Studies linking depressive symptoms and coronary artery calcium (CAC), a measure of subclinical atherosclerosis, have yielded mixed results. No longitudinal studies of depressive symptoms and CAC have included older adults of both genders. This study examined the association of depressive symptoms with CAC and CAC progression in older men and women. Participants were 417 community-dwelling older adults (mean age = 67 ± 7) with no history of heart disease who attended a 1997 to 1999 research clinic visit when depressive symptoms were assessed using the Beck Depression Inventory (BDI). CAC was measured using electron-beam computed tomography in 2000 to 2002 and again in 2005 to 2007. Median BDI was 3, range = 0 to 37; 39% of men and 10% of women had severe CAC (Agatston score ≥400) in 2000 to 2002. Ordinal logistic regression analyses examining the odds of greater compared with lesser CAC severity by BDI quartiles showed an unexpected negative association whereby women with the lowest depressive symptoms had 2.4 times the odds of increasing CAC severity compared with women in the second BDI quartile (95% CI 1.1 to 5.4). A nonlinear, U-shaped association was observed in men with those in the first and fourth BDI quartiles having 2.6 and 3.0 times higher odds of increasing CAC severity than subjects in the second quartile (95% CI 1.2 to 5.6 and 1.3 to 6.9, respectively) after adjustment for coronary heart disease risk factors. No significant associations were observed for CAC progression although similar nonlinear patterns were observed in men. In conclusion, our results suggest that depressive symptoms have a gender-specific, cross-sectional association with CAC but no statistically significant associations with CAC progression.
Coronary artery calcium (CAC) is a marker of subclinical atherosclerosis that independently predicts coronary heart disease (CHD) risk, future coronary events, and stroke. Although the evidence establishing depression as an independent risk factor for CHD is not conclusive, a recent meta-analysis found depression increased the risk by 80%. Depressive symptoms, not always severe enough to meet thresholds indicative of clinical depression, have been identified as an independent risk factor for CHD in older adults (>65 years). A body of research has emerged testing the hypothesis that depressive symptoms increase the risk of CHD through an association with CAC. Results from cross-sectional analyses are mixed with 3 studies reporting null associations, 2 reporting negative associations, and 2 reporting positive associations. Longitudinal studies of CAC progression in middle-aged adults have shown that greater depressive symptoms are associated with greater CAC progression. The only study of depressive symptoms and CAC progression in older adults included only women and did not find statistically significant associations. To our knowledge, no study has examined the association of CAC progression and depressive symptoms in a community-based population of older women and men. Therefore, we examined the associations of depressive symptoms, CAC, and CAC progression in older men and women with repeat CAC assessments 4.5 ± 0.5 years apart. We hypothesized that greater levels of depressive symptoms would be cross-sectionally associated with greater CAC severity and that subjects with greater baseline levels of depressive symptoms would experience greater CAC progression.
Methods
Data used in analyses were from participants of the Rancho Bernardo Study, a prospective population-based cohort study of heart disease risk factors that began in 1972 to 1974 when 6,629 Caucasian middle class adults from a Southern California community were enrolled. From 1997 to 1999, 1,096 adults, representing 77% of surviving participants, attended a research clinic visit when depressive symptoms were assessed. From 2000 to 2001, 525 of these attendees were contacted to have chest electron-beam computed tomography (EBCT) screening for coronary artery calcium. Eligible participants were (1) evaluated by our research team from 1997 to 1999, (2) postmenopausal (>1 year without menses) if women, and (3) free of clinically manifest CHD (no physician-diagnosed angina, myocardial infarction, or coronary artery revascularization). Of the 525 contacted, 2 were deceased, 15 were ineligible because of clinically manifest CHD, 38 declined to participate, and 48 were not seen because of scheduling problems. The 86 men and women who were eligible but did not participate were similar in age, gender, and depression symptom scores to the 422 men and women who participated. Five participants were excluded from analyses for missing Beck Depression Inventory (BDI) measurements. From 2005 to 2007, 323 (176 women and 147 men) of the originally screened participants still without clinically manifest CHD returned for a follow-up CAC scan. Reasons for not returning included refusal (n = 43), death (n = 21), and unknown (n = 35). The study protocol was approved by the Human Research Protections Program at the University of California, San Diego. Written consent was obtained before participation at all 3 visits.
Depressive symptoms were assessed during the 1997 to 1999 research clinic visit using the self-administered BDI. The BDI consists of 21 items, each assessing symptoms and attitudes related to depression. Respondents rated each item from 0 (lowest intensity) to 3 (highest intensity), and the scores were summed to quantify depressive symptomology. The BDI has high internal consistency in nonpsychiatric patients and adequate reliability in older adults.
Anthropometric measurements made during the 1997 to 1999 clinic visit included height, weight, and waist and hip circumference. Body mass index was used as an estimate of overall obesity, whereas waist-to-hip ratio was used as an estimate of central adiposity. Blood pressure was measured twice in seated participants after 5 minutes of rest using the Hypertension Detection and Follow-up Program protocol ; the average measurements were used. Hypertension was defined as systolic blood pressure >140 mm Hg, diastolic blood pressure >90 mm Hg, or reported use of antihypertensive medication.
Plasma glucose, triglycerides, total cholesterol, and high density and low density lipoprotein (LDL) were assessed using standard methods after a requested 12 to 16-hour overnight fast. Age, alcohol use (drinks per day), cigarette smoking (never, past, or present), and exercise (≥3 times per week, no/yes) were obtained by standardized questionnaire. Medication use, including antidepressant, statin and estrogen use, was queried and validated by trained nurses who reviewed prescriptions and pill containers brought to the clinic for that purpose.
CAC was measured using chest EBCT scans at 2 clinic visits, EBCT1 (2000 to 2002) and EBCT2 (2005 to 2007). An Imatron C-150 scanner took 40 contiguous images while participants held a single breath. CAC was defined as a plaque of ≥2 pixels (area 0.67 mm 2 ) with a density of ≥130 Hounsfield units. Calcium scores used to classify adults by CAC severity were calculated using the method of Agatston et al. Total volume scores (mm 3 ) were calculated as the sum of volume scores for each lesion. Data on visceral and subcutaneous fat (assessed by EBCT) as well as statin use were obtained at each EBCT visit.
Substantial gender differences in CAC severity suggested stratified analyses of men and women were appropriate; subsequent tests of effect modification confirmed this (p = 0.08). Participants were grouped into gender-specific quartiles on the basis of BDI scores. The methods of Rumberger et al were used to group participants by CAC severity: Agatston scores of 0 to 10 = minimal; 11 to 100 = mild; 101 to 399 = moderate; and ≥400 = severe. A binary indicator of CAC progression was computed using the method proposed by Hokanson et al in which the difference in the square root–transformed total calcium volume scores are computed and differences ≥2.5 mm 3 are considered progression. The Hokanson method is considered the best measure of CAC progression.
Depressive symptoms, CAC, and potential covariates were described using age-adjusted means (for continuous variables) or percentages (for categorical variables). Comparisons of CAC and potential covariates across BDI quartiles were assessed using a Wald test. Covariates were selected for inclusion on the basis of known risk factors for CAC.
Multivariate ordinal logistic regression models were fit using the ologit command to assess the odds of increasing CAC severity (an ordinal indicator of CAC) by BDI quartile. While assessing the functional form of BDI, we observed nonlinear patterns in men. Nonlinear relations were then tested by regressing CAC severity on the continuous and quadratic form of BDI and testing the null hypothesis that coefficients of the squared term were equal to zero. To satisfy the proportional odds assumption to complete tests for nonlinearity, one man and one woman with BDI scores >5 SDs from the overall mean were removed after which the assumption was met at the standard alpha of 0.10. Data for both older adults were included in all subsequent analyses using BDI quartiles. To evaluate nonlinear patterns, men and women in the second quartile were selected as the referent category. For all models, proportional odds assumptions were tested using the Brant test and were met at an alpha level of 0.10. Longitudinal analyses of CAC progression followed the same approach described previously using multivariate logistic regression models fit using the logistic command.
Associations of BDI with CAC severity and progression were examined using 4 sequential models: model 1 adjusted for age and follow-up time; model 2 added LDL and fasting plasma glucose; model 3 added visceral fat and statin use to model 2; model 4 added a measure of the number of alcohol drinks per week to model 3. CAC severity models used age, statin use, and visceral fat assessed at EBCT1 and time from baseline to EBCT1. CAC progression models used age, statin use, and visceral fat measured at EBCT2 and time between the first and second EBCT measurements. Estimates were unchanged when total cholesterol was included in models instead of LDL; therefore, LDL was retained for analyses. Full models were tested for multicollinearity and all variance inflations factors were <5. All data were analyzed using Stata, version 11.2. Alpha levels were set to 0.05 unless otherwise stated.
Results
Average baseline age of participants was 67 ± 7.2 years. A total of 417 participants underwent CAC screening (EBCT1) 2.3 ± 1.0 years after the baseline visit and 326 returned for EBCT2 4.5 ± 0.5 years later. Age and age-adjusted characteristics are provided in Table 1 .
| Baseline visit (1997-1999) | Men (n = 199) | Women (n = 218) | p-value |
|---|---|---|---|
| Age (years) ∗ | 70 (0.6) | 66 (0.4) | < 0.01 |
| Ever smoker | 60% | 51% | 0.46 |
| Exercise >3 days per week | 79% | 76% | 0.41 |
| Alcoholic drinks per week | 7.5 (0.46) | 4.4 (0.44) | < 0.01 |
| Body mass index (kg/m 2 ) | 27 (0.3) | 26 (0.3) | < 0.01 |
| Waist to hip ratio | 0.9 (0.01) | 0.8 (0.00) | < 0.01 |
| Low density lipoprotein (mg/dl) | 122 (2.1) | 123 (2.0) | 0.58 |
| High density lipoprotein (mg/dl) | 50 (1.0) | 67 (1.0) | < 0.01 |
| Total cholesterol (mg/dl) | 197 (2.3) | 216 (2.2) | < 0.01 |
| Triglycerides (mg/dl) | 126 (4.8) | 130 (4.6) | 0.71 |
| Fasting plasma glucose (mg/dl) | 107 (1.4) | 99 (1.3) | < 0.01 |
| Systolic blood pressure (mm Hg) | 131 (1.3) | 130 (1.2) | 0.93 |
| Diastolic blood pressure (mm Hg) | 78 (0.6) | 75 (0.6) | < 0.01 |
| Hypertension | 48% | 47% | 0.84 |
| Antidepressant use | 7.1% | 11.3% | 0.15 |
| Beck Depression Index | 3.7 (0.29) | 4.4 (0.28) | 0.10 |
| Depressed (% with BDI > 12) | 2.7 (1.20) | 3.9 (1.30) | 0.47 |
| EBCT1 visit (2000-2002) | (n = 199) | (n = 218) | |
|---|---|---|---|
| Age (years) ∗ | 71 (0.6) | 68 (0.5) | < 0.01 |
| Time from baseline to EBCT1 (years) | 2.2 (0.04) | 2.4 (0.03) | < 0.01 |
| Statin use | 22% | 14% | 0.05 |
| Visceral fat (cm 3 ) | 94 (4) | 61 (4) | < 0.01 |
| Subcutaneous fat (cm 3 ) | 128 (5.4) | 151 (5.2) | < 0.01 |
| EBCT2 visit (2005-2007) | (n = 147) | (n = 176) | |
|---|---|---|---|
| Age (years) ∗ | 74 (0.7) | 72 (0.5) | 0.01 |
| Time from EBCT1 to EBCT2 (years) | 4.5 (0.03) | 4.4 (0.03) | 0.03 |
| Statin use | 40% | 28% | 0.02 |
| Visceral fat (cm 3 ) | 108 (4) | 72 (3) | < 0.01 |
| Subcutaneous fat (cm 3 ) | 135 (5) | 141 (5) | 0.33 |
| Coronary Artery Calcium progression | 55% | 39% | < 0.01 |
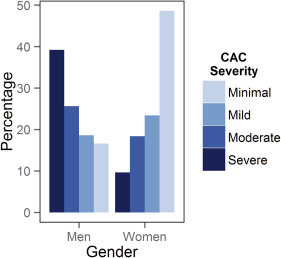
Figure 1 shows the distribution of CAC severity for men and women separately. Nearly 50% of women had minimal CAC compared to 17% for men. Conversely, the largest proportion of men had severe CAC (39%), whereas only 10% of women had severe CAC.
Demographic, behavioral, clinical, and anthropometric characteristics across BDI quartiles were compared separately for men and women. Notable significant differences in men were LDL and total cholesterol, which followed a U-shaped pattern with the highest mean values observed in men in the first and fourth BDI quartiles ( Table 2 ). Among women, age varied significantly by BDI quartile at baseline and EBCT1 (p <0.05; Table 3 ). Antidepressant use also differed (p = 0.01) with 25% of women in the fourth BDI quartile using depression medication compared to 7%, 5%, and 9% in the first, second, and third quartiles, respectively.
| Baseline visit (1997-1999) | Quartile, Beck Depression Inventory Range | p-value † | |||
|---|---|---|---|---|---|
| I, 0-1 (n = 64) | II, 2-3 (n = 53) | III, 4-5 (n = 51) | IV, 6-37 (n = 31) | ||
| Age (years) ∗ | 68 (1.0) | 69 (1.0) | 69 (1.1) | 70 (1.4) | 0.48 |
| Ever smoker | 43% | 60% | 51% | 81% | 0.01 |
| Exercise >3 days per week | 85% | 79% | 83% | 67% | 0.21 |
| Alcoholic drinks per week | 7.1 (0.9) | 7.3 (1.0) | 7.7 (1.1) | 8.6 (1.4) | 0.81 |
| Body mass index (kg/m 2 ) | 27 (0.4) | 27 (0.5) | 27 (0.5) | 27 (0.6) | 0.93 |
| Waist to hip ratio | 0.9 (0.01) | 0.9 (0.01) | 0.9 (0.01) | 0.9 (0.01) | 0.73 |
| Low density lipoprotein (mg/dl) | 126 (3.7) | 113 (4.0) | 120 (4.1) | 129 (5.2) | 0.04 |
| High density lipoprotein (mg/dl) | 50 (1.5) | 50 (1.7) | 51 (1.7) | 51 (2.2) | 0.96 |
| Total cholesterol (mg/dl) | 201 (3.9) | 187 (4.3) | 196 (4.4) | 206 (5.6) | 0.03 |
| Triglycerides (mg/dl) | 128 (8.7) | 122 (9.6) | 126 (9.8) | 130 (12.5) | 0.96 |
| Fasting plasma glucose (mg/dl) | 106 (2.1) | 110 (2.3) | 105 (2.4) | 106 (3.1) | 0.32 |
| Systolic blood pressure (mm Hg) | 129 (2.2) | 132 (2.5) | 136 (2.5) | 130 (3.2) | 0.20 |
| Diastolic blood pressure (mm Hg) | 77 (1) | 79 (1.1) | 80 (1.1) | 80 (1.4) | 0.17 |
| Hypertension | 43% | 49% | 55% | 61% | 0.32 |
| Antidepressant use | 0% | 8% | 10% | 16% | 0.47 |
| Beck Depression I nventory | 0.4 (0.3) | 2.5 (0.3) | 4.9 (0.3) | 10.8 (0.4) | <0.01 |
| EBCT1 visit (2000-2002) | (n = 64) | (n = 53) | (n = 51) | (n = 31) | |
|---|---|---|---|---|---|
| Age (years) ∗ | 70 (1.0) | 71 (1.1) | 72 (1.3) | 73 (1.5) | 0.43 |
| Time from baseline to EBCT1 (years) | 2.3 (0) | 2.4 (0.1) | 2.4 (0.1) | 2.5 (0.1) | 0.13 |
| Statin use | 23% | 18% | 20% | 29% | 0.07 |
| Visceral fat (cm 3 ) | 100 (8.3) | 86 (9.1) | 94 (9.5) | 91 (11.8) | 0.73 |
| Subcutaneous fat (cm 3 ) | 135 (10.0) | 116 (11.0) | 118 (11.4) | 131 (14.2) | 0.53 |
| EBCT2 visit (2005-2007) | (n = 46) | (n = 41) | (n = 39) | (n = 21) | |
|---|---|---|---|---|---|
| Age (years) ∗ | 73 (1.1) | 75 (1.2) | 75 (1.3) | 74 (1.8) | 0.50 |
| Time from EBCT1 to EBCT2 (years) | 4.4 (0) | 4.5 (0) | 4.6 (0) | 4.5 (0.1) | 0.23 |
| Statin use | 35% | 32% | 32% | 36% | 0.27 |
| Visceral fat (cm 3 ) | 104 (6.8) | 111 (7.0) | 109 (7.3) | 115 (9.8) | 0.82 |
| Subcutaneous fat (cm 3 ) | 140 (8.5) | 119 (8.7) | 139 (9.1) | 136 (12.2) | 0.29 |
∗ Values are not adjusted for age.
† p Values from Wald tests after linear (continuous variables) or logistic (binary variables) regression.
| Baseline visit (1997-1999) | Quartile, Beck Depression Inventory Range | p-value † | |||
|---|---|---|---|---|---|
| I, 0-1 (n = 67) | II, 2-3 (n = 42) | III, 4-6 (n = 57) | IV, 7-27 (n = 52) | ||
| Age (years) ∗ | 65 (0.8) | 65 (0.9) | 67 (0.7) | 67 (0.9) | 0.03 |
| Ever smoker | 51% | 45% | 48% | 60% | 0.50 |
| Exercise >3 days per week | 78% | 82% | 77%) | 60% | 0.07 |
| Alcoholic drinks per week | 4.0 (0.7) | 4.4 (0.8) | 4.7 (0.7) | 4.7 (0.7) | 0.89 |
| Body mass index (kg/m 2 ) | 25 (0.6) | 26 (0.7) | 26 (0.6) | 26 (0.6) | 0.44 |
| Waist to hip ratio | 0.8 (0.01) | 0.8 (0.01) | 0.8 (0.01) | 0.8 (0.01) | 0.28 |
| Low density lipoprotein (mg/dl) | 121 (3.7) | 129 (4.6) | 122 (4.0) | 123 (4.2) | 0.57 |
| High density lipoprotein (mg/dl) | 65 (2.1) | 63 (2.6) | 67 (2.2) | 71 (2.3) | 0.12 |
| Total cholesterol (mg/dl) | 212 (4.0) | 219 (5.0) | 215 (4.3) | 220 (4.5) | 0.47 |
| Triglycerides (mg/dl) | 126 (8.1) | 133 (10.2) | 136 (8.8) | 131 (9.2) | 0.87 |
| Fasting plasma glucose (mg/dl) | 98 (2.7) | 104 (3.4) | 96 (3.0) | 100 (3.1) | 0.44 |
| Systolic blood pressure (mm Hg) | 129 (2.3) | 128 (2.9) | 131 (2.5) | 129 (2.6) | 0.89 |
| Diastolic blood pressure (mm Hg) | 74 (1.0) | 77 (1.2) | 76 (1.1) | 75 (1.1) | 0.29 |
| Hypertension | 38% | 47% | 43% | 50% | 0.57 |
| Antidepressant use | 7% | 5% | 9% | 25% | 0.01 |
| Beck Depression Inventory | 0.3 (0.2) | 2.5 (0.3) | 5.1 (0.2) | 10 (0.3) | <0.01 |
| EBCT1 visit (2000-2002) | (n = 67) | (n = 42) | (n = 57) | (n = 52) | |
|---|---|---|---|---|---|
| Age (years) ∗ | 67 (0.9) | 67 (0.9) | 70 (0.8) | 69 (1.1) | 0.03 |
| Time from baseline to EBCT1 (years) | 2.3 (0.1) | 2.2 (0.1) | 2.2 (0.1) | 2.4 (0.1) | 0.18 |
| Statin use | 15% | 19% | 19% | 21% | 0.88 |
| Visceral fat (cm 3 ) | 55 (4.2) | 62 (5.2) | 68 (4.6) | 64 (4.7) | 0.22 |
| Subcutaneous fat (cm 3 ) | 136 (8.8) | 159 (10.8) | 159 (9.6) | 165 (9.9) | 0.12 |
| EBCT2 visit (2005-2007) | (n = 50) | (n = 35) | (n = 47) | (n = 44) | |
|---|---|---|---|---|---|
| Age (years) | 70 (0.9) | 71 (1.0) | 73 (0.8) | 73 (1.1) | 0.06 |
| Time from EBCT1 to EBCT2 (years) | 4.5 (0.1) | 4.5 (0.1) | 4.6 (0.1) | 4.4 (0.1) | 0.08 |
| Statin use | 30% | 29% | 26% | 28% | 0.75 |
| Visceral fat (cm 3 ) | 67 (5.7) | 78 (6.8) | 71 (5.9) | 70 (6.1) | 0.67 |
| Subcutaneous fat (cm 3 ) | 127 (9.3) | 152 (11.1) | 146 (9.7) | 150 (10.0) | 0.28 |
∗ Values are not adjusted for age.
† p Values from Wald tests after linear (continuous variables) or logistic (binary variables) regression.
Visual inspection of Figure 2 suggests a greater proportion of men and women in the first and fourth BDI quartiles (compared with those in the second and third quartiles) had severe CAC. A similar U-shaped trend was also apparent for moderate-to-severe CAC (Agatston scores >100) in men (but not women) with rates of 64% for those in BDI quartile 1, and 53%, 69%, and 81% for subjects in BDI quartiles 2, 3, and 4, respectively.
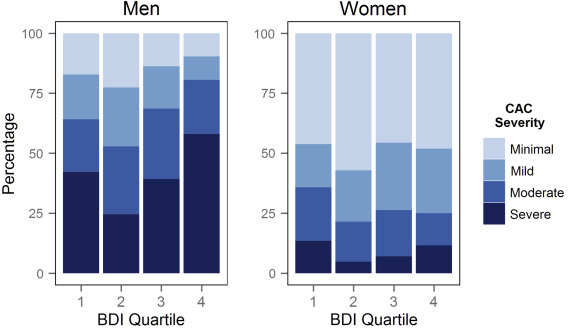
Results from multivariate ordinal logistic regression models corroborate the observed nonlinear associations in men. As listed in Table 4 , the fully adjusted odds for increasing CAC severity were 2.60 and 3.00 times higher for men in BDI quartiles 1 and 4 (compared with BDI quartile 2), respectively. Unexpected results were also observed in women, which indicated that those in the first BDI quartile had 2.39 times higher adjusted odds of increasing CAC severity compared to women in the second BDI quartile, with odds ratios near unity for quartiles 3 and 4. Results using BDI quartiles were corroborated using models that included the quadratic form of total BDI score (p values for the squared term are reported in Table 4 ), suggesting a significant U-shaped relation between BDI and the fully adjusted odds of increasing CAC severity for men (p = 0.01) but not for women (p = 0.20).
| Model 1 | Men | p- Value † | Women ∗ | p- value † | ||
|---|---|---|---|---|---|---|
| OR (n=199) | 95% CI | OR (n=217) | 95% CI | |||
| Beck Depression Inventory | 0.016 | 0.393 | ||||
| Quartile 1 | 2.28 | (1.15-4.52) | 2.19 | (0.99-4.83) | ||
| Quartile 2 | 1.00 | Referent | 1.00 | Referent | ||
| Quartile 3 | 2.28 | (1.06-4.89) | 1.01 | (0.45-2.27) | ||
| Quartile 4 | 2.88 | (1.33-6.26) | 1.13 | (0.49-2.62) | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


