Obesity is well-established as a major cardiovascular (CV) risk factor. Obesity confers a greater risk for developing atrial fibrillation (AF), but the relation between obesity and established nonvalvular AF for stroke and all-cause death is still unclear. To ascertain the prevalence of overweight and obesity in patients with nonvalvular AF, their influence on adverse events, and the relation with anticoagulation control, we performed this post hoc analysis of the pooled Stroke Prevention using an Oral Thrombin Inhibitor in patients with atrial Fibrillation (SPORTIF) III and V data sets. For this study, we analyzed all patients assigned to the warfarin arm with data on body mass index (BMI). Time in therapeutic range was used as an index of the quality of anticoagulation control. The 3,630 patients eligible for this analysis were categorized as follows: (1) BMI 18.5 to 24.9 (“normal weight”) in 24.1%; (2) BMI 25.0 to 29.9 (“overweight”) in 39.8%; and BMI ≥30 (“obese”) in 36.1%. Both overweight (hazard ratio [HR] 0.70) and obese (HR 0.59) categories were inversely associated with the composite outcome of stroke/all-cause death. A similar inverse association was seen for the end point of stroke (HR 0.61 and 0.47, respectively). Good anticoagulation control also attenuated the association between BMI categories and outcomes. In patients with time in therapeutic range >70%, BMI category was not significantly associated with the composite outcome of stroke/death and stroke. Stroke and all-cause death progressively reduced in overweight and obese anticoagulated patients with AF. The inverse relation of BMI categories to the risk of stroke and all-cause death was mitigated by good anticoagulation control.
Obesity represents one of the most prevalent cardiovascular (CV) risk factors in the general population. Data released from the USA Center for Disease Control ( http://www.cdc.gov/obesity/index.html ) show that in the past 20 years, the prevalence of obesity has rapidly increased, up to 25% of the population. Obesity has been associated with a higher incidence of both CV and cerebrovascular events in the general population. Indeed, obesity has been identified as one of the most important risk factors to be controlled in both primary and secondary preventions. The relation between obesity and atrial fibrillation (AF) is robust, with evidence documenting how obesity could be a trigger and major risk factor in determining AF occurrence, with a direct causal relation. Indeed, some recent data have shown how interventions to reduce weight in obese patients could lead to a reduction in the risk of developing AF. However, data on the influence of obesity on adverse outcomes in AF patients have been conflicting. Although some data suggest that obese and overweight AF patients had a lower risk for both CV and all-cause death, other evidence indicates that both overweight and obese patients with AF are at greater risk for the composite outcome of ischemic stroke, thromboembolism (TE), and all-cause death. Another consideration is the risk of adverse outcomes while on anticoagulation in patients with AF with low body weight, being associated with a greater bleeding risk ; this leads some guidelines recommending a lower therapeutic target to mitigate bleeding risks. The aims of this study were (1) to describe the prevalence of overweight and obesity in an anticoagulated clinical trial cohort of patients with nonvalvular AF (NVAF); (2) define risks related to each weight category for the occurrence of stroke, all-cause death, and their composite outcome; and (3) to determine the relation between quality of anticoagulation control (as reflected by time in therapeutic range, [TTR]) and being overweight or obese.
Methods
For the purposes of the present study, we analyzed pooled data sets from the Stroke Prevention using an Oral Thrombin Inhibitor in patients with atrial Fibrillation (SPORTIF) III and V trials. Details on the trial protocol have been reported elsewhere. In brief, the SPORTIF trials were 2 large multicenter phase III clinical trials comparing the efficacy and safety of the direct thrombin inhibitor, ximelagatran, compared against warfarin in NVAF. SPORTIF III was an open-label trial, whereas SPORTIF V was a double-blind study. From the pooled data sets, we included all patients assigned to warfarin treatment where data on height and weight were recorded, to obtain body mass index (BMI) measurements for this post hoc analysis.
BMI values were used to define weight categories. According to the standard World Health Organization definition ( http://www.who.int/mediacentre/factsheets/fs311/en/index.html ), patients were categorized as (1) BMI from 18.5 to 24.9 kg/m 2 (“normal weight”); (2) BMI 25.0 to 29.9 kg/m 2 (“overweight”)l and (3) BMI ≥30 kg/m 2 (“obese”). Patients with a BMI <18.5 kg/m 2 were excluded from these analyses because of the small numbers.
TE risk was categorized according to CHA 2 DS 2 -VASc score. “Low-risk” patients were defined as men with a CHA 2 DS 2 -VASc = 0 or women with CHA 2 DS 2 -VASc = 1; “moderate risk” was defined as male patients with CHA 2 DS 2 -VASc = 1; and “high risk” with CHA 2 DS 2 -VASc ≥2. Anticoagulation control, as reflected by TTR, was calculated according to the standardized Rosendaal interpolation method. Based on the European Society of Cardiology recommendations, optimal anticoagulation was defined as a TTR >70%.
Stroke was clinically defined as the acute onset of a focal neurologic deficit in any of the carotid, vertebral, or cerebral artery distribution territories lasting >24 hours, irrespective of the pathophysiological mechanism. This was the trial protocol–defined primary outcome, which was formally adjudicated. Myocardial infarction (MI) diagnosis required 2 of 3 of the following criteria: (1) typical chest pain lasting at least 20 minutes; (2) electrocardiographic changes clearly indicating an acute MI; (3) significant, that is, >2× upper limit, elevation of cardiac biomarkers (creatine-kinase-MB, troponin). Major bleeding, according to International Society of Thrombosis and Hemostasis criteria, was defined by one of the following criteria: clinically overt bleeding with a concomitant decrease in hemoglobin levels ≥2 g/dl or requiring blood transfusion of at least 2 U of whole blood or erythrocytes; bleeding episode involving a critical site (i.e., intracranial, retroperitoneal, intraocular, intraspinal, atraumatic intraarticular, or pericardial). Mortality was related to the reported occurrence of death by any investigator. A composite outcome of stroke and all-cause death was also considered. All outcomes were assessed by a central adjudication committee.
All continuous variables were tested for normality. Variables normally distributed were expressed as mean and SD and tested for differences using one-way analysis of variance. Nonparametric variables were expressed as median and interquartile range (IQR) and differences tested using the Kruskal–Wallis test. Categorical variables, expressed as counts and percentages, were analyzed by the chi-square test. Crude and age-adjusted study outcomes rates were estimated. Logistic regression analysis, crude and adjusted for age, gender, and TE risk, was computed to analyze the association between weight categories and outcomes. Linear regression analysis, adjusted for age, gender, and TE risk, was used to examine the relation between BMI and TTR.
Survival analysis, assessed by an intention-to-treat approach, was performed according to the different weight categories, and differences in survival were analyzed using the log-rank test. Evaluation of clinical characteristics significantly associated with outcomes was explored using a Cox proportional hazards analysis. All variables analyzed at baseline underwent univariate analysis (see Supplementary Tables 1 to 3 ). All variables with a p value <0.10 for the association in the univariate analysis were included in the forward stepwise multivariate model. A linear regression analysis, adjusted for age, gender, and TE risk, between outcomes risk and BMI was also conducted. A 2-sided p value <0.05 was considered statistically significant. All analyses were performed using SPSS v. 22.0 (IBM, New York).
Results
From the original SPORTIF pooled cohorts of 7,329 patients, patients assigned to the warfarin treatment arm were selected. Of the 3,665 patients treated with warfarin, data on BMI were available for 3,651 (99.6%). After the exclusion of patients with BMI <18.50 kg/m 2 (n = 21 [0.6%]), a total of 3,630 patients (median [IQR] age 72 [66 to 77]; 30.3% women) were included in this analysis. Overweight was recorded for 1,446 (39.8%) patients, whereas 1,310 (36.1%) patients were categorized as obese.
High TE risk was recorded in 86.7% (n = 3,149) and median TTR for the overall population was 65.6% (IQR 55.2% to 79.3%). Median age progressively decreased from normal weight to obese patients (p <0.001). Patients in the normal-weight category were more commonly women compared to obese and overweight patients (p <0.001). Median creatinine clearance levels progressively increased, from normal-weight to obese categories (p <0.001).
Baseline characteristics, according to BMI categories, are reported in Table 1 . Prevalence of hypertension and diabetes mellitus progressively increased from normal-weight to obese patients (p <0.001). Patients with normal weight were more frequently smokers (p = 0.006) and more likely to have had a previous stroke/transient ischemic attack (TIA; p <0.001) compared to overweight and obese subjects. High TE risk was more prevalent in normal-weight patients, compared to overweight and obese patients (p <0.001).
| Variable | Normal Weight (n= 874) | Overweight (n= 1,446) | Obese (n= 1,310) | p |
|---|---|---|---|---|
| Age (years) | ||||
| Median [IQR] | 76 [70-80] | 73 [67-77] | 68 [62-74] | <0.001 |
| Female | 328 (37.5%) | 369 (25.5%) | 403 (30.8%) | <0.001 |
| Creatinine Clearance (ml/min) | ||||
| Median [IQR] | 58.82 [47.89-72.59] | 76.93 [60.67-92.85] | 100.52 [78.39-130.11] | <0.001 |
| Type of Atrial Fibrillation ∗ | 0.418 | |||
| Paroxysmal | 104 (11.9%) | 159 (11.0%) | 125 (9.5%) | |
| Chronic | 770 (88.1%) | 1,826 (88.9%) | 1,184 (90.4%) | |
| Hypertension | 580 (66.4%) | 1,077 (74.5%) | 1,134 (86.6%) | <0.001 |
| Diabetes Mellitus | 138 (15.8%) | 306 (21.2%) | 412 (31.5%) | <0.001 |
| Current Smoker | 101 (11.6%) | 110 (7.6%) | 119 (9.1%) | 0.006 |
| Coronary Heart Disease | 392 (44.9%) | 635 (43.9%) | 578 (44.2%) | 0.906 |
| Previous Stroke/TIA | 234 (26.8%) | 310 (21.4%) | 203 (15.5%) | <0.001 |
| Chronic Heart Failure | 320 (36.6%) | 524 (36.2%) | 515 (39.3%) | 0.211 |
| Previous Bleeding | 50 (5.7%) | 93 (6.4%) | 65 (5.0%) | 0.253 |
| Aspirin Treatment | 190 (21.7%) | 292 (20.2%) | 239 (18.2%) | 0.123 |
| TTR † (%) | ||||
| Median [IQR] | 66.5 [52.1-78.7] | 69.7 [56.7-80.5] | 68.6 [55.9-78.8] | 0.002 |
| TTR>70% † | 382 (44.2%) | 702 (49.1%) | 605 (46.7%) | 0.070 |
| CHA 2 DS 2 -VASc | <0.001 | |||
| Median [IQR] | 3 [2-4] | 3 [2-4] | 3 [2-4] | |
| CHA 2 DS 2 -VASc Risk Categories | <0.001 | |||
| Low | 1 (0.1%) | 2 (0.1%) | 3 (0.2%) | |
| Intermediate | 58 (6.6%) | 177 (12.2%) | 240 (18.3%) | |
| High | 815 (93.2%) | 1,267 (87.6%) | 1,067 (81.5%) | |
Mean (SD) and median (IQR) follow-up time was 566.52 ± 142.84 days and 567 (492 to 652) days, respectively. During the entire follow-up observation, 90 (2.5%) strokes, 164 (4.5%) major bleeding, 52 (1.4%) MIs, and 195 (5.4%) all-cause death events were observed. Hemorrhagic stroke was recorded only in 11 patients (0.3%), so these were not considered separately from ischemic stroke. For the composite outcome of stroke/all-cause death, a total of 266 (7.3%) events were recorded. Crude study outcomes rates progressively decreased from the normal-weight to obese category for stroke (p = 0.016), all-cause death (p = 0.001), and the composite outcome of stroke/all-cause death (p <0.001, Table 2 ). Taking into account age-adjusted rates, patients with normal weight reported consistently higher rates for stroke, all-cause death, and composite outcome ( Table 2 ).
| Normal Weight (n= 874) | Overweight (n= 1,446) | Obese (n= 1,310) | p | |
|---|---|---|---|---|
| Stroke/All-Cause Death | 94 / 266 (10.8%) | 97 / 266 (6.7%) | 75 / 266 (5.7%) | <0.001 |
| Age-adjusted rate | 10.1% | 6.6% | 5.9% | |
| OR (95%CI) crude | Ref | 0.60 (0.44-0.80) | 0.50 (0.37-0.69) | <0.001 ∗ |
| Adjusted † | Ref | 0.64 (0.48-0.87) | 0.61 (0.44-0.85) | <0.001 ∗ |
| Stroke | 33 / 90 (3.8%) | 32 / 90 (2.2%) | 25 / 90 (1.9%) | 0.016 |
| Age-adjusted rate | 3.4% | 2.2% | 1.9% | |
| OR (95%CI) crude | Ref | 0.58 (0.35-0.95) | 0.50 (0.29-0.84) | 0.022 ∗ |
| Adjusted † | Ref | 0.58 (0.35-0.95) | 0.50 (0.29-0.84) | 0.022 ∗ |
| Major Bleeding | 47 / 164 (5.4%) | 61 / 164 (4.2%) | 56 / 164 (4.3%) | 0.372 |
| Age-adjusted rate | 5.6% | 4.1% | 4.5% | |
| OR (95%CI) crude | Ref | 0.91 (0.58-1.43) | 0.93 (0.59-1.46) | 0.919 ∗ |
| Adjusted † | Ref | – | – | – |
| Myocardial Infarction | 14 / 52 (1.6%) | 19 / 52 (1.3%) | 19 / 52 (1.5%) | 0.850 |
| Age-adjusted rate | 1.2% | 1.3% | 1.4% | |
| OR (95%CI) crude | Ref | 0.82 (0.41-1.64) | 0.90 (0.45-1.81) | 0.851 ∗ |
| Adjusted † | Ref | – | – | – |
| All-Cause Death | 68 / 195 (7.8%) | 73 / 195 (5.0%) | 54 / 195 (4.1%) | 0.001 |
| Age-adjusted rate | 7.4% | 5.0% | 4.3% | |
| OR (95%CI) crude | Ref | 0.63 (0.45-0.89) | 0.51 (0.35-0.74) | 0.001 ∗ |
| Adjusted † | Ref | 0.66 (0.46-0.93) | 0.62 (0.42-0.91) | <0.001 ∗ |
∗ Chi-square for entire model.
Stroke incidence was significantly higher in patients with normal weight (2.5% patient-years) than in overweight and obese patients (1.4% and 1.2% patient-years, respectively). All-cause death and composite outcome incidence progressively decreased from normal weight to overweight to obese patients (5.2% vs 3.3% vs 2.6% patient-years, 7.2% vs 4.3% vs 3.6% patient-years, respectively). No difference was seen in major bleeding or MI incidence rates in the 3 BMI categories. Logistic regression analysis showed that both overweight and obese categories were inversely associated with the composite outcome, stroke, and all-cause death, after adjustment for age, gender, and TE risk categories ( Table 2 ).
Considering TTR as a continuous variable, lower median (IQR) values were found in normal-weight patients (p = 0.002). The proportion of patients with good anticoagulation control (TTR >70%) was lower in patients with normal weight, with a nonsignificant trend to being greater in overweight and obese patients (p = 0.070).
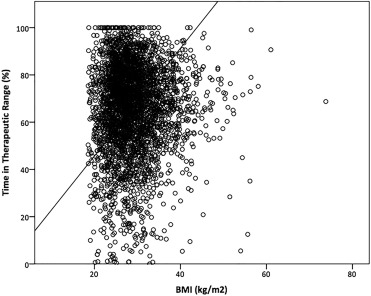
Linear regression analysis, adjusted for age, gender, and TE risk, showed a significant linear association between BMI and TTR ( Figure 1 ). Similar relationships were found for regressions according to age classes, gender, and TE risk categories using CHA 2 DS 2 -VASc (see Supplementary Figures 1 to 3 ). No significant association was found between weight categories and TTR >70%.
Kaplan–Meier curves showed that both overweight and obese patients had a lower risk for the occurrence of the composite outcome, stroke, and all-cause death ( Figure 2 ).
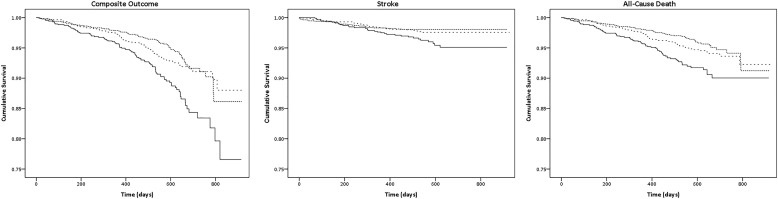
On univariate analysis (see Supplementary Tables 1 to 3 ), a Cox multivariate analysis model ( Table 3 ) adjusted for the interactions between weight categories and TTR showed that the composite outcome was inversely associated to both overweight and obese categories, as well as good anticoagulation control. Stroke was inversely associated with being overweight and obese. Conversely, the association of all-cause death and weight categories was attenuated by good-quality anticoagulation control (TTR >70%) and creatinine clearance.
| HR (95% CI) | HR (95% CI) | ||
|---|---|---|---|
| Stroke/All-Cause Death | Stroke/All-Cause Death | ||
| Normal Weight (ref.) | — | Normal Weight (ref.) | — |
| Overweight | 0.69 (0.52-0.92) | Overweight | 0.71 (0.53-0.96) |
| Obese | 0.59 (0.42-0.82) | Obese | 0.60 (0.43-0.83) |
| TTR>70% | 0.66 (0.51-0.84) | TTR (%) | 0.98 (0.98-0.99) |
| Age (per year) | 1.03 (1.01-1.04) | Age (per year) | 1.03 (1.01-1.04) |
| Chronic Heart Failure | 1.53 (1.20-1.96) | Previous Stroke/TIA | 1.60 (1.23-2.09) |
| Previous Stroke/TIA | 1.58 (1.21-2.07) | Chronic Heart Failure | 1.54 (1.21-1.98) |
| Coronary Heart Disease | 1.63 (1.26-2.10) | Coronary Heart Disease | 1.64 (1.27-2.11) |
| Current Smoker | 1.73 (1.19-2.50) | Current Smoker | 1.74 (1.20-2.52) |
| Stroke | Stroke | ||
| Normal Weight (ref.) | — | Normal Weight (ref.) | — |
| Overweight | 0.61 (0.37-0.99) | Overweight | 0.64 (0.39-1.04) |
| Obese | 0.47 (0.27-0.81) | Obese | 0.49 (0.28-0.84) |
| TTR>70% | 0.62 (0.40-0.96) | TTR (%) | 0.98 (0.97-0.99) |
| Previous Stroke/TIA | 2.26 (1.46-3.50) | Coronary Heart Disease | 1.53(1.01-2.35) |
| Previous Stroke/TIA | 2.28 (1.48-3.53) | ||
| All-Cause Death | All-Cause Death | ||
| Creatinine Clearance (per ml) | 0.99 (0.98-0.99) | Creatinine Clearance (per ml) | 0.99 (0.98-0.99) |
| TTR>70% | 0.64 (0.47-0.85) | TTR (%) | 0.98 (0.98-0.99) |
| Current Smoker | 1.66 (1.08-2.56) | Current Smoker | 1.64 (1.07-2.52) |
| Previous Stroke/TIA | 2.02 (1.51-2.72) | Previous Stroke/TIA | 2.04 (1.52-2.74) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


