Periodontitis and atherosclerosis are highly prevalent chronic inflammatory diseases, and it has been suggested that periodontitis is an independent risk factor of cardiovascular disease (CVD) and that a causal link may exist between the 2 diseases. Using Danish national registers, we identified a nationwide cohort of 17,691 patients who received a hospital diagnosis of periodontitis within a 15-year period and matched them with 83,003 controls from the general population. We performed Poisson regression analysis to determine crude and adjusted incidence rate ratios of myocardial infarction, ischemic stroke, cardiovascular death, major adverse cardiovascular events, and all-cause mortality. The results showed that patients with periodontitis were at higher risk of all examined end points. The findings remained significant after adjustment for increased baseline co-morbidity in periodontitis patients compared with controls, for example, with adjusted incidence rate ratio 2.02 (95% CI 1.87 to 2.18) for cardiovascular death and 2.70 (95% CI 2.60 to 2.81) for all-cause mortality. Patients with a hospital diagnosis of periodontitis have a high burden of co-morbidity and an increased risk of CVD and all-cause mortality. In conclusion, our results support that periodontitis may be an independent risk factor for CVD.
Periodontitis is a chronic inflammatory disease of the tooth supporting tissues and is caused by oral bacteria, primarily anaerobic gram-negative rods and spirochetes, organized in protective biofilms on the surface of the teeth and extending into the periodontal pockets. This condition may result in a systemic inflammatory response and in combination with the predisposing condition gingivitis, it is the most commonly occurring chronic infection in humans. Although no causal relation has been firmly established, there is mounting evidence of an association between periodontitis and cardiovascular disease (CVD). Periodontitis and CVD share important common risk factors such as smoking, diabetes mellitus, and low socioeconomic status. Most observational studies favor an association between periodontitis and CVD that is largely independent of these overlapping risk factors. There is a relative scarcity of epidemiological studies in unselected large populations of the association between periodontitis and CVD. Therefore, we used the validated Danish national registries to investigate this association in a cohort of the entire adult Danish population over a 15-year period.
Methods
In Denmark, a unique 10-digit personal identification number is assigned all citizens at birth or at immigration which allows individual linkage to national administrative registries. All Danish citizens have free and equal access to health care services, and all hospital admissions are registered in the Danish National Patient Register established in 1977. Outpatient hospital contacts have been included since 1995. Registration is performed using the International Classification of Diseases (ICD) codes. ICD-8 was used until 1994 and ICD-10 hereafter. For administrative reasons, ICD-9 was never used in Denmark. Since 1994 detailed information on pharmacy-dispensed medications are registered in the Danish Registry of Medicinal Products Statistics in accordance with the international Anatomical Therapeutic Chemical classification system. Tax-reported income is recorded in Statistics Denmark and information on age, gender, migration, and vital status is available from the Civil Registration System. Cause of death is registered within 2 weeks of death in the Danish Register of Causes of Death using ICD-10 codes.
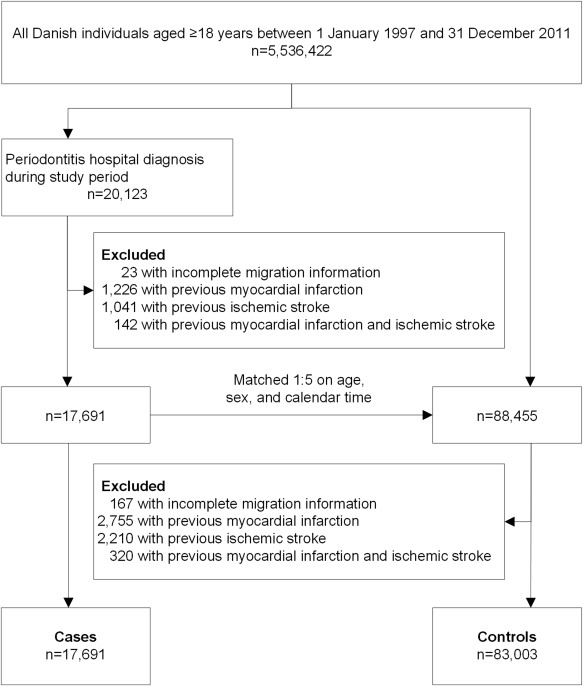
As cases, we identified patients aged ≥18 years with a first-time hospital diagnosis (inpatient or outpatient) of periodontitis from January 1, 1997, to December 31, 2011. Index date for cases was defined as the date of first diagnosis. To identify the case patients, we used ICD-8-codes 523.39 and 523.49, and ICD-10 codes K05.2-05.3, covering acute and chronic periodontitis (excluding K05.2 C [acute pericoronitis]). Most hospital diagnoses of periodontitis were registered by departments of dental, oral and maxillofacial surgery and based on clinical examination and radiological findings. The patients were primarily referred from dental clinics due to suspected presence of complicating factors, for example, oral cysts, concomitant oral mucosal disease, or special requirements for patient sedation. Because individual dentists differ in their threshold for referring patients to hospitals, the periodontitis hospital diagnoses were not limited to severe disease. Each case patient was matched on age, gender, and index date with 5 control subjects from the general population. The cohort was followed until death from any cause, migration or occurrence of an endpoint, whichever came first. Primary endpoints were a diagnosis of myocardial infarction (MI; I21 to I22), ischemic stroke (I63 to I64), and cardiovascular death (I00 to I99), respectively. Secondary endpoints were major adverse cardiovascular events (MACE), that is, a composite of MI, ischemic stroke and cardiovascular death, and all-cause mortality, respectively. The respective endpoints were examined in separate analyses, and the occurrence of an endpoint in one analysis did not result in censoring in the other analyses. All patients (cases and controls) with a history of MI or ischemic stroke before the index date were excluded from the study.
Baseline co-morbidity was assessed up to 5 years before index date for the following diagnoses: alcohol abuse, cardiac dysrhythmia, diabetes mellitus, heart failure, hypertension, ischemic heart disease/peripheral artery disease, renal disease, and venous thromboembolism. Hypertension was defined using a previously validated method with either as a hospital diagnosis or if the patient within a 90 day-period had received treatment with at least 2 of the following classes of antihypertensive agents: beta blockers, calcium channel blockers, renin-angiotensin system inhibitors, α-adrenergic blockers, vasodilators, and nonloop diuretics. Diabetes mellitus was defined as a hospital diagnosis or treatment with glucose-lowering drugs. Smoking history was assessed using a data retrieval algorithm dependent on ICD-10 codes for smoking, tobacco use, chronic obstructive pulmonary disease, lung cancer, and treatment with prescription drugs for smoking cessation and/or therapeutic interventions aimed at smoking cessation as previously described. In a similar manner, alcohol abuse was defined by either the hospital diagnosis or by including conditions strongly related to alcohol abuse, for example, alcoholic liver disease, pharmacological alcohol dependency treatment, and/or treatment intervention. We calculated an age-standardized index of socioeconomic status from 0 to 4 based on average gross annual income during a 5-year period before study inclusion. Baseline pharmaceutical treatment up to 6 months before the index date was registered for the following drug: cholesterol-lowering drugs, loop diuretics, platelet inhibitors, and vitamin K antagonists.
Baseline characteristics were described using means and SDs for continuous variables and frequencies and percentages for categorical variables. Incidence rates (IRs) were summarized per 1,000 person-years at risk, and Poisson regression analyses were performed to estimate crude and adjusted IR ratios (IRRs). Model assumptions including linearity of continuous variables were tested and found valid unless otherwise specified. p Values <0.05 were considered statistically significant and 95% CIs were reported where applicable. Statistical analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, North Carolina) and Stata software, version 11.0 (StataCorp, College Station, Texas).
Study approval was obtained from the Danish Data Protection Agency (ref. 2007-58-0015, int. ref. GEH-2014, I-Suite 02736). Approval from an ethics committee is not required for register studies in Denmark since data are encrypted and rendered anonymous when used for research purposes. Conduct and reporting in this study was done in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology recommendations.
Results
From January 1, 1997, and December 31, 2011, we identified 20,123 subjects with a hospital diagnosis of periodontitis, and after excluding 2,432 subjects with a history of MI, stroke, or incomplete follow-up, the final number of periodontitis cases was 17,691. Each case was matched on gender, age, and index date with 5 controls from the general population (n = 88,455). Of these, 5,452 subjects were also excluded due to a history of MI, stroke, or migration, leaving a final control population of 83,003 subjects. Figure 1 shows a flow chart of the study population.
Baseline characteristics of the final study population are presented in Table 1 . Patients with periodontitis had lower socioeconomic status (1.7 vs 2.1), a higher proportion of smokers (18.1% vs 9.5%), and an overall higher degree of co-morbidity and medication than the general population.
| Periodontitis cases (n=17,691) | Controls (n=83,003) | |
|---|---|---|
| Mean (SD) age (years) | 57.3 (15.1) | 56.6 (15.0) |
| Women | 7,451 (42.1%) | 35,822 (43.2%) |
| Men | 10,240 (57.9%) | 47,181 (56.8%) |
| Mean (SD) socioeconomic status | 1.7 (1.3) | 2.1 (1.4) |
| Smoking, ever | 3,193 (18.1%) | 7,916 (9.5%) |
| Comorbidity | ||
| Alcohol abuse | 811 (4.6%) | 1,320 (1.6%) |
| Cardiac dysrhytmia | 819 (4.9%) | 1,312 (1.6%) |
| Diabetes | 1,344 (7.6%) | 3,647 (4.4%) |
| Heart failure | 743 (4.2%) | 671 (0.8%) |
| Hypertension | 4,073 (23.0%) | 11,422 (13.8%) |
| Peripheral artery disease | 1,362 (7.7%) | 1,737 (2.1%) |
| Chronic renal disease | 498 (2.9%) | 215 (0.3%) |
| Venous thromboembolism | 308 (1.7%) | 665 (0.8%) |
| Medication | ||
| Cholesterol-lowering drugs | 2,553 (14.4%) | 7,475 (9.0%) |
| Loop diuretics | 2,308 (13.1%) | 2,978 (3.6%) |
| Platelet inhibitors | 2,702 (15.3%) | 6,657 (8.0%) |
| Vitamin K antagonists | 930 (5.3%) | 1,390 (1.7%) |
The IRs per 1,000 person-years of MI, ischemic stroke, cardiovascular death, MACE, and all-cause death were 5.69, 9.93, 13.17, 24.19, and 58.35 for patients with periodontitis and 3.95, 5.26, 5.50, 11.94, and 18.22 for controls, respectively.
Crude and adjusted IRRs are presented in Table 2 . In the analyses adjusted for age, gender, and all examined covariates, patients with periodontitis had significantly increased risk of all study end points, for example, IRRs of 2.02 (95% CI 1.87 to 2.18) for cardiovascular death and 2.70 (95% CI 2.60 to 2.81) for all-cause mortality ( Table 2 ).
| Crude IRR | Adjusted IRR ∗ | |||||
|---|---|---|---|---|---|---|
| IRR | 95% CI | P-value | IRR | 95% CI | P-value | |
| Myocardial infarction | 1.44 | 1.30-1.60 | <0.001 | 1.16 | 1.04-1.30 | <0.05 |
| Ischemic stroke | 1.89 | 1.74-2.05 | <0.001 | 1.51 | 1.38-1.65 | <0.001 |
| Cardiovascular death | 2.54 | 2.36-2.72 | <0.001 | 2.02 | 1.87-2.18 | <0.001 |
| MACE | 2.03 | 1.92-2.14 | <0.001 | 1.55 | 1.47-1.65 | <0.001 |
| All-cause mortality | 3.20 | 3.09-3.32 | <0.001 | 2.70 | 2.60-2.81 | <0.001 |
∗ Adjusted for age, gender, smoking, co-morbidities, medication, and socioeconomic status.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


