Impaired kidney function often accompanies heart failure (HF) and is associated with a worse prognosis. This post hoc analysis of the Treating to New Targets (TNT) trial examined whether the observed decrease in HF hospitalizations with high- compared to low-dose atorvastatin could be related to improvements in kidney function. Of 10,001 TNT participants, 9,376 had estimated glomerular filtration rate (eGFR) measurements at baseline and 1 year and were included in this analysis. The association of change in year-1 eGFR and subsequent HF hospitalization was examined using Cox regression models. In total 218 participants developed subsequent HF hospitalization. Little change in eGFR occurred over 1 year in the atorvastatin 10-mg group, whereas eGFR improved in the 80-mg group by 1.48 ml/min/1.73 m 2 (95% confidence interval 1.29 to 1.67, p <0.0001). Subsequent HF was preceded by a decrease in eGFR over 1 year compared to modest improvement in those without subsequent HF (−0.09 ± 7.89 vs 0.81 ± 6.90 ml/min/1.73 m 2 , p = 0.0015). After adjusting for baseline eGFR, each 5-ml/min/1.73 m 2 increase in eGFR at 1 year was associated with a lower risk of subsequent HF hospitalization (hazard ratio 0.85, 95% confidence interval 0.77 to 0.94, p = 0.002). This relation was independent of treatment effect or change in low-density lipoprotein cholesterol level at 1 year. In conclusion, treatment with high- compared to low-dose atorvastatin was associated with improvement in eGFR at 1 year, which was related to a decrease in subsequent HF hospitalization. This suggests that improvement in kidney function may be related to the beneficial effect of high-dose atorvastatin on HF hospitalization.
In clinical trials, treatment with atorvastatin has been associated with improved estimated glomerular filtration rate (eGFR) in patients with diabetes mellitus, chronic coronary disease, and cerebrovascular disease. In the Treating to New Targets (TNT) trial, the mean increase in eGFR was significantly greater in the atorvastatin 80-mg group compared to the 10-mg group, suggesting that this improvement is dose dependent. Treatment with high-dose atorvastatin was also associated with a significant decrease in rate of heart failure (HF) hospitalizations compared to low-dose treatment. We sought to investigate whether the observed decrease in HF hospitalizations with high-dose atorvastatin was related to improvements in kidney function. The purpose of this post hoc analysis of TNT was threefold: (1) to examine the effect of change in eGFR from baseline to 1 year on subsequent rate of HF hospitalizations, (2) to investigate whether treatment effect (high- vs low-dose atorvastatin) modified the relation between eGFR and HF hospitalizations, and (3) to examine changes in eGFR and the potential relation of these changes to risk of HF hospitalization.
Methods
The design of the TNT study has been described in detail previously. TNT was a randomized, double-blind parallel-group trial in men and women aged 35 to 75 years with clinically evident coronary heart disease (CHD), defined as previous myocardial infarction, previous or present angina with atherosclerotic CHD, or a previous coronary revascularization procedure. To ensure that all patients achieved low-density lipoprotein (LDL) cholesterol levels consistent with then-current guidelines, patients with LDL cholesterol from 130 to 250 mg/dl (3.4 to 6.5 mmol/L) after a wash-out period took open-label treatment with atorvastatin 10 mg/day for 8 weeks. After this run-in period, 10,001 patients with LDL cholesterol <130 mg/dl (<3.4 mmol/L) were randomized to atorvastatin 10 or 80 mg/day and were followed for a median of 4.9 years.
Patients with a known left ventricular ejection fraction <30% or symptoms of advanced HF (New York Heart Association class IIIb or IV) were excluded from the study, as were those with nephrotic syndrome. Of 10,001 subjects enrolled in TNT, 625 were excluded according to the following criteria (310 in atorvastatin 10-mg group, 315 in 80-mg group): missing baseline eGFR data (n = 345), missing year-1 eGFR (n = 229), and death or HF hospitalization before 1 year (n = 51), leaving 9,376 subjects for this analysis.
The main end point of this analysis was hospitalization with a primary diagnosis of HF, which was a prespecified secondary efficacy outcome of TNT. Hospitalization for HF was defined according to the following criteria: (1) the patient was hospitalized with a primary admission diagnosis of HF and demonstrated symptoms and signs consistent with this clinical diagnosis, (2) cause of HF was related to impaired left ventricular emptying or filling characteristics, and (3) cause of HF was not temporally related to an acute myocardial infarction. An independent end-point committee blinded to treatment assignment adjudicated all potential end-point events.
Serum creatinine was measured and eGFR was estimated using the Modification of Diet in Renal Disease equation (eGFR in milliliters per minute per 1.73 m 2 = 175 × serum creatinine × age × 0.742 if a woman, × 1.212 if African-American) as recommended by the National Kidney Foundation Kidney Disease Outcomes Quality Initiative.
Baseline characteristics were depicted by treatment group (high- vs low-dose atorvastatin) and by subsequent HF hospitalization status. Renal function between treatment groups and subsequent HF hospitalization status were compared using 2-sample t tests for baseline and year-1 eGFR measurements. Change in year-1 eGFR was compared within and between groups using least squares means and analysis of covariance models with treatment group as the major predictor and baseline eGFR as the covariate. Cox proportional hazards regression was used to assess the effect of change in year-1 eGFR on subsequent HF hospitalization. Nested models were created, adjusting for baseline eGFR, treatment, and change in LDL cholesterol from baseline to year 1. Based on previous data showing a significant treatment effect on subsequent HF hospitalization, analyses were repeatedly stratified by treatment. The potential interaction of treatment group and year-1 eGFR was tested.
Results
Of the 9,376 patients included in this analysis, 218 underwent HF hospitalization after 1 year, 100 of 4,680 in the atorvastatin 80-mg group and 118 of 4,696 in the 10-mg group (2.1% vs 2.5%, hazard ratio [HR] 0.85, 95% confidence interval [CI] 0.65 to 1.11, p = 0.23). Clinical characteristics of patients with and without HF hospitalization after 1 year are listed in Table 1 . Clinical features of patients in the 10- and 80-mg groups were similar. There was no significant difference in proportion of patients with previous HF between treatment groups (7.5% in atorvastatin 10-mg group vs 7.2% in 80-mg group, p = 0.61). About 1/3 of participants who developed subsequent HF had a history of HF. Participants who had subsequent HF hospitalizations were older and had a higher prevalence of cardiovascular risk factors including previous HF, diabetes mellitus, hypertension, and peripheral arterial disease. In addition, those with subsequent HF were less frequently treated with β blockade and more frequently treated with angiotensin-converting enzyme inhibitors, aldosterone blockade, and diuretics.
| Characteristic | HF | No HF | ||
|---|---|---|---|---|
| (n = 218) | (n = 9,158) | |||
| Atorvastatin 10 mg | Atorvastatin 80 mg | Atorvastatin 10 mg | Atorvastatin 80 mg | |
| (n = 118) | (n = 100) | (n = 4,578) | (n = 4,580) | |
| Age (years) | 65.9 ± 6.9 | 65.3 ± 7.3 | 60.7 ± 8.9 | 61.1 ± 8.7 |
| Men | 91 (77%) | 74 (74%) | 3,713 (81%) | 3,743 (82%) |
| Caucasian race | 115 (98%) | 88 (88%) | 4,314 (94%) | 4,327 (95%) |
| Systolic blood pressure (mm Hg) | 136 ± 19 | 136 ± 18 | 131 ± 17 | 131 ± 17 |
| Diastolic blood pressure (mm Hg) | 77 ± 9 | 76 ± 11 | 78 ± 10 | 78 ± 9 |
| Body mass index (kg/m 2 ) | 30.1 ± 5.4 | 29.7 ± 5.5 | 28.6 ± 4.6 | 28.4 ± 4.4 |
| Current smoker | 18 (15%) | 17 (17%) | 605 (13%) | 582 (13%) |
| Heart failure | 46 (39%) | 29 (29%) | 304 (7%) | 306 (7%) |
| Hypertension | 94 (80%) | 77 (77%) | 2,428 (53%) | 2,441 (53%) |
| Diabetes mellitus | 45 (38%) | 45 (45%) | 642 (14%) | 649 (14%) |
| Myocardial infarction | 71 (60%) | 66 (66%) | 2,631 (58%) | 2,685 (59%) |
| Cerebrovascular accident | 18 (15%) | 11 (11%) | 224 (5%) | 221 (5%) |
| Peripheral arterial disease | 31 (26%) | 37 (37%) | 493 (11%) | 528 (12%) |
| Coronary revascularization | ||||
| Angioplasty | 62 (53%) | 54 (54%) | 2,499 (55%) | 2,460 (54%) |
| Bypass surgery | 76 (64%) | 66 (66%) | 2,103 (46%) | 2,112 (46%) |
| β Blocker | 53 (45%) | 48 (48%) | 2,471 (54%) | 2,491 (54%) |
| Angiotensin-converting enzyme inhibitor | 55 (45%) | 53 (53%) | 1,201 (26%) | 1,225 (27%) |
| Angiotensin receptor blocker | 16 (14%) | 9 (9%) | 238 (5%) | 224 (5%) |
| Aldosterone antagonist | 23 (20%) | 24 (24%) | 77 (2%) | 75 (2%) |
| Aspirin | 87 (74%) | 73 (73%) | 3,982 (87%) | 3,991 (87%) |
| Diuretic | 53 (45%) | 51 (51%) | 608 (13%) | 589 (13%) |
| Calcium channel blockers | 35 (30%) | 47 (47%) | 1,175 (26%) | 1,251 (27%) |
| Antiplatelet therapy | 3 (3%) | 3 (3%) | 137 (3%) | 141 (3%) |
| Lipids (mg/dl) | ||||
| Low-density lipoprotein cholesterol | 98 ± 19 | 100 ± 16 | 98 ± 18 | 97 ± 17 |
| Total cholesterol | 178 ± 22 | 176 ± 23 | 174 ± 24 | 175 ± 24 |
| Triglycerides | 180 ± 76 | 155 ± 76 | 149 ± 71 | 150 ± 69 |
| High-density lipoprotein cholesterol | 44 ± 9 | 45 ± 11 | 47 ± 11 | 48 ± 11 |
| Baseline estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 55.8 ± 13.6 | 63.1 ± 12.6 | 65.7 ± 11.5 | 65.1 ± 11.2 |
Despite being significantly lower at baseline, eGFR values were higher at 1 year in the atorvastatin 80-mg compared to the 10-mg group (p = 0.0002), as shown in Table 2 . Little change occurred in eGFR from baseline to 1 year with atorvastatin 10 mg (p = 0.29), whereas significant improvement in 1-year eGFR was observed with atorvastatin 80 mg (least squares means 1.48 ml/min/1.73 m 2 , 95% CI 1.29 to 1.67; p <0.0001). Improvement in eGFR from baseline to 1 year was greater with atorvastatin 80 mg compared to 10 mg (1.52 ± 7.02 vs 0.07 ± 6.77, p <0.0001). The 5-year change in eGFR in the 2 groups was incrementally higher, suggesting time- and dose-dependent increases, which met statistical significance (data not shown).
| Variable | Atorvastatin 10 mg | Atorvastatin 80 mg | Total | p Value ⁎ |
|---|---|---|---|---|
| (n = 4,696) | (n = 4,680) | (n = 9,376) | ||
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | ||||
| Baseline | 65.6 ± 11.4 | 65.0 ± 11.3 | 65.3 ± 11.3 | 0.018 |
| 1 year | 65.7 ± 11.8 | 66.6 ± 11.9 | 66.1 ± 11.9 | 0.0002 |
| Change from baseline to 1 year | 0.1 ± 6.8 | 1.5 ± 7.0 | 0.8 ± 6.9 | <0.0001 |
| Comparison of 1 year to baseline within treatment group † | 0.10 (−0.09 to 0.30) | 1.48 (1.29–1.67) | 0.79 (0.65–0.93) | |
| p Value | 0.29 | <0.0001 | <0.0001 |
⁎ Values for between-treatment estimated glomerular filtration rate were based on 2-sample t tests.
† Values are presented as least square means or means difference (95% confidence interval); values for within- and between-treatment comparisons were based on an analysis of covariance model comparing patients with to those without heart failure hospitalization that was adjusted for baseline estimated glomerular filtration rate.
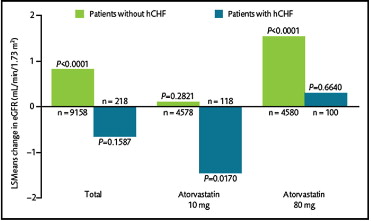
As presented in Table 3 , baseline and year-1 eGFR were significantly lower in patients with subsequent HF hospitalization compared to those without HF. Subsequent HF hospitalization was preceded by a decrease in eGFR over 1 year compared to modest improvement in those without subsequent HF. Mean difference between the 2 groups for change in eGFR at 1 year was 1.47 ml/min/1.73 m 2 (p = 0.0015). Changes in patients with and without subsequent HF per atorvastatin treatment group are depicted in Figure 1 . In the 10-mg group, eGFR did not change over 1 year in patients without HF but decreased in patients with subsequent HF hospitalization (p = 0.017); in the 80-mg group, eGFR increased in patients without HF (p <0.0001) but did not change significantly in patients with subsequent HF.
| Variable | HF Hospitalization | p Value ⁎ | |
|---|---|---|---|
| No | Yes | ||
| (n = 9,158) | (n = 218) | ||
| Modification of Diet in Renal Disease estimated glomerular filtration rate (ml/min/1.73 m 2 ) | |||
| Baseline | 65.4 ± 11.2 | 61.3 ± 13.9 | <0.0001 |
| 1 year | 66.2 ± 11.8 | 61.2 ± 14.5 | <0.0001 |
| Change from baseline to 1 year | 0.8 ± 6.9 | −0.1 ± 7.9 | 0.0015 |
| Comparison of 1 year to baseline within treatment group † | 0.82 (0.69–0.96) | −0.65 (−1.54 to 0.25) | |
| p Value | <0.0001 | 0.16 | |
⁎ Values for between-treatment estimated glomerular filtration rate were based on 2-sample t tests.
† Least square means or means difference (95% confidence interval) for within- and between-treatment comparisons were based on an analysis of covariance model comparing patients with to those without heart failure hospitalization that was adjusted for baseline estimated glomerular filtration rate.
After adjusting for baseline eGFR, each 5-ml/min/1.73 m 2 increase in eGFR from baseline to year 1 was associated with a lower risk of subsequent HF hospitalization (HR 0.85, 95% CI 0.77 to 0.94, p = 0.002), as presented in Table 4 . This effect remained significant after adjustments were made for randomized treatment assignment and/or change in LDL cholesterol levels at 1 year. Conversely, after adjusting for baseline and 1-year change in eGFR, treatment effect and 1-year change in LDL cholesterol levels were no longer predictive of subsequent HF hospitalization. There was no significant interaction between treatment and 1-year change in eGFR (p = 0.89).



