106 outpatients with CHF. Patients were prospectively followed during a median follow-up period of 1.3 years with end points of cardiac death or rehospitalization. Plasma sRAGE level increased with advancing New York Heart Association functional class, SHFS, age, and ischemic cause. Plasma sRAGE level was also higher in patients with cardiac death and/or events than in event-free patients. In Cox multivariate proportional hazard analysis, SHFS, sRAGE, and N-terminal pro–B-type natriuretic peptide were independent risk factors for cardiac death (sRAGE hazard ratio 1.26, 95% confidence interval 1.09 to 1.45, p = 0.002) and/or cardiac events (sRAGE hazard ratio 1.07, 95% confidence interval 1.03 to 1.11, p = 0.002). Survival curves adjusted by Cox analysis clearly demonstrated that the high-sRAGE group (higher than median) had a significantly higher incidence of cardiac death than the low-sRAGE group (p = 0.001). In conclusion, sRAGE is a novel, highly sensitive, and specific prognostic marker in current optimally treated patients with CHF with an additive and independent value compared to the multimarker SHFS.
Advanced glycation end products (AGEs) are molecules that appear in plasma and tissues and are generated by nonenzymatic glycation and oxidation of proteins because of the Maillard reaction, which is driven by oxidative stress in its final step. In the setting of chronic heart failure (CHF), excess free-radical generation leads to increased plasma levels of AGEs. There is accumulating evidence that an interaction of AGEs with their receptor (RAGE) causes activation of intracellular signaling, gene expression, and production of proinflammatory cytokines and free radicals, thus playing a central role in the pathogenesis of vascular and heart complications. Biological function of the soluble form of RAGE (sRAGE) has not been clearly defined and its biological importance within the AGE-RAGE axis is only recently beginning to be understood. In the present study, we sought to evaluate the relation of sRAGE to severity and prognosis of CHF and to analyze whether this parameter has an additional value in predicting outcomes compared to the widely accepted Seattle Heart Failure Score (SHFS). SHFS is a model used to predict CHF prognosis in outpatients that uses common CHF clinical risk predictors and incorporates the effects of medical therapy and device interventions. However, the model does not incorporate certain HF prognostic parameters such as renal function, B-type natriuretic peptide levels (BNP), and other biomarkers.
Methods
One hundred six consecutive outpatients with stable CHF who visited our hospital (cardiology department of University Hospital of Santiago de Compostela) from September 2008 through March 2009 were entered in this prospective study. Causes of CHF were identified as hypertensive in 34%, ischemic in 33%, valvular in 9%, and other in 24%. Diagnosis of CHF was based on clinic symptoms and signs and evidence of structural and/or functional cardiac abnormalities (according to diagnostic criteria of the European Society of Cardiology ). All patients had been in a stable clinical state for ≥2 months before study entry. Patients with known tumoral disease, hematologic disorders, history of clinically relevant infection within 90 days, or acute and chronic inflammatory diseases involving organs other than the heart were excluded from analysis. We did not include patients undergoing long-term treatment with steroid or nonsteroid anti-inflammatory drugs. The entire study was planned according to ethical standards detailed in the Declaration of Helsinki and was approved by the ethics committee for human studies at Galicia (Spanish region).
Collection of medical history, cigarette smoking status, and current use of medication were recorded from questionnaires and interviews. Weight and height were measured while wearing indoor clothing without shoes and body mass index was calculated. Blood pressure was measured 2 times in a supine position after a 10-minute rest with a random 0 sphygmomanometer. During this visit, a cardiac transthoracic ultrasound study was done to determine left ventricular ejection fraction (LVEF). LVEF was measured by echocardiography using the biplane disk summation method (Simpson rule). LVEF was considered preserved when it was >45%.
Peripheral venous blood was collected from 8 through 10 a . m . after an overnight fast. Blood samples were centrifuged at 2,000 g for 10 minutes at room temperature, and serum or plasma samples were frozen at −40°C until assayed. Basic biochemical tests were performed with a Cobas Integra model 700 multichannel analyzer (Roche Diagnostics, Indianapolis, Indiana). Estimated glomerular filtration rate was used as an indicator of renal function based on the abbreviated Modification of Diet in Renal Disease study formula. Serum lipid levels were measured by enzymatic colorimetric test (Boehringer Ingelheim, Mannheim, Germany) and low-density lipoprotein cholesterol was calculated from the Friedewald formula. Hemoglobin A 1c was measured by a latex-enhanced turbidimetric immunoassay (Cobas Integra System, Roche Diagnostics, Mannheim, Germany). Plasma levels of N-terminal pro-BNP (NT–pro-BNP) were measured using the Elecsys pro-BNP sandwich enzyme-linked immunosorbent assay (Roche Diagnostics, Madrid, Spain). Plasma sRAGE levels were determined using a commercially available enzyme-linked immunosorbent assay kit (Quantikine, R&D Systems, Minneapolis, Minnesota) according to the manufacturer’s protocol. Measurements were performed in duplicate and results were averaged. Intra-assay and interassay coefficients of variation were <5% and <8%, respectively. AGEs were measured by fluorescence of plasma according to the method of Munch et al. Plasma was aliquoted into black 96-well plates in duplicate and fluorescence (excitation 360/40 nm, emission 460/40 nm) measured in a multimode microplate reader (Synergy 2, Bio-Tek, Bad Friedrichshall, Germany) at room temperature to estimate levels of fluorescent AGE. Readings were subtracted from those of plasma-free wells to obtain measurements in arbitrary units and the mean of each pair of readings was calculated.
SHFS was derived for all patients based on original risk factor coefficients as described by Levy et al. Mean life expectancy was derived using the Web-based SHFS tool ( http://depts.washington.edu/shfm ).
All patients were monthly consulted in our hospital to assess adherence to medication. Follow-up data were based on patients’ records available at our outpatient clinic. None of the patients were lost to follow-up. Median follow-up of event-free patients was 1.3 years (1.1 to 1.4 SD, range 1.0 to 1.7). End points were death and rehospitalization with worsening HF. We defined cardiac events as a combination of these end points.
All analyses were performed with SPSS 15.0 for Windows (SPSS, Inc., Chicago, Illinois). Continuous variables were expressed as mean ± SD. Categorical variables were presented as count or proportion (percentage). Comparisons of continuous variables between 2 different groups were performed with Student’s t test. Continuous data from >2 groups were compared with 1-way analysis of variance. Pearson chi-square test was used for comparing categorical variables. To study the correlation between quantitative variables, Pearson or Spearman test was used. To calculate the sensitivity and specificity for sRAGE cut-off values to predict mortality and/or cardiac events, a receiver operator characteristic curve was configured. Cox proportional hazard analysis was performed to determine the independent predictor of cardiac events for the entire population. All variables that showed a p value <0.10 in univariate Cox regression analysis were entered into multivariate Cox regression analysis, as were entered other variables with demonstrated clinical value. SHFS was expressed as percent mortality risk, NT–pro-BNP per 100 pg/ml, fluorescent AGE per arbitrary unit, and sRAGE per 100 pg/ml. Adjusted survival curves for these variables for groups with high and low levels of sRAGE (based on median of sRAGE) were shown to indicate the independent prognostic value of this parameter. A p value <0.05 was considered statistically significant.
Results
Baseline characteristics are presented in Table 1 . There was no difference in gender, body mass index, presence of diabetes mellitus or hypertension, and decreased LVEF between groups without and with cardiac events. Mean values for age, SHFS, NT–pro-BNP, fluorescent AGE, and sRAGE were significantly higher in patients with cardiac events. The opposite was found for hemoglobin. Percent kidney failure and ischemic cause were higher in the group with cardiac events. Concerning therapy, the group with cardiac events received more treatment with diuretics without other significant differences between groups.
| Characteristics | Total (n = 106) | Survivors (n = 95, 89.6%) | Nonsurvivors (n = 11, 10.4%) | p Value | Without Cardiac Event (n = 77, 72.6%) | With Cardiac Event (n = 29, 27.4%) | p Value |
|---|---|---|---|---|---|---|---|
| Age (years) | 72.0 (63.0–78.5) | 69.6 ± 11.7 | 74.2 ± 9.8 | 0.233 | 68.0 ± 12.2 | 75.5 ± 7.4 | 0.001 |
| Women | 32.7% | 34.0% | 20.0% | 0.368 | 33.8% | 29.6% | 0.693 |
| Hypertension ⁎ | 53.6% | 57.6% | 60.0% | 0.884 | 53.3% | 70.4% | 0.124 |
| Dyslipidemia † | 48.2% | 52.7% | 50.0% | 0.869 | 50.0% | 59.3% | 0.419 |
| Diabetes mellitus | 35.8% | 35.8% | 36.4% | 0.970 | 33.8% | 41.4% | 0.466 |
| New York Heart Association classes III to IV | 22.2% | 21.3% | 30.0% | 0.533 | 19.2% | 30.8% | 0.222 |
| Ischemic cause | 32.0% | 30.1% | 50.0% | 0.200 | 25.0% | 51.9% | 0.010 |
| Body mass index (kg/m 2 ) | 28.2 ± 4.4 | 28.4 ± 4.3 | 25.8 ± 4.4 | 0.202 | 28.5 ± 4.2 | 27.7 ± 4.7 | 0.678 |
| Decreased left ventricular ejection fraction | 61.9% | 63.6% | 44.4% | 0.259 | 63.9% | 56.0% | 0.484 |
| Estimated glomerular filtration rate <60 ml/min | 37.9% | 37.6% | 40.0% | 0.883 | 30.3% | 59.3% | 0.008 |
| Hemoglobin (g/dl) | 13.1 ± 1.6 | 13.2 ± 1.5 | 11.7 ± 1.9 | 0.003 | 13.4 ± 1.5 | 12.4 ± 1.8 | 0.007 |
| High-density lipoprotein (mg/dl) | 42.9 ± 17.8 | 43.9 ± 18.3 | 33.3 ± 8.5 | 0.091 | 45.0 ± 19.3 | 36.9 ± 11.3 | 0.139 |
| Low-density lipoprotein (mg/dl) | 110.2 ± 35.4 | 112.3 ± 34.2 | 87.8 ± 41.5 | 0.061 | 113.3 ± 31.1 | 100.4 ± 45.6 | 0.056 |
| Glucose (mg/dl) | 121.5 ± 43.4 | 122.6 ± 44.4 | 111.8 ± 33.0 | 0.458 | 118.6 ± 36.9 | 130.2 ± 58.9 | 0.254 |
| Glycated hemoglobin | 6.3 ± 1.3 | 6.3 ± 1.2 | 6.5 ± 2.1 | 0.709 | 6.2 ± 1.1 | 6.6 ± 1.6 | 0.146 |
| Fluorescent advanced glycation end products (AU) | 67.3 ± 22.6 | 66.3 ± 21.4 | 76.5 ± 30.8 | 0.156 | 62.3 ± 19.0 | 80.6 ± 26.2 | 0.001 |
| Soluble receptor for advanced glycation end products (pg/ml) | 1,229.1 ± 931.4 | 1,170.0 ± 909.6 | 1,739.2 ± 1,005.9 | 0.055 | 997.4 ± 766.2 | 1,844.1 ± 1,058.4 | 0.001 |
| Brain natriuretic peptide (pg/ml) | 2,669.8 ± 3,274.5 | 2,356.2 ± 3,139.0 | 5,609.7 ± 3,242.3 | 0.007 | 1,971.8 ± 2,944.1 | 5,020.9 ± 3,308.3 | 0.001 |
| Seattle Heart Failure Score | 7.3 ± 5.1 | 13.5 ± 10.7 | 6.6 ± 3.5 | 0.057 | 11.2 ± 7.6 | 5.8 ± 2.6 | 0.001 |
| Treatment | |||||||
| Angiotensin–aldosterone system blockers | 88.7% | 89.6% | 80.0% | 0.315 | 90.9% | 82.8% | 0.198 |
| β Blockers | 85.1% | 84.6% | 90.0% | 0.543 | 86.5% | 81.5% | 0.367 |
| Diuretics | 82.2% | 80.2% | 100.0% | 0.127 | 75.7% | 100.0% | 0.002 |
| Statins | 41.7% | 41.7% | 50.0% | 0.427 | 41.6% | 44.8% | 0.465 |
| Insulin | 10.4% | 10.4% | 10.0% | 0.723 | 7.8% | 17.2% | 0.144 |
⁎ Antihypertensive treatment or systolic/diastolic blood pressure ≥140/90 mm Hg.
† Antihyperlipidemic treatment or total cholesterol ≥220 mg/dl, triglyceride ≥150 mg/dl, or high-density lipoprotein <40 mg/dl.
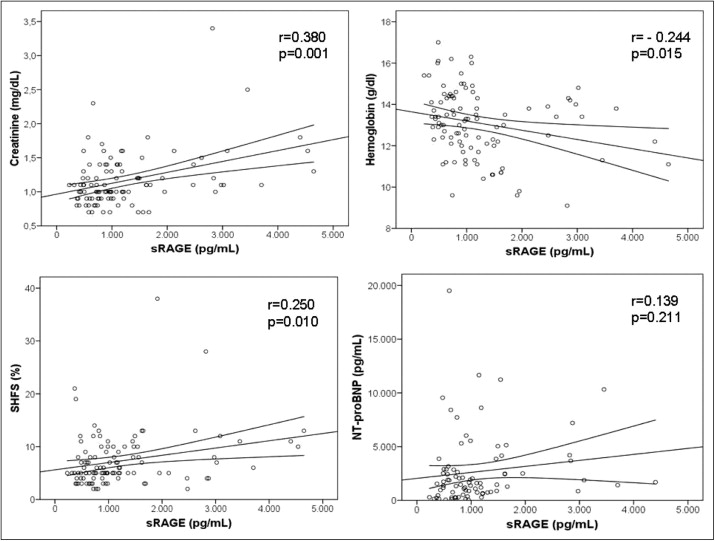
No difference existed in sRAGE levels between patients with and without diabetes mellitus, hypertension, and decreased LVEF. Plasma levels of fluorescent AGE were higher in patients with diabetes mellitus (70.4 ± 18.5 vs 58.3 ± 18.1 AU, p = 0.007) and kidney failure (79.2 ± 19.8 vs 54.8 ± 13.3 AU, p = 0.001). sRAGE levels were higher in patients with ischemic CHF (1,321.1 ± 1,105.2 vs 895.8 ± 596.5 pg/ml, p = 0.036) and kidney failure (1,545.2 ± 1,142.8 vs 1,039.5 ± 717.7 pg/ml, p = 0.014). sRAGE levels were also significantly higher in severe than in mild CHF (1,663.2 ± 1,135.9 vs 1,090.3 ± 770.6 pg/ml for New York Heart Association classes III to IV vs I to II, respectively, p = 0.007). A significant inverse correlation existed between plasma levels of AGE and sRAGE with hemoglobin and creatinine ( Figure 1 ). NT–pro-BNP correlated directly with fluorescent AGE (r = 0.226, p = 0.040) but not with sRAGE ( Figure 1 ). Fluorescent AGE and sRAGE showed a positive correlation (r = 0.283, p = 0.003).
During the follow-up period, 11 patients died and 18 were hospitalized because of worsening CHF. Plasma levels of fluorescent AGE and sRAGE were higher in nonsurvivors compared to survivors and in the group with cardiac events compared to the group without cardiac events ( Table 1 ).
High levels of plasma sRAGE but not of fluorescent AGE (defined as higher than the median) were associated with a higher rate of mortality and rehospitalization because of worsening CHF in patients with stable CHF ( Table 2 ). By univariate analysis, hemoglobin, high-density lipoprotein cholesterol, NT–pro-BNP, and sRAGE were significant predictors of mortality. Backward stepwise multivariate analysis showed that SHFS, NT–pro-BNP, and sRAGE were significant independent predictors for mortality ( Figure 2 ). Model discrimination was assessed by a receiver operator characteristic curve and the c statistic was 0.88 (0.79 to 0.96). In relation to cardiac events in aggregate, in univariate analysis the same variables as for mortality plus age (per decade), severe CHF, ischemic cause, kidney failure, and fluorescent AGE (per arbitrary unite) were significant predictors of morbidity/mortality. In stepwise multivariate analysis SHFS, NT–pro-BNP, and sRAGE remained significant ( Figure 2 ). Neither serum creatinine nor estimated glomerular filtration rate reached statistical significance for morbidity and mortality in multivariate analysis.
| Characteristics | High sRAGE | Low sRAGE | p Value |
|---|---|---|---|
| Age (years) | 72.6 ± 9.6 | 67.5 ± 12.8 | 0.023 |
| Women | 35.3% | 30.2% | 0.579 |
| Hypertension ⁎ | 56.9% | 58.8% | 0.841 |
| Dyslipidemia † | 58.0% | 47.1% | 0.271 |
| Diabetes mellitus | 36.5% | 35.2% | 0.885 |
| New York Heart Association classes III to IV | 32.7% | 12.0% | 0.013 |
| Ischemic cause | 43.1% | 21.2% | 0.017 |
| Body mass index (kg/m 2 ) | 27.7 ± 4.2 | 28.7 ± 4.5 | 0.341 |
| Depressed left ventricular ejection fraction | 57.4% | 66.0% | 0.386 |
| Estimated glomerular filtration rate <60 ml/min | 49.0% | 30.8% | 0.045 |
| Hemoglobin (g/dl) | 12.6 ± 1.6 | 13.6 ± 1.5 | 0.002 |
| High-density lipoprotein (mg/dl) | 40.2 ± 12.8 | 45.5 ± 21.5 | 0.152 |
| Low-density lipoprotein (mg/dl) | 109.8 ± 38.4 | 115.8 ± 31.9 | 0.921 |
| Glucose (mg/dl) | 127.6 ± 52.9 | 115.8 ± 31.9 | 0.178 |
| Glycated hemoglobin | 6.7 ± 1.5 | 5.9 ± 0.9 | 0.003 |
| Fluorescent advanced glycation end-products (AU) | 71.1 ± 23.2 | 63.7 ± 21.7 | 0.093 |
| Brain natriuretic peptide (pg/ml) | 3,097.9 ± 3,077.8 | 2,325.4 ± 3,418.9 | 0.288 |
| Seattle Heart Failure Score | 8.4 ± 5.9 | 6.2 ± 4.0 | 0.032 |
| Treatment | |||
| Angiotensin–aldosterone system blockers | 84.6% | 90.2% | 0.195 |
| β Blockers | 83.7% | 86.5% | 0.686 |
| Diuretics | 95.7% | 88.8% | 0.666 |
| Statins | 44.9% | 44.2% | 0.946 |
| Insulin | 17.6% | 3.8% | 0.024 |
| Death | 17.6% | 3.7% | 0.022 |
| Cardiac events | 44.2% | 11.1% | 0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


