Fragmented QRS (fQRS) on 12-lead electrocardiography reflects conduction delay caused by myocardial fibrosis and dysfunction. Ventricular fibrosis detected by late gadolinium enhancement (LGE) cardiac magnetic resonance (CMR) is reportedly correlated with worse clinical outcomes in adults with repaired tetralogy of Fallot (TOF). The aim of this study was to assess whether the presence of fQRS is associated with right ventricular (RV) fibrosis or dysfunction in this patient group. In 37 consecutive patients (median age 30 years, median age at repair 6.6 years), the number of leads showing fQRS, defined as the presence of >2 notches on the R/S wave in ≥2 contiguous leads, was counted. RV systolic function, dilatation, and LGE score were measured using LGE CMR. Ventricular LGE was observed mainly at the previous surgical sites: the RV outflow tract (33 of 37), ventricular septal defect patch region (15 of 37), and RV anterior wall (11 of 37). Fragmented QRS was found mostly in the right and mid precordial leads. The fQRS group (n = 20) demonstrated higher RV LGE scores (p <0.001) and lower RV ejection fractions (p = 0.02) and a trend toward larger RV end-diastolic and end-systolic volumes (p = 0.12 and p = 0.06, respectively) compared to the non-fQRS group (n = 17). The number of electrocardiographic leads showing fQRS was positively correlated with RV LGE score (r = 0.75, p <0.001). The presence of fQRS remained independently associated with the presence of supramedian RV LGE score, even after adjusting for relevant parameters. In conclusion, fQRS was closely associated with more extensive RV fibrosis and dysfunction in adults with repaired tetralogy of Fallot.
QRS complexes on surface electrocardiography show fragmented morphology in some patients late after repair of tetralogy of Fallot (TOF). Fragmented QRS (fQRS) has been shown to indicate myocardial scarring, leading to inhomogenous conduction delays in patients with ischemic or nonischemic heart disease. However, no data exist regarding the relation of fQRS to ventricular fibrosis and dysfunction detected by late gadolinium enhancement (LGE) cardiac magnetic resonance (CMR) in adults with repaired TOF. The aim of this study was to investigate the relation between the presence of fQRS on 12-lead electrocardiography and right ventricular (RV) fibrosis or dysfunction detected by LGE CMR.
Methods
Thirty-seven consecutive patients were enrolled for the present study who met all the following criteria: (1) they were >15 years of age, (2) ≥10 years had elapsed since their corrective surgery for TOF, and (3) they had undergone LGE CMR examinations at Samsung Medical Center from May 2004 to May 2010 to ascertain the necessity of redo surgery because of increases in heart size or worsening symptoms such as exercise intolerance or palpitation. We excluded patients if the LGE protocol was not incorporated in their CMR studies or if image quality was inadequate for assessing the presence of LGE. Of the 37 patients, 26 had undergone transannular patch, 6 RV outflow tract (RVOT) patch, and 3 RV–to–pulmonary artery conduit insertion. The remaining 2 patients had undergone subpulmonary resection only. The study protocol was approved by the institutional review board of Samsung Medical Center, and the requirement for written informed consent was waived.
To assess the relation of fQRS to ventricular LGE, an electrocardiogram recorded before LGE CMR was analyzed. The time interval between the electrocardiographic and CMR examinations ranged from 0.1 to 1.0 month (median 0.6 months). Standard 12-lead electrocardiograms were obtained with an optimal low-pass filter setting (filter range 0.15 to 100 Hz, alternating current filter 60 Hz, 25 mm/s, 10 mm/mV; GE Marquette, Milwaukee, Wisconsin).
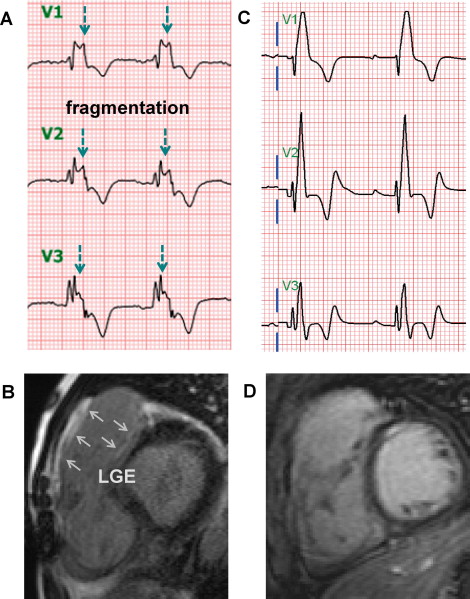
QRS morphology late after repair of TOF usually shows a right bundle branch block pattern. Therefore, QRS complexes were defined as fragmented when >2 notches in the R/S wave were present (≥1 notch more than the typical right bundle branch block pattern; Figure 1 ) in ≥2 contiguous anterior (V 1 to V 5 ), inferior (II, aVF, and III), or lateral (I, aVL, and V 6 ) leads. The extent of fQRS in each patient was estimated by counting the number of electrocardiographic leads with fQRS. Electrocardiograms were reviewed without using any magnification by 2 independent readers who were blinded to CMR and clinical data. There was 98% and 96% intra- and interobserver agreement for the presence of fQRS, respectively. Electrocardiographic parameters such as QRS duration and QRS, QT, and JT dispersion were also measured. As for QRS duration, the broadest QRS width in any lead was measured from the earliest to the latest signal crossing the isoelectric line.
The detailed LGE CMR protocol used in this study was described in previous studies. In brief, all scans were obtained using a 1.5-T scanner (Achieva; Philips Medical Systems, Best, The Netherlands). Cine images were obtained using a fast gradient-echo sequence (balanced fast field echo, steady-state free precession) along the long and the short axis from the apex to the base of the right and left ventricles. Pulmonary regurgitation volume and fraction were assessed by measuring anterograde and retrograde flow in the main pulmonary artery using a free-breathing, electrocardiographically triggered, cine phase velocity pulse sequence. Volumetric variables were computed using Simpson’s algorithm from the short-axis images acquired at end-diastole and end-systole during brief periods of breath-holding. They were adjusted for body surface area to obtain the RV and left ventricular (LV) end-diastolic volume index, end-systolic volume index, mass index, and ejection fraction. The RVOT region was included as we calculated the RV volumes or mass index. Delayed hyperenhancement was evaluated 5 to 15 minutes after the intravenous injection of 0.15 mmol/kg gadolinium-diethylenetriamine pentaacetic acid (Magnevist; Bayer Schering Pharma AG, Berlin, Germany) in 10 to 12 contiguous slices of 6-mm thickness with a 4-mm interslice gap. We used a multishot turbo field echo breath-hold sequence with a nonselective inversion (repetition time 4.6 ms, echo time 1.4 ms). A Look-Locker sequence was used to determine the optimal inversion time for nulling of healthy myocardium, which varied from 200 to 300 ms. RV long-axis planes including a sagittal RVOT and RV oblique and 4-chamber views were also obtained. The field-of-view and image matrix were 35 × 35 cm and 256 × 256, respectively.
To quantify the extent of RV LGE, the residual volume was divided into 6 segments: the RVOT, RV anterior wall, RV inferior wall, septum, ventricular septal defect patch region, and trabecular bands. LGE for each segment was scored from 0 to 3 depending on its linear extent or number of enhanced trabeculations: 0 = no LGE, 1 = up to 2 cm, 2 = 2 to 3 cm, and 3 = >3 cm in length. LGE in trabeculations was scored as follows: 0 = no LGE, 1 = LGE of 1 trabeculation, 2 = LGE of 2 to 4 trabeculations, and 3 = LGE of >4 trabeculations, respectively. Therefore, total RV LGE score ranged from 0 to 18. LGE in LV or RV-LV insertion points was not incorporated in the analysis as with the previous studies. Two expert radiologists who were blinded to the clinical and electrocardiographic information independently analyzed LGE, and there was 93% and 96% intra- and interobserver agreement for the presence of RV LGE, respectively.
Continuous variables are presented as medians with interquartile ranges and were compared using Mann-Whitney U tests. The results for categorical variables are described as percentages, and Fisher’s exact tests were used to compare these results. Correlation between the extent of fQRS and RV LGE score was assessed using Spearman’s rank correlation coefficient. Multivariate analyses were performed using logistic regression to evaluate independent relations between fQRS and the presence of a high RV LGE score (supramedian). All statistical analyses were performed using PASW Statistics version 18 Windows (SPSS, Inc., Chicago, Illinois). All p values were 2 sided, and results with p values <0.05 were considered statistically significant.
Results
Table 1 summarizes the baseline characteristics of the 37 patients. Median ages at TOF repair and at enrollment were 6.6 and 30 years, respectively. More than 20 years had elapsed from TOF repair (median 22.9, range 13.6 to 39.2).
| Variable | All Patients | Non-fQRS Group | fQRS Group | p Value |
|---|---|---|---|---|
| (n = 37) | (n = 17) | (n = 20) | ||
| Men | 16 (43%) | 7 (41%) | 9 (45%) | 1.00 |
| Age (years) | 30.0 (23.3–40.0), 15.8–66.4 | 27.4 (20.6–36.2) | 34.5 (26.9–42.0) | 0.13 |
| Age at TOF repair (years) | 6.6 (3.0–10.8), 0.7–27.2 | 6.1 (1.5–9.7) | 7.9 (4.6–12.2) | 0.19 |
| Time from TOF repair (years) | 22.9 (19.9–28.8), 13.6–39.2 | 22.3 (19.4–25.3) | 25.8 (20.0–29.4) | 0.15 |
| New York Heart Association class I | 26 (70%) | 13 (77%) | 13 (65%) | 0.49 |
| Maximum V o 2 (ml/kg/min) | 28 (22–34), 16–54 | 27 (22–36) | 29 (21–34) | 0.59 |
Ventricular LGE was detected in most patients (35 of 37) who underwent LGE CMR, usually at the previous surgical sites, including the RVOT, ventricular septal defect patch region, and RV anterior wall. However, the extent of RV LGE was quite variable among patients (RV LGE score range 0 to 13; Table 2 ) as well as over RV segments; the RVOT was the most common segment enhanced with gadolinium ( Figures 1 and 2 ) . The frequency of LGE is depicted according to each RV segment in Figure 2 . In contrast, the left ventricle revealed no significant enhancements, except for focal areas in the RV-LV insertion points. Therefore, LGE in LV or RV-LV insertion points was not incorporated in further analysis, as with the previous studies.
| Variable | All Patients | Non-fQRS Group | fQRS Group | p Value |
|---|---|---|---|---|
| (n = 37) | (n = 17) | (n = 20) | ||
| Electrocardiographic parameters | ||||
| QRS duration (ms) | 154 (144–165), 88–226 | 154 (124–164) | 155 (146–166) | 0.46 |
| QRS dispersion (ms) | 59 (50–73), 30–93 | 59 (50–70) | 62 (51–75) | 0.37 |
| QT dispersion (ms) | 62 (51–80), 11–146 | 68 (51–86) | 62 (37–79) | 0.37 |
| JT dispersion (ms) | 45 (34–45), 10–131 | 53 (37–75) | 42 (27–52) | 0.20 |
| Interval between electrocardiographic and CMR examinations (months) | 0.6 (0.1–1.0), 0-6.1 | 0.6 (0.3–0.9) | 0.6 (0.1–1.1) | 0.99 |
| CMR parameters | ||||
| RV LGE score | 5 (2–7), 0-13 | 2 (1–3.5) | 7 (5–8) | <0.001 |
| High RV LGE score (supramedian) | 15 (41%) | 2 (12%) | 13 (65%) | 0.002 |
| Pulmonary regurgitant fraction (%) | 37 (25–48), 2–93 | 37 (23–51) | 38 (25–47) | 0.82 |
| RV end-diastolic volume index (ml/m 2 ) | 131 (111–157), 79–318 | 124 (103–148) | 143 (115–176) | 0.12 |
| RV end-systolic volume index (ml/m 2 ) | 84 (69–103), 28–199 | 78 (59–94) | 94 (79–115) | 0.06 |
| RV ejection fraction (%) | 37 (30–43), 11–72 | 41 (36–49) | 35 (30–41) | 0.02 |
| Moderate to severe tricuspid regurgitation | 12 (32%) | 4 (24%) | 8 (40%) | 0.32 |
| LV end-diastolic volume index (ml/m 2 ) | 78 (65–94), 46–169 | 73 (58–114) | 78 (71–88) | 0.46 |
| LV end-systolic volume index (ml/m 2 ) | 36 (29–45), 14–135 | 37 (26–50) | 35 (31–42) | 0.52 |
| LV ejection fraction (%) | 53 (45–60), 20–69 | 56 (45–62) | 53 (45–59) | 0.46 |
Fragmented morphology of QRS complex was noted in 73 of 444 electrocardiographic leads from the 37 patients. In most of the leads showing fQRS (70 of 73), the fragmentation was located on the latter R (R′) wave of the QRS complex, with a right bundle branch block pattern ( Figure 1 ). Fragmented QRS was found mainly in the right and mid precordial leads, followed in frequency by the left precordial, inferior, and lateral leads ( Figure 2 ). The extent of fQRS, defined by the number of leads with fQRS, showed a positive correlation with RV LGE score (r = 0.75, p <0.001; Figure 3 ) .




