The presence of a left dominant coronary artery system is associated with worse outcome after ST-segment elevation myocardial infarction (STEMI) compared with right dominance or a balanced coronary artery system. However, the association between coronary arterial dominance and left ventricular (LV) function at follow-up after STEMI is unclear. The present study aimed at evaluating the relation between coronary arterial dominance and LV ejection fraction (LVEF) shortly after STEMI and at 12-month follow-up. A total of 741 patients with STEMI (mean age 60 ± 11 years and 77% men) were evaluated with 2-dimentional echocardiography within 48 hours of admission (baseline) and at 12-month follow-up after STEMI. Coronary arterial dominance was assessed on the angiographic images obtained during primary percutaneous coronary intervention. A right, left, and balanced dominant coronary artery system was noted in 640 (86%), 58 (8%), and 43 (6%) patients, respectively. At baseline, significant difference in LV function was observed, with slightly lower LVEF in patients with a left dominant coronary artery system (LVEF 45 ± 8% vs 48 ± 9% and 50 ± 9%, for left dominant, right dominant, and balanced coronary artery system respectively, p = 0.03). However, at 12-month follow-up no differences in LV function or volumes were observed among the different coronary arterial dominance groups. In conclusion, patients with a left dominant coronary artery system had lower LVEF early after STEMI. At 12-month follow-up, differences in LVEF were no longer present among the different coronary arterial dominance groups.
Left ventricular (LV) systolic dysfunction and remodeling have been strongly associated with short- and long-term outcomes of patients with ST-segment elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PCI). Independent correlates of LV systolic dysfunction and remodeling after STEMI include infarct size, heart rate, and severity of coronary artery disease. The effect of coronary arterial dominance on LV dysfunction and remodeling at follow-up is unclear. A left dominant system, defined by the posterior descending artery (PDA) rising from the left circumflex (LCx) artery, increases by approximately 13% the odds in all-cause mortality after PCI. To obtain more insight into the relation between coronary arterial dominance and LV function, the present study aimed at evaluating the relation between coronary arterial dominance and LV function shortly after the index infarction and at 12-month follow-up.
Methods
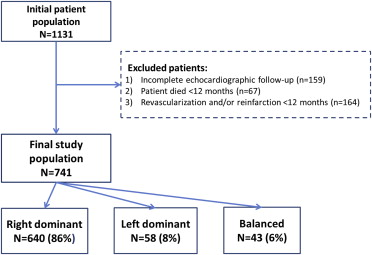
The present study population includes patients from an original cohort of patients with STEMI previously published. From 1,131 patients with a first STEMI who were admitted at the Leiden University Medical Center (Leiden, The Netherlands) from 2004 to 2008, 741 patients with completed echocardiographic examination at baseline (within 48 hours of admission) and at 12-month follow-up were included in the analysis ( Figure 1 ).
The diagnosis of STEMI was defined based on criteria of typical chest pain, elevated cardiac enzyme levels, and typical changes on the electrocardiogram. All patients were treated according to the institutional STEMI protocol, which includes primary PCI and optimal medical therapy initiated early during hospitalization. Circulating levels of creatine kinase and cardiac troponin T were systematically measured every 6 hours after primary PCI, until the highest levels were reached. Routine 2-dimensional echocardiography was performed within 48 hours of admission (baseline) and repeated at 12-month follow-up. The association between coronary arterial dominance, assessed during admission coronary angiography, and changes in LV volumes and ejection fraction at 12-month follow-up was evaluated.
Demographic, clinical, angiographic, and echocardiographic data were prospectively collected in the departmental cardiology information system (EPD-Vision, Leiden University Medical Center, Leiden, The Netherlands) and retrospectively analyzed.
The digitally stored images of the coronary angiography and PCI were obtained according to standardized angiographic projections. All coronary angiographic images of the primary PCI were retrospectively reviewed by 2 experienced observers. As previously described, coronary arterial dominance was defined according to the following definition: a coronary artery system was classified as right dominant if the PDA and posterolateral branch originated from the right coronary artery (RCA), left dominant if the PDA and the posterolateral branch originated from the LCx, and balanced if the PDA originated from the RCA in combination with posterolateral branches originating from the LCx artery. The extent of coronary artery disease was expressed as the presence of 1-, 2-, or 3-vessel disease (stenosis causing ≥50% luminal narrowing).
Images were obtained at rest with the patient in the left lateral decubitus position using a commercially available system (Vivid 7 and E9 [General Electric-Vingmed, Horten, Norway]). Data acquisition was performed with 3.5 MHz or M5S transducers in the standard parasternal and apical views. M-mode, 2-dimensional, and Doppler images were acquired during breath hold and saved in cine-loop format. Data analysis was performed offline with commercially available postprocessing data software, EchoPac 112.0.1 (GE Medical Systems, Horten, Norway).
LV function was assessed by tracing the LV end-systolic volume and end-diastolic volume in the apical 4- and 2-chamber views. Using the biplane Simpson’s method LV ejection fraction (LVEF) was calculated. Subsequently, the LV was divided into 16 segments to calculate the wall motion score index (WMSI). Every segment was individually assessed and scored based on its motion and systolic thickening ([1] normokinesia, [2] hypokinesia, [3] akinesia, and [4] dyskinesia). WMSI was calculated as the sum of the segment scores divided by the number of segments scored.
The continuous variables are presented as mean ± SD or as median and interquartile ranges. Categorical variables are presented as number and percentages. Differences in baseline characteristics among the 3 coronary arterial dominance groups (right dominance, left dominance, and balanced) were evaluated with the chi-square and 1-way analysis of variance tests with Bonferroni post hoc analysis for significant 1-way analysis of variance p values. Changes in LV volumes and LVEF from baseline to 12-month follow-up were evaluated using linear mixed model analyses. Subsequently, a mixed-effect modeling approach was used to compare differences in LV volumes and LVEF among the 3 coronary arterial dominance groups from baseline to 12-month follow-up (group-time interaction). Differences within groups at baseline and at 12-month follow-up were assessed by 1-way analysis of variance. Statistical analysis was performed using SPSS software version 20.0 (SPSS, Inc., Chicago, Illinois). A p value <0.05, by a 2-sided test, was considered statistically significant.
Results
A total of 741 patients with baseline and 12-month follow-up echocardiography were included. A right dominant coronary artery system was noted in 640 patients (86%); 58 patients (8%) had a left dominant coronary artery system and 43 (6%) a balanced coronary artery system. Baseline characteristics and angiographic data of the patient cohort, categorized by coronary arterial dominance, are listed in Table 1 . Mean age was 60 ± 11 years and most patients were men (n = 568, 77%). Overall, baseline characteristics were similar among coronary arterial dominance groups. In addition, in patients with a right dominant coronary artery system the RCA was more often the culprit vessel than in patients with a left dominant or balanced coronary artery system (p <0.01). On the contrary, in patients with a left dominant system, the left anterior descending (LAD) artery and LCx artery were more frequently affected than in patients with a right dominant system (p <0.01 and p = 0.02 for the LAD and LCx arteries, respectively). Only 10% of the total patient population showed 3-vessel disease. Patients with a balanced coronary artery system had a greater prevalence of 3-vessel disease compared with patients with a right or left dominant coronary artery system (21% vs 10% and 5%, respectively, p = 0.02).
| Variable | Total (n=741) | Right dominant (n=640) | Left dominant (n=58) | Balanced (n=43) | P-value |
|---|---|---|---|---|---|
| Men | 568 (77%) | 494 (77%) | 41 (71%) | 33 (77%) | 0.53 |
| Age (years) | 60 ± 11 | 60 ± 11 | 60 ± 10 | 59 ± 10 | 0.88 |
| Diabetes mellitus | 67 (9%) | 55 (9%) | 6 (10%) | 6 (14%) | 0.46 |
| Hypercholesterolemia ∗ | 126 (17%) | 108 (17%) | 10 (17%) | 8 (19%) | 0.96 |
| Hypertension † | 224 (30%) | 186 (29%) | 25 (43%) | 13 (30%) | 0.08 |
| Current smoker | 365 (49%) | 310 (48%) | 31 (53%) | 24 (56%) | 0.52 |
| Glomerular filtration rate (mL/min/1.73m 2 ) | 102 ± 32 | 102 ± 33 | 103 ± 31 | 105 ± 27 | 0.80 |
| Glomerular filtration rate ≤60 mL/min/1.73m 2 | 61 (8%) | 57 (9%) | 2 (3%) | 2 (5%) | 0.24 |
| Peak cardiac troponin T level (μg/L) | 5.8 ± 5.8 | 5.7 ± 5.8 | 5.6 ± 5.5 | 6.4 ± 6.3 | 0.77 |
| Peak cardiac troponin T level ≥3.5 μg/L | 402 (54%) | 346 (54%) | 30 (52%) | 26 (61%) | 0.66 |
| Presenting in Killip class≥2 during STEMI | 26 (4%) | 21 (3%) | 2 (3%) | 3 (4%) | 0.44 |
| Culprit coronary artery | |||||
| Left main | 1 (0.1%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 0.92 |
| Right | 280 (38%) | 268 (42%) | 0 (0%) | 12 (28%) | <0.01 |
| Left anterior descending | 346 (47%) | 282 (44%) | 43 (74%) | 21 (49%) | <0.01 |
| Left circumflex | 114 (15%) | 89 (14%) | 15 (26%) | 10 (23%) | 0.02 |
| No. of coronary arteries narrowed: | |||||
| 1 | 458 (62%) | 393 (61%) | 42 (72%) | 23 (54%) | 0.52 |
| 2 | 210 (28%) | 186 (29%) | 13 (22%) | 11 (26%) | 0.13 |
| 3 | 73 (10%) | 61 (10%) | 3 (5%) | 9 (21%) | 0.02 |
∗ Serum total cholesterol ≥230 mg/dl and/or serum triglycerides ≥200 mg/dl or treatment with lipid lowering drugs.
† Defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or the use of antihypertensive medication.
Table 2 lists the comparison of LV function and volumes at baseline and 12-month follow-up among patients with right dominant, left dominant, and balanced coronary artery system. At baseline, patients with a left dominant coronary artery system showed significantly lower LVEF compared with patients with a right dominant or balanced coronary artery system (LVEF 45 ± 8% vs 48 ± 9% and 50 ± 9% for left dominant, right dominant, and balanced coronary artery system, respectively, p = 0.03). This difference among groups was mainly based on the difference between patients with a left dominant and a balanced coronary artery system (p = 0.025). However, at 12-month follow-up, no differences in LVEF or LV volumes were observed among the different coronary arterial dominance groups ( Table 2 ). Similar improvement in LVEF and WMSI was noted among patients with a right dominant, left dominant, and balanced coronary artery system (group-time interaction p = 0.181 and p = 0.355 for LVEF and WMSI, respectively; Figure 2 ). Although LV end-systolic volume significantly decreased at 12-month follow-up in patients with a right and left dominant coronary artery system ( Table 2 ), the linear mixed model analysis indicated that changes in LV end-systolic volume did not differ among groups (p = 0.073, Figure 2 ). In addition, the within-group analysis showed that patients with a right dominant system had a significant increase in LV end-diastolic volume at 12-month follow-up, whereas, in patients with a left dominant or balanced system no change was noted ( Table 2 ). However, the linear mixed model analysis showed no significant changes in LV end-diastolic volume over time among coronary arterial dominance groups (p = 0.106, Figure 2 ).



