Past studies examining the effects of the metabolic syndrome (MS) on prognosis in postangiography patients were limited in size or were controversial in results. The aim of the study was to examine the association of the MS and the risk for long-term mortality in a large cohort of patients undergoing coronary angiography for various clinical indications. Medical history, physical examination, and laboratory values were used to diagnose patients with the MS. Cox regression models were used to analyze the effect of MS on long-term all-cause mortality. We prospectively recruited 3,525 consecutive patients with a mean age of 66 ± 22 years (range 24 to 97) and 72% men. Thirty percent of the cohort had MS. Patients with MS were more likely to have advanced coronary artery disease and acute coronary syndrome (p <0.001). Patients with MS had more abnormalities in their metabolic and inflammatory biomarkers regardless of their clinical presentation. A total of 495 deaths occurred during a mean follow-up period of 1,614 ± 709 days (median 1,780, interquartile range 1,030 to 2,178). MS was associated with an increased risk of death in the general cohort (hazard ratio [HR] 1.27, 95% confidence interval [CI] 1.01 to 1.56, p = 0.02). MS had a significant effect on mortality in stable patients (HR 1.55, 95% CI 1.1 to 2.18, p = 0.01), whereas it did not have a significant effect on mortality in patients with acute coronary syndrome (HR 1.11, 95% CI 0.86 to 1.44, p = 0.42). In conclusion, MS is associated with increased mortality in postangiography patients. Its adverse outcome is mainly seen in patients with stable angina.
Highlights
- •
The effect of the metabolic syndrome (MS) on prognosis in the catheterization laboratory is controversial.
- •
Patients with MS had more CAD, ACS, and elevated atherogenic biomarkers.
- •
MS had a significant effect on mortality in stable patients and not in patients with ACS.
In the present study, we examined whether the presence of metabolic syndrome (MS) constitutes a risk factor for long-term mortality in a large cohort of patients undergoing coronary angiography for various clinical indications. We aimed to assess the association of the MS in patients presenting with acute coronary syndrome (ACS) compared with patients presenting with stable angina.
Methods
The data in this study were collected from the Tel Aviv Prospective Angiographic Survey (TAPAS) database. The TAPAS is a prospective, single-center registry that enrolls all patients undergoing cardiac catheterization at the Tel Aviv Medical Center. The study cohort consisted of consecutive patients referred for coronary angiography in our institution for various clinical presentations. Excluded were patients with known diabetes mellitus (DM) because we aimed to evaluate the effect of MS on outcomes without the confounding effect of diabetic patients. All the enrollees signed a written informed consent for participation in the study, which was approved by the institutional ethics committee.
The primary end point of the study was death from any cause. The data were obtained from the Israeli Ministry of Health mortality records. End of follow-up was defined as the first from the following events: death from any cause or November 1, 2013.
MS was diagnosed according to current guidelines. Shortly, waist circumference ≥102 cm in men and ≥88 cm in women, triglycerides ≥150 mg/dl, high-density lipoprotein cholesterol <40 mg/dl in men and <50 mg/dl in women, elevated blood pressure (≥130 mm Hg systolic pressure or ≥85 mm Hg diastolic pressure), and fasting glucose ≥100 mg/dl. The presence of ≥3 of the individual criteria was categorized as MS. Recently, it was shown that diagnosis of MS during hospitalization for ACS is accurate.
Categorical variables were compared using the chi-square test and continuous variables by t test (presented as means with SD) or the Kruskal-Wallis/Mann-Whitney test (medians with interquartile range). Continuous variables were tested for normal distribution using the Kolmogorov-Smirnov test and Q-Q plots. All-cause mortality was evaluated using univariate and multivariate Cox proportional hazard regression. All clinical features, biochemical variables, and potential confounders that were significant in univariate analysis, as presented in Table 1 , were available for selection in this model. The influence of MS was checked by assessing its significance by adding it in a second block in the regression models. A 2-tailed p <0.05 was considered statistically significant. All analyses were performed with the SPSS 19.0 software (SPSS Inc., Chicago, Illinois).
| Variable | Entire cohort | Metabolic Syndrome | P value ∗ | |
|---|---|---|---|---|
| (N=3525) | YES(N=1055) | NO (N=2470) | ||
| Males | 2555 (72.5%) | 742 (70%) | 1813(73%) | 0.06 |
| Age(years) | 65.4±12.2 | 65.8±12.5 | 64.4±11.5 | 0.01 |
| Hypertension | 2347 (66.5%) | 958 (91%) | 1385 (56%) | <0.001 |
| Impaired fasting glucose | 786 (22.3%) | 413 (39%) | 370 (15%) | <0.001 |
| Dyslipidemia | 2492 (70.6%) | 838 (79%) | 1650 (67%) | <0.001 |
| Peripheral arterial disease | 581 (16.5%) | 223 (21%) | 356 (14%) | <0.001 |
| Known coronary heart disease | 1610 (45.6%) | 557 (53%) | 1052 (43%) | <0.001 |
| Prior myocardial infarction | 840 (23.8%) | 305 (29%) | 535 (22%) | <0.001 |
| Prior stroke | 337 (9.5%) | 115 (11%) | 221 (9%) | 0.07 |
| Prior coronary artery bypass surgery | 454 (12.9%) | 152 (14%) | 301 (12%) | 0.07 |
| Current smoker | 855 (24%) | 253 (24%) | 600 (24%) | 0.017 |
| Past smoker | 1342 (38%) | 433 (41%) | 908 (37%) | |
| Indications for angiography | ||||
| Unstable angina pectoris | 790 (22%) | 277 (26%) | 512(20%) | 0.055 |
| Stable angina pectoris | 1703 (48%) | 474 (45%) | 1226(50%) | |
| Non-ST elevation myocardial infarction | 608 (17%) | 195 (19%) | 413(17%) | |
| ST elevation myocardial infarction | 428 (12%) | 109 (10%) | 319(13%) | |
| Number of narrowed coronary arteries | ||||
| 0 | 846 (24%) | 211 (20%) | 643(26%) | 0.002 |
| 1 | 776 (22%) | 232 (22%) | 543(22%) | |
| 2 | 846 (24%) | 274 (26%) | 568(23%) | |
| 3 | 1057 (30%) | 338 (32%) | 716(29%) | |
| Medications | ||||
| Aspirin | 2979 (84.4%) | 897 (85%) | 2079 (84%) | 0.52 |
| Statins | 2595 (73.5%) | 769 (73%) | 1823 (74%) | 0.57 |
| β-blockers | 2242 (63.5%) | 732 (69%) | 1508 (61%) | <0.001 |
| Clopidogrel | 1412 (40%) | 415 (39%) | 996 (40%) | 0.58 |
| Angiotensin converting enzyme inhibitors | 1608 (46%) | 553 (52%) | 1053 (43%) | <0.001 |
| Angiotensin II receptor blockers | 388 (11%) | 152 (14%) | 235 (10%) | <0.001 |
| Oral Hypoglycemics | 431 (12.2%) | 253 (24%) | 176(7%) | <0.001 |
∗ p value relates to the comparison of MetS to non-MetS patients.
Results
A total of 3,525 consecutive patients referred for coronary angiography at the Tel Aviv Medical Center were included in the final analysis. The mean age was 66 ± 22 years (range 24 to 97), and 72% were men. Thirty percent of the study population was diagnosed as having MS. The baseline clinical characteristics are presented in Table 1 . Patients with MS had more cardiac risk factors and more history of myocardial infarction. However, they did not receive more evidence-based medications (statins, aspirin, and so on).
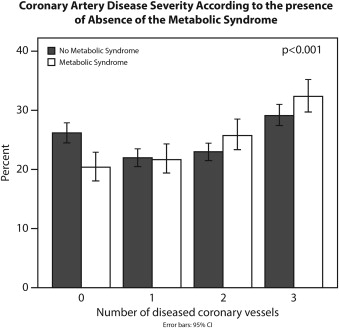
Patients with MS presented with more advanced coronary artery disease (CAD) (odds ratio 1.4, 95% confidence interval [CI] 1.17 to 1.76, p = 0.001; Figure 1 ) and were more likely to present with ACS ( Table 1 ). In addition, the rate of percutaneous coronary intervention was higher in patients with MS than in the rest of the cohort (69% vs 49%, respectively, p <0.001). Patients with MS had unfavorable laboratory tests ( Table 2 ), regardless of the clinical presentation.
| Variable | Acute Coronary Syndrome | p | Stable angina pectoris | p | ||
|---|---|---|---|---|---|---|
| Metabolic Syndrome | No Metabolic Syndrome | Metabolic Syndrome | No Metabolic Syndrome | |||
| N=603 | N=1288 | N=452 | N=1182 | |||
| Glucose (mg/dl) | 127±53 | 101±29 | <0.001 | 112±41 | 94±24 | <0.001 |
| Hs-CRP | 12±22 | 13±28 | <0.001 | 8.6±16 | 6±14 | <0.001 |
| Fibrinogen (mg/dl) | 346±89 | 342±97 | <0.001 | 326±83 | 307±75 | <0.001 |
| Total Cholesterol (mg/dl) | 173±41 | 170±39 | 0.09 | 164±38 | 164±36 | 0.78 |
| Triglycerides (mg/dl) | 191±108 | 115±76 | <0.001 | 176±90 | 109±55 | <0.001 |
| High density lipoprotein cholesterol(mg/dl) | 35±8 | 44±12 | <0.001 | 37±8.6 | 47±13 | <0.001 |
| Non High density lipoprotein cholesterol (mg/dl) | 138±40 | 126±38 | <0.001 | 126±36 | 117±37 | <0.001 |
| Low density lipoprotein cholesterol (mg/dl) | 100±35 | 103±33 | 0.07 | 92±31 | 95±30 | 0.054 |
| HbA1c (%) | 6.6±1.4 | 5.8±0.7 | <0.001 | 6.4±1.2 | 5.8±0.7 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


