Whether autonomic dysfunction predates the development of symptomatic heart failure (HF) or is simply a consequence of severe HF is unknown. We hypothesized that reduced heart rate variability (a marker of abnormal autonomic function) at baseline is associated with incident HF in subjects free of clinically recognized cardiovascular disease. In the Multi-Ethnic Study of Atherosclerosis (MESA), a population-based study of subclinical cardiovascular disease in adults aged 45 to 84 years, we measured the heart rate variability using a standard 30-second, 12-lead electrocardiogram to measure the standard deviation of normal-to-normal intervals (SDNN) and the root mean square of successive differences in RR intervals (RMSSD). During a median follow-up of 7.6 years, 95 participants developed HF (incidence rate 2.7/1,000 person-years). After adjusting for age, gender, and ethnicity, the hazard ratio for incident HF stratified by the RMSSD tertile was 2.4 (95% confidence interval 1.4 to 4.2) for the lowest tertile and 1.7 (95% confidence interval 1.0 to 3.2) for the middle tertile (highest tertile was the referent group; p for trend <0.001). The inverse association between the RMSSD and incident HF persisted after adjustment for additional covariates, including diabetes, systolic blood pressure, heart rate, subclinical atherosclerosis, left ventricular end-systolic volume, interim myocardial infarction, and high-sensitivity C-reactive protein (p for trend = 0.009). A similarly significant inverse association was also observed for SDNN. In conclusion, baseline autonomic dysfunction was a risk factor for the development of HF in a multiethnic cohort. These population-based findings implicate autonomic dysfunction in the pathogenesis of HF, and decreased short-term heart rate variability might be a novel form of stage B (asymptomatic) HF.
Abnormal functioning of the autonomic nervous system, as reflected by reduced heart rate variability (HRV), has been identified in a variety of chronic cardiovascular disease states, such as coronary artery disease, hypertension, and heart failure (HF). Although decreased HRV has been previously described in both asymptomatic left ventricular (LV) systolic dysfunction and symptomatic systolic HF, the relation between the HRV and incident HF has not been evaluated. Also, whether decreased HRV is a cause or a consequence of the HF syndrome is unknown. Subclinical abnormalities in cardiac structure and function might be associated with abnormal autonomic function through maladaptive neurohormonal activation. In addition, the risk factors for HF, such as diabetes mellitus and coronary artery disease, have also been associated with autonomic dysfunction. Finally, reduced HRV might be a sign of sympathetic activation, which can lead to increased sodium retention and thereby precipitate the HF syndrome in patients at risk. We therefore hypothesized that decreased short-term HRV would be associated with increased incident HF in those free of clinical cardiovascular disease. We tested this hypothesis in the Multi-Ethnic Study of Atherosclerosis (MESA), a large, population-based, multiethnic cohort of participants without known clinical cardiovascular disease.
Methods
The design of MESA has been previously described in detail. In brief, MESA was a multicenter, population-based, cohort study of 6 communities in the United States (Illinois, North Carolina, Maryland, California, New York, and Minnesota). The participants were recruited from July 2000 to August 2002. The participants defined themselves as white (38%), African-American (28%), Hispanic (22%), or Chinese American (12%). All MESA participants were free of clinical cardiovascular disease at baseline. The institutional review boards of all participating centers approved MESA, and all the participants gave written, informed consent. For the present analysis, we included 4,652 MESA participants who had undergone measurement of the root mean square of successive differences in RR intervals (RMSSD) and standard deviation of normal-to-normal intervals (SDNN), and cardiac magnetic resonance imaging and had follow-up data available.
The baseline short-term HRV was quantified similar to that in a previous study using time-domain analysis of 3 sequential 10-second electrocardiograms (recorded after 30 minutes of supine rest). Electrocardiograms were obtained using a Marquette MAC-1200 instrument (GE Medical Systems, Milwaukee, Wisconsin) and analyzed electronically by a central electrocardiographic reading center that was blinded to all clinical and nonelectrocardiographic data from the participants. From the 3 consecutive, 10-second electrocardiograms, after discarding ectopic beats, the time-domain HRV parameters, including the SDNN and RMSSD, were documented for each participant with available and interpretable electrocardiographic data. All HRV parameters were calculated using previously published guidelines.
A telephone interviewer contacted each participant (or their proxy) every 6 to 9 months to inquire about outpatient cardiovascular diagnoses, interim hospitalizations, and death. For each event, the medical records were obtained. Two MESA investigators independently reviewed all the records for the cardiovascular events. Incident HF, the primary outcome for the present study, was adjudicated by the MESA investigators using validated clinical criteria for symptomatic HF determined from the Cardiovascular Health Study and Women’s Health Initiative Study. The criteria for the diagnosis of incident HF required (1) physician-diagnosed, symptomatic HF, (2) medical treatment of HF, and (3) ≥1 of the following: pulmonary edema or pulmonary vascular congestion found on the chest radiograph, dilated LV or reduced LV systolic function on the echocardiogram or ventriculogram, and/or evidence of LV diastolic dysfunction.
In addition to undergoing HRV analysis and outcomes ascertainment, all participants underwent comprehensive baseline testing, including documentation of co-morbidities, measurement of blood pressure and heart rate, laboratory testing (fasting lipid profile, fasting glucose, and high-sensitivity C-reactive protein), computed tomography of the chest to determine the coronary artery calcium score, and cardiac magnetic resonance imaging to evaluate the LV size and function. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or current use of antihypertensive medications. Diabetes was defined as fasting glucose ≥126 mg/dl or the use of diabetic medications. Obesity was defined as a body mass index of ≥30 kg/m 2 . Physical activity was defined as the number of MET minutes per week spent doing intentional leisure time exercise (e.g., moderate walking exercise, dance, and vigorous sports).
Computed tomography scanning (for the coronary artery calcium score) and cardiac magnetic resonance imaging (for LV structure and function) in MESA have previously been described in detail. For the present study, we included data on the coronary artery calcium score as a marker of subclinical atherosclerosis at baseline. In addition, we included the following cardiac magnetic resonance parameters: LV mass, LV end-diastolic volume, LV end-systolic volume, LV ejection fraction, and stroke volume. Interim myocardial infarction was diagnosed by a combination of symptoms, electrocardiographic findings, and cardiac biomarker levels.
The correlation between RMSSD and SDNN was assessed using Pearson’s correlation coefficient. For descriptive purposes only, the participants were classified into RMSSD and SDNN groups using the tertiles of each HRV parameter within the entire cohort (RMSSD tertiles: low,<16 ms; middle; ≥16 but <27 ms; and high, ≥27 ms; and SDNN tertiles: low, <14.6 ms; middle, ≥14.6 but <24.3 ms; and high, ≥24.3 ms). The baseline characteristics were compared across the tertiles of RMSSD and SDNN with significance determined using chi-square tests for categorical variables or analysis of variance (or the Kruskal-Wallis test, when appropriate) for continuous variables. We further examined the associations between the baseline characteristics and HRV parameters modeled as continuous variables (instead of tertiles). Statistical significance was tested using linear regression analysis (continuous variables), Cochran-Armitage trend tests (dichotomous variables), or quantile regression analysis (nonparametric comparisons).
For all survival analyses, the follow-up interval was defined for each participant as the elapsed time between the baseline visit to the date of most recent follow-up point (MESA telephone follow-up 9), the date of death, or the date of incident HF. The median follow-up duration for the cohort was 7.6 years. Annualized incidence rates of HF per 1,000 person-years according to the tertiles of RMSSD or SDNN were calculated, with the number of cases of HF as the numerator and number of person-years as the denominator.
Cox proportional hazards models were used to investigate the association of incident HF and tertiles of RMSSD and SDNN separately, with the highest tertile as the reference group in 4 models: model 1, adjusted for age, gender, and ethnicity; model 2, all variables in model 1 plus education, physical activity, smoking status, diabetes, systolic blood pressure, presence of coronary artery calcium, LV end-systolic volume, and heart rate at rest; model 3, all variables in model 2 plus time-varying incident myocardial infarction (myocardial infarction occurring before or on the date of incident HF); and model 4, all variables in model 3 plus C-reactive protein. Linear trend across the tertiles was performed on the log-transformed RMSSD or SDNN as a continuous variable because of the highly skewed distribution. The proportionality assumption was confirmed for all Cox regression models.
Covariates were screened for inclusion into multivariate models if they were associated with the HRV parameters (either RMSSD or SDNN) in MESA or previously published studies of HRV. From this list, the covariates thought to be plausibly associated with both HRV and HF (using external clinical judgment) were chosen for inclusion in the multivariate models. Additional covariates were added if a previous association was known between the covariate and HF. Several covariates associated with the HRV parameters (e.g., cardiac magnetic resonance parameters) were collinear; therefore, only 1 of a group of collinear variables was selected for entry into the final multivariate models. All analyses were conducted using SAS statistical software, version 9.2 (SAS Institute, Cary, North Carolina). p Values <0.05 were considered statistically significant.
Results
Our study included 4,652 MESA participants (53.0% women; 38.7% white, 13.4% Chinese American, 25.2% African-American, and 22.7% Hispanic) with a mean age of 61.2 years at baseline. The 2 calculated HRV parameters (SDNN and RMSSD) correlated highly, with a Pearson correlation coefficient of 0.95 (p <0.001). The characteristics of the participants stratified by the RMSSD and SDNN tertiles are listed in Table 1 . The participants in the lowest tertile for both SDNN and RMSSD were older, more often men, and less likely African-American. In general, these participants were also more likely to be taking angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, calcium channel blockers, or antihypertensive or lipid-lowering medication.
| Variable | RMSSD Tertiles | p Value ∗ | SDNN Tertiles | p Value ∗ | ||||
|---|---|---|---|---|---|---|---|---|
| Low (1.0–15.9) | Middle (16.0–26.9) | High (27.0–328.0) | Low (0.90–14.5) | Middle (14.6–24.2) | High (24.3–208.1) | |||
| Patients (n) | 1,492 | 1,602 | 1,558 | 1,555 | 1,565 | 1,532 | ||
| Age (yrs) | ||||||||
| Mean ± SD | 64.1 ± 9.6 | 60.8 ± 9.8 | 59.0 ± 10.0 | <0.001 | 64.4 ± 9.7 | 60.4 ± 9.7 | 58.8 ± 10.0 | <0.001 |
| <65 yrs (%) | 49.4 | 61.9 | 68.2 | <0.001 | 47.1 | 63.3 | 69.7 | <0.001 |
| Male gender (%) | 50.4 | 47.9 | 42.9 | <0.001 | 48.0 | 49.3 | 43.7 | 0.005 |
| Race (%) | <0.001 | <0.001 | ||||||
| White | 41.9 | 39.9 | 34.5 | 38.8 | 39.7 | 37.6 | ||
| Chinese American | 16.3 | 14.7 | 9.2 | 16.9 | 14.2 | 8.9 | ||
| African-American | 18.3 | 22.8 | 34.2 | 19.4 | 23.5 | 32.8 | ||
| Hispanic | 23.5 | 22.6 | 22.1 | 24.8 | 22.6 | 20.7 | ||
| Education beyond high school (%) | 62.9 | 67.3 | 66.0 | 0.028 | 62.0 | 66.2 | 68.2 | 0.001 |
| BMI (kg/m 2 ) | 27.7 ± 4.8 | 27.5 ± 4.8 | 28.0 ± 5.1 | 0.022 | 27.6 ± 4.9 | 27.6 ± 4.9 | 28.0 ± 5.0 | 0.071 |
| BMI ≥30 kg/m 2 (%) | 27.1 | 27.4 | 30.5 | 0.071 | 26.9 | 27.7 | 30.5 | 0.059 |
| Cigarette smokers (%) | 10.3 | 11.9 | 15.5 | <0.001 | 10.5 | 12.5 | 14.8 | 0.001 |
| Physical activity (MET min/wk) | ||||||||
| Women | 0.027 | 0.026 | ||||||
| Median | 630 | 735 | 840 | 660 | 765 | 825 | ||
| IQR | 0–1,687 | 82–1,852 | 210–1,890 | 0–1,657 | 105–1,860 | 210–1,890 | ||
| Men | 0.123 | 0.043 | ||||||
| Median | 967 | 1,050 | 1,114 | 1,080 | 922 | 1,200 | ||
| IQR | 157–2,224 | 315–2,325 | 315–2,682 | 315–2,235 | 157–2,340 | 330–2,625 | ||
| Medication use (%) | ||||||||
| β Blocker | 8.4 | 7.6 | 9.1 | 0.311 | 9.3 | 8.1 | 7.8 | 0.283 |
| ACEI or ARB | 17.8 | 12.1 | 11.8 | <0.001 | 18.8 | 10.8 | 11.9 | <0.001 |
| Calcium channel blocker | 13.8 | 10.6 | 11.0 | 0.010 | 14.7 | 10.0 | 10.5 | <0.001 |
| Hypertension | 40.0 | 32.3 | 31.9 | <0.001 | 42.3 | 31.0 | 30.5 | <0.001 |
| Lipid altering | 18.2 | 16.1 | 13.3 | 0.001 | 18.5 | 15.7 | 13.2 | <0.001 |
| SBP (mm Hg) | 128.4 ± 20.8 | 124.6 ± 20.8 | 123.1 ± 21.6 | <0.001 | 128.7 ± 21.3 | 124.1 ± 20.4 | 123.1 ± 21.5 | <0.001 |
| DBP (mm Hg) | 73.0 ± 10.3 | 71.9 ± 10.1 | 70.8 ± 10.3 | <0.001 | 72.6 ± 10.3 | 71.8 ± 10.0 | 71.2 ± 10.4 | 0.001 |
| Hypertension (%) | 49.1 | 38.8 | 38.6 | <0.001 | 50.9 | 37.1 | 38.0 | <0.001 |
| Pulse pressure (mm Hg) | 55.4 ± 16.6 | 52.8 ± 16.7 | 52.2 ± 17.0 | <0.001 | 56.1 ± 17.0 | 52.3 ± 16.3 | 51.9 ± 16.9 | <0.001 |
| Heart rate (beats/min) | 68.0 ± 9.4 | 62.3 ± 8.0 | 58.5 ± 7.9 | <0.001 | 66.4 ± 9.8 | 62.3 ± 8.4 | 59.8 ± 8.4 | <0.001 |
| Total cholesterol (mg/dl) | 196.3 ± 35.6 | 194.8 ± 36.5 | 192.6 ± 33.8 | 0.017 | 195.4 ± 35.6 | 195.4 ± 35.8 | 192.8 ± 34.5 | 0.057 |
| HDL cholesterol (mg/dl) | 50.6 ± 14.9 | 50.8 ± 14.8 | 52.2 ± 15.3 | 0.008 | 50.8 ± 14.7 | 50.9 ± 15.4 | 51.9 ± 15.0 | 0.090 |
| LDL cholesterol (mg/dl) | 117.4 ± 30.8 | 117.9 ± 32.7 | 116.7 ± 30.1 | 0.580 | 116.8 ± 31.0 | 118.2 ± 32.2 | 117.0 ± 30.5 | 0.422 |
| Triglycerides (mg/dl) | <0.001 | <0.001 | ||||||
| Median | 122.0 | 113.0 | 100.0 | 120.0 | 113.0 | 100.0 | ||
| IQR | 84.0–177.0 | 79.0–163.0 | 72.0–149.0 | 83.0–172.0 | 80.0–163.0 | 72.0–150.0 | ||
| Fasting glucose (mg/dl) | 100.9 ± 33.6 | 95.2 ± 27.7 | 92.3 ± 23.3 | <0.001 | 101.1 ± 35.2 | 94.9 ± 26.2 | 92.0 ± 22.3 | <0.001 |
| Diabetes mellitus (%) | 15.8 | 10.4 | 8.3 | <0.001 | 16.0 | 10.3 | 7.9 | <0.001 |
| C-reactive protein (mg/L) | 0.003 | 0.019 | ||||||
| Median | 2.0 | 1.7 | 1.7 | 1.9 | 1.7 | 1.7 | ||
| IQR | 0.9–4.4 | 0.7–3.7 | 0.7–3.9 | 0.8–4.3 | 0.7–3.8 | 0.7–3.9 | ||
| CAC score >10 (%) | 49.6 | 39.7 | 31.7 | <0.001 | 48.8 | 40.4 | 31.2 | <0.001 |
| MRI | ||||||||
| LV mass (g) | 144.0 ± 39.9 | 142.5 ± 37.1 | 147.2 ± 40.9 | 0.002 | 143.2 ± 39.8 | 143.8 ± 38.0 | 146.6 ± 40.2 | 0.037 |
| LVEDV (cm 3 ) | 122.1 ± 29.8 | 125.9 ± 31.3 | 130.0 ± 31.9 | <0.001 | 122.0 ± 30.5 | 126.7 ± 30.8 | 129.5 ± 31.7 | <0.001 |
| LVESV (cm 3 ) | 38.5 ± 16.3 | 39.3 ± 16.8 | 41.2 ± 16.6 | <0.001 | 37.9 ± 16.2 | 39.8 ± 16.6 | 41.3 ± 16.8 | <0.001 |
| LVEF (%) | 69.2 ± 7.7 | 69.5 ± 7.3 | 68.8 ± 6.9 | 0.056 | 69.6 ± 7.6 | 69.2 ± 7.1 | 68.7 ± 7.1 | 0.002 |
| LV stroke volume (ml) | 83.7 ± 18.8 | 86.6 ± 19.8 | 88.7 ± 20.3 | <0.001 | 84.1 ± 19.5 | 86.9 ± 19.4 | 88.2 ± 20.2 | <0.001 |
| Follow-up time (yrs) | 0.703 | 0.882 | ||||||
| Median | 7.6 | 7.6 | 7.6 | 7.6 | 7.6 | 7.6 | ||
| IQR | 7.3–7.8 | 7.4–7.8 | 7.4–7.8 | 7.3–7.8 | 7.4–7.8 | 7.4–7.8 | ||
∗ p Value for test of difference across tertiles of RMSSD or SDNN using chi-square test for categorical variables, analysis of variance for continuous variables, or Kruskal-Wallis test for nonparametric comparisons.
Hypertension, an increased blood pressure (including increased systolic blood pressure and increased pulse pressure), and an increased heart rate were all associated with reduced HRV. The factors related to metabolic syndrome and diabetes (lower high-density lipoprotein cholesterol, higher triglycerides, higher fasting glucose, and greater prevalence of diabetes) were all present in those with the lowest SDNN and RMSSD tertiles. However, low-density lipoprotein cholesterol and body mass index were similar across the tertiles. Subclinical markers of atherosclerosis and abnormal LV structure and function (i.e., subclinical HF) were also present in those in the lowest SDNN and RMSSD tertiles. The prevalence of a coronary artery calcium score >10, LV mass, and LV volumes were all higher (and stroke volume lower) in participants with the lowest HRV. We observed similar results when these relations between the baseline characteristics and HRV parameters were analyzed using the continuous HRV data instead of tertiles.
During a median follow-up period of 7.6 years, 95 participants developed HF and 98 experienced a myocardial infarction, for an incidence rate of 2.7 per 1,000 person-years for HF and 2.8 per 1,000 person-years for myocardial infarction. New-onset HF has previously been shown to occur more commonly in the MESA participants who were older, male, obese, currently smoking, hypertensive, and diabetic. Several of these factors were also present in the MESA participants in the lowest HRV tertiles ( Table 1 ).
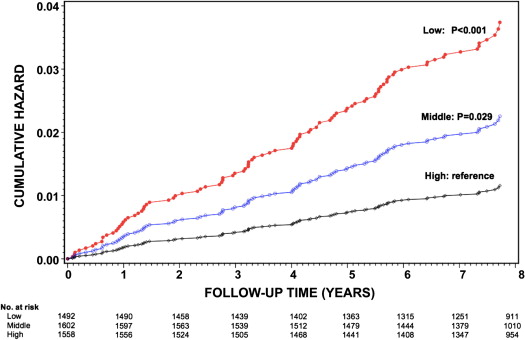
A significant difference was found in the cumulative hazard of incident HF among the participants in the lowest and middle RMSSD tertiles compared with those in the highest tertile (p <0.001 and p = 0.029, respectively; Figure 1 ). In the age-, gender-, and race-adjusted analyses, the hazard ratio of HF was 2.40 (95% confidence interval 1.37 to 4.22) for the lowest RMSSD tertile and 1.74 (95% confidence interval 1.01 to 3.15) for the middle tertile compared with those in the highest tertile (p for trend <0.001; Table 2 , model 1). These significant inverse associations persisted after adjustment for physical activity, diabetes, systolic blood pressure, heart rate, coronary artery calcium, and LV end-systolic volume (p for trend = 0.004, model 2) and additional adjustment for time-varying incident myocardial infarction (p for trend = 0.009, model 3). Additional adjustment for C-reactive protein (model 4) did not attenuate the association. Similar, but less strong, inverse relations were also observed with SDNN and incident HF. Similar findings were also demonstrated when alternative LV parameters (e.g., LV mass, LV end-diastolic volume, and LV ejection fraction) were substituted for LV end-systolic volume in the multivariate analyses.
| Variable | RMSSD Tertiles | SDNN Tertiles | ||||||
|---|---|---|---|---|---|---|---|---|
| Low (1.0–15.9) | Middle (16.0–26.9) | High (27.0–328.0) | Low (0.90–14.5) | Middle (14.6–24.2) | High (24.3–208.1) | |||
| HF | ||||||||
| Patients (n/total) | 49/1,492 | 32/1,602 | 17/1,558 | 50/1,555 | 28/1,565 | 20/1,532 | ||
| Person-years | 10,512 | 11,396 | 11,105 | 10,937 | 11,140 | 10,935 | ||
| Rate per 1,000 person-years | 4.7 | 2.8 | 1.5 | 4.6 | 2.5 | 1.8 | ||
| Model ∗ | HR (95% CI) | p for Trend † | HR (95% CI) | p for Trend † | ||||
| 1 | 2.40 (1.37–4.22) ‡ | 1.74 (1.01–3.15) ‡ | 1.0 (Reference) | <0.001 | 1.88 (1.11–3.20) ‡ | 1.28 (0.72–2.28) | 1.0 (Reference) | <0.001 |
| 2 | 2.24 (1.20–4.18) ‡ | 1.94 (1.07–3.54) ‡ | 1.0 (Reference) | 0.004 | 1.71 (1.00–3.00) ‡ | 1.38 (0.77–2.47) | 1.0 (Reference) | 0.002 |
| 3 | 1.83 (1.00–3.50) ‡ | 1.96 (1.07–3.58) ‡ | 1.0 (Reference) | 0.009 | 1.50 (0.84–2.69) | 1.29 (0.72–2.32) | 1.0 (Reference) | 0.007 |
| 4 | 1.85 (1.00–3.53) ‡ | 1.90 (1.04–3.47) ‡ | 1.0 (Reference) | 0.009 | 1.49 (0.83–2.67) | 1.23 (0.68–2.23) | 1.0 (Reference) | 0.008 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


