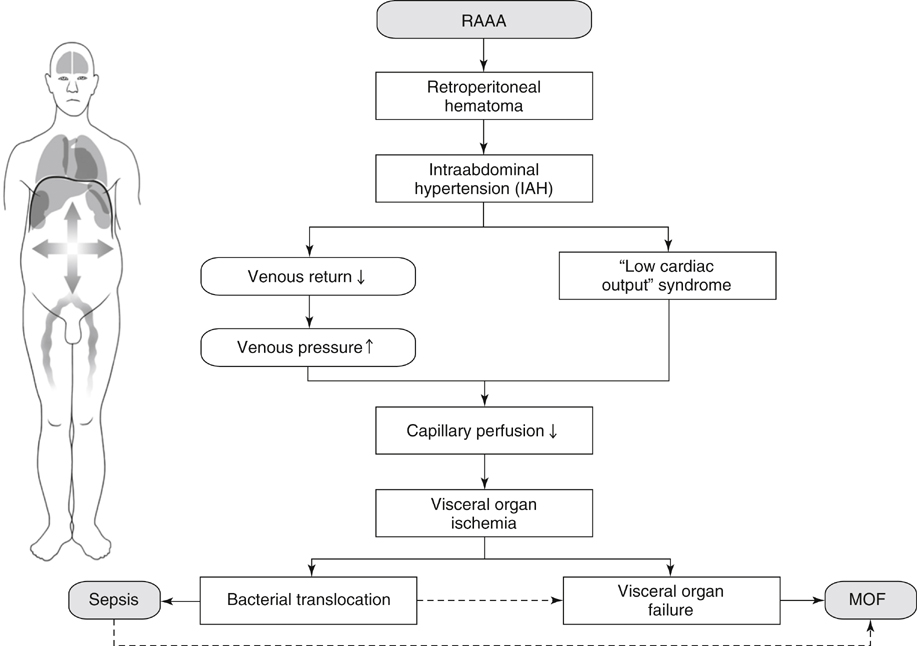
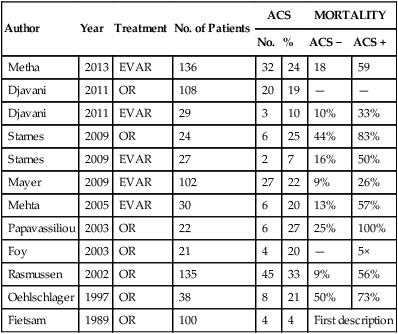
Abdominal compartment syndrome (ACS) and intraabdominal hypertension (IAH) caused by elevated intraabdominal pressure (IAP) are commonly encountered in patients with ruptured abdominal aortic aneurysms (AAAs) and carry a high morbidity and mortality risk (Table 1). However, IAH/ACS are still overlooked by many physicians and therefore timely diagnosis is not made and treatment is often inadequate. TABLE 1 Incidence and Mortality of Abdominal Compartment Syndrome in Patients with Ruptured Abdominal Aortic Aneurysm and Relation to Type of Repair The World Society of the Abdominal Compartment Syndrome (WSACS) has first brought order into the chaos of differing definitions of IAH and ACS by publishing part one of the WSACS Consensus Definitions and Recommendations in 2006. In this document, state-of-the-art definitions for IAH and ACS are proposed based upon current medical evidence as well as expert opinion. In 2013, these consensus definitions and recommendationshave been revised and resulted in updated consensus definitions and clinical practice guidelines (Box 1). The WSACS website (www.wsacs.org) provides several links to educational movies showing various techniques of measuring bladder pressure with different industrially assembled IAP measurement kits (see Education, IAP techniques [requires password]). It is generally regarded as less important which method is used for IAP measurement so long as IAP is routinely measured. IAP values should always be expressed as mm Hg (1 mm Hg = 1.36 cm H2O). Significant physiologic derangements occur as a result of IAH and affect not only the intraabdominal organs but also every organ system in the body (polycompartment syndrome). All of these pathophysiologic derangements are potentially reversible if IAH is recognized and rapidly treated before significant organ dysfunction has developed. If these derangements are prolonged or untreated, subsequent organ failure occurs at variable pressure thresholds (specific for each organ system) owing to inappropriate tissue perfusion (Figure 1). Preexisting comorbidities, such as chronic kidney failure, pulmonary disease, or cardiovascular disease can further reduce the threshold of IAH that causes the clinical manifestations of ACS.
Recognition and Treatment of Abdominal Compartment Syndrome Following Ruptured Abdominal Aortic Aneurysm Repair
Author
Year
Treatment
No. of Patients
ACS
MORTALITY
No.
%
ACS −
ACS +
Metha
2013
EVAR
136
32
24
18
59
Djavani
2011
OR
108
20
19
—
—
Djavani
2011
EVAR
29
3
10
10%
33%
Starnes
2009
OR
24
6
25
44%
83%
Starnes
2009
EVAR
27
2
7
16%
50%
Mayer
2009
EVAR
102
27
22
9%
26%
Mehta
2005
EVAR
30
6
20
13%
57%
Papavassiliou
2003
OR
22
6
27
25%
100%
Foy
2003
OR
21
4
20
—
5×
Rasmussen
2002
OR
135
45
33
9%
56%
Oehlschlager
1997
OR
38
8
21
50%
73%
Fietsam
1989
OR
100
4
4
First description
Detection
Pathophysiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine