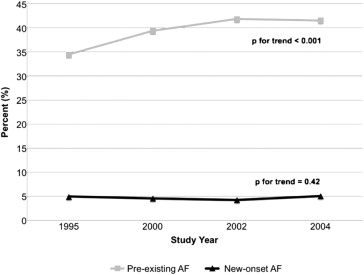
Atrial fibrillation (AF) and heart failure (HF) are common cardiovascular diseases and the co-occurrence of AF and HF has been associated with reduced survival. Data are needed on the potentially changing trends in the characteristics, treatment, and prognosis of patients with acute decompensated HF (ADHF) and AF. The study population consisted of 9,748 patients hospitalized with ADHF at 11 hospitals in the Worcester, Massachusetts, metropolitan area during 4 study years (1995, 2000, 2002, and 2004). Of the 9,748 patients admitted with ADHF, 3,868 (39.7%) had a history of AF and 449 (4.6%) developed new-onset AF during hospitalization. The rates of new-onset AF remained stable (4.9% in 1995; 5.0% in 2004), but the proportion of patients with pre-existing AF (34.5% in 1995; 41.6% in 2004) increased over time. New-onset and pre-existing AF were associated with older age, but pre-existing AF was more closely linked to a greater co-morbid disease burden. The use of HF therapies did not differ greatly by AF status. Despite this, new-onset AF was associated with a longer length of stay (7.5 vs 6.1 days) and greater in-hospital death rates (11.4% vs 6.6%). In contrast, pre-existing AF was associated with lower rates of postdischarge survival compared to patients with no AF (p <0.05 for all). The mortality rates improved significantly over time in patients with AF. In conclusion, AF was common among patients with ADHF, and the proportion of ADHF patients with co-occurring AF increased during the study period. Despite improving trends in survival, patients with ADHF and AF are at increased risk of in-hospital and postdischarge mortality.
Heart failure (HF) and atrial fibrillation (AF) represent 2 global cardiovascular disease epidemics. The prevalence of AF is high and ever increasing, concomitant with the aging of the United States population, likely because this arrhythmia disproportionately affects older subjects and those with HF. The effect of AF on the quality of life and longevity of the affected patients is profound, because AF has been associated with greater hospitalization rates, a lower quality of life, a markedly greater risk of ischemic stroke, and reduced survival. Approximately 1 in 3 patients with HF also have AF, and upward of 40% of patients diagnosed with HF develop AF within 10 years of their diagnosis. However, the epidemiology, treatment, and prognosis of AF and HF have changed in recent years, and several reports have suggested that AF is no longer associated with increased mortality in well-treated patients with HF. There could also be differences in the prognosis of AF developing before, versus after, HF onset. Despite conflicting data on the prognostic import of AF and its changing treatment, limited relatively recent information exists on the incidence, treatment, and in-hospital and long-term outcomes of patients hospitalized with HF, further categorized according to the presence and type of AF.
Methods
The Worcester Heart Failure Study is a community-based investigation of adult residents from the Worcester, Massachusetts, metropolitan area (2000 census population estimates 478,000) who were hospitalized for ADHF at any of the 11 greater Worcester medical centers during 4 study years (1995, 2000, 2002, and 2004). Primary and/or secondary “International Classification of Diseases” discharge diagnoses consistent with possible HF were reviewed in a standardized fashion, as previously outlined in detail. Patients with a discharge diagnosis of HF and patients with a discharge diagnosis of rheumatic HF, hypertensive heart and renal disease, cardiomyopathy, pulmonary heart disease and congestion, acute lung edema, edema, dyspnea, acute cor pulmonale, pulmonary heart disease and congestion, dyspnea, and respiratory abnormalities had their charts reviewed by trained study physicians and nurses to identify hospitalized patients with ADHF. The diagnosis of HF was confirmed using the Framingham criteria and required that patients had met ≥2 major, or 1 major and 2 minor, criteria for HF present. Incident HF was considered to be present if a patient did not have a previous hospitalization for HF noted, a previous physician diagnosis of HF, or treatment of HF determined by hospital record review. Patients with HF secondary to another acute illness, after surgery, or after an interventional procedure were excluded.
Trained study staff abstracted the demographic, clinical, treatment, and laboratory information from the patients’ medical records. Information was collected on the patients’ age, gender, co-morbidities, length of hospital stay, and hospital discharge status. We reviewed the physicians’ progress notes and medication logs for the prescription of cardiac medications, especially those thought to be of benefit in improving the prognosis (e.g., β blockers, angiotensin-converting enzyme inhibitors) or symptoms (e.g., diuretics, digoxin) of patients with ADHF. The short- and long-term survival status was determined through a comprehensive review of all regional hospital records for other medical care contacts and by reviewing the Social Security Death Index and death certificates at the Massachusetts State Health Department.
Patients with pre-existing AF were identified on the basis of documentation of AF at any previous point in their medical history. The presence of AF was determined from the data from the medical record and a review of all electrocardiograms obtained during hospitalization for ADHF. The criteria used to define new-onset AF in the present study were electrocardiographic changes consistent with AF on admission or at any point during their hospitalization among those without a history of AF.
We examined the differences in the characteristics and treatment of patients with pre-existing, new-onset, and no AF using t tests and chi-square tests for continuous and discrete variables, respectively. Logistic regression analysis was used to examine the changes over time in the rates of new-onset and pre-existing AF, adjusting for factors associated with the risk of AF (age, gender, race, length of stay, history of chronic obstructive pulmonary disease, stroke, anemia, diabetes, coronary heart disease, coronary artery bypass grafting, and admission systolic and diastolic blood pressure, heart rate, creatinine, and serum glucose). The in-hospital and postdischarge case-fatality rates were calculated in a standard manner. Multivariate logistic regression analysis was used to examine the association between the type of AF and the in-hospital, 1-year, and 2-year postadmission mortality, while controlling for previously described factors of prognostic importance. We did not attempt to control for the receipt of medications or interventional therapies owing to the substantial risk of confounding by treatment indication and a the lack of information on the timing of therapy administration relative to AF onset. The analyses were conducted using SAS, version 9.2 (SAS Institute, Cary, North Carolina).
Results
The mean age of the study participants was 76.2 years, 56.1% were women, and 93.3% were white. Of the 9,748 patients admitted with ADHF from 1995 to 2004, 3,868 patients (39.7%) had a history of AF and 449 (4.6%) developed new-onset AF during hospitalization ( Table 1 ). Greater rates of new-onset AF were observed in patients without a history of HF (7.0% vs 3.6%).
| Variable | New-Onset AF (n = 449) | p Value (New vs No) | Pre-Existing AF (n = 3,868) | p Value (Pre vs No) | No AF (n = 5,431) | p Value (New vs Pre) |
|---|---|---|---|---|---|---|
| Age (yrs) | 78.5 ± 11.0 | <0.001 | 79.1 ± 9.95 | <0.001 | 73.9 ± 13.1 | 0.23 |
| Men | 206 (45.9%) | 0.20 | 1,757 (45.4%) | <0.05 | 2,321 (42.7%) | 0.85 |
| White race | 433 (96.4%) | <0.001 | 3,709 (95.9%) | <0.001 | 4,949 (91.1%) | 0.57 |
| Body mass index (kg/m 2 ) | 28.2 ± 8.4 | 0.18 | 27.1 ± 9.3 | <0.001 | 28.9 ± 9.1 | <0.05 |
| Systolic blood pressure (mm Hg) | 140.6 ± 31.4 | <0.001 | 138.7 ± 30.3 | <0.001 | 146.1 ± 34.3 | 0.21 |
| Diastolic blood pressure (mm Hg) | 77.2 ± 20.7 | 0.16 | 72.8 ± 18.6 | <0.001 | 75.8 ± 20.4 | <0.001 |
| Pulse (beats/min) | 96.5 ± 27.2 | <0.001 | 88.9 ± 24.1 | 0.53 | 89.2 ± 21.3 | <0.001 |
| Length of stay (days) | 7.54 ± 7.92 | <0.05 | 6.14 ± 8.69 | 0.56 | 6.07 ± 7.01 | <0.05 |
| Chronic obstructive pulmonary disease | 150 (33.4%) | 0.46 | 1,441 (37.3%) | <0.05 | 1,909 (35.2%) | 0.11 |
| Anemia | 86 (19.2%) | 0.07 | 1,077 (27.8%) | <0.001 | 1,236 (22.8%) | <0.001 |
| Coronary heart disease | 200 (44.5%) | <0.001 | 2,329 (60.2%) | <0.001 | 2,927 (53.7%) | <0.001 |
| Heart failure | 252 (56.1%) | <0.001 | 3,105 (80.3%) | <0.001 | 3,557 (65.5%) | <0.001 |
| Angina | 63 (14.0%) | <0.05 | 642 (16.6%) | 0.21 | 956 (17.6%) | 0.16 |
| Coronary artery bypass grafting | 70 (15.6%) | 0.06 | 956 (24.7%) | <0.001 | 1,038 (19.1%) | <0.001 |
| Diabetes mellitus | 135 (30.1%) | <0.001 | 1,371 (35.4%) | <0.001 | 2,301 (42.4%) | <0.05 |
| Hypertension | 304 (67.7%) | 0.72 | 2,667 (69.0%) | 0.67 | 3,722 (68.5%) | 0.59 |
| Stroke | 47 (10.5%) | 0.17 | 564 (14.6%) | <0.05 | 687 (12.7%) | <0.05 |
| Renal disease | 93 (20.7%) | <0.05 | 1,036 (26.8%) | 0.29 | 1,401 (25.8%) | <0.01 |
| Peripheral vascular disease | 73 (16.3%) | 0.08 | 780 (20.2%) | 0.49 | 1,064 (19.6%) | <0.05 |
| Creatinine (mg/dl) | 1.6 ± 1.4 | 0.11 | 1.6 ± 1.0 | <0.001 | 1.71 ± 1.9 | 0.93 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 54.1 ± 59.2 | 0.89 | 51.0 ± 24.9 | <0.001 | 53.7 ± 31.7 | 0.27 |
| Total cholesterol (mg/dl) | 150.4 ± 46.1 | <0.01 | 156.3 ± 50.7 | <0.001 | 168.1 ± 51.1 | 0.31 |
| Glucose (mg/dl) | 154.6 ± 69.8 | <0.01 | 153.2 ± 71.6 | <0.001 | 166.3 ± 82.3 | 0.70 |
| B-type natriuretic peptide (ng/L) | 906.3 ± 906.6 | 0.07 | 959.6 ± 1,079.1 | <0.05 | 1,120.8 ± 1,272.8 | 0.69 |
| Baseline ejection fraction (%) ∗ | 45.7 ± 16.5 | 0.84 | 45.5 ± 25.2 | 0.90 | 45.5 ± 20.0 | 0.91 |
| Left bundle branch block | 41 (9.1%) | 0.58 | 410 (10.6%) | 0.31 | 538 (9.9%) | 0.34 |
∗ Echocardiographic data were available for only 5,009 participants.
The rates of new-onset AF remained stable from 1995 to 2004 (4.9% to 5.0%), and the proportion of patients with pre-existing AF (34.5% to 41.6%) increased during the study years ( Figure 1 ). In the multivariate logistic regression analyses adjusting for potential confounders, the odds of developing new-onset AF during hospitalization for ADHF was 30% greater in 2004 than in 1995 (odds ratio 1.30, 95% confidence interval 0.96 to 1.77) and the odds of presenting with a history of AF was nearly 50% greater in 2004 than in 1995 (odds ratio 1.42, 95% confidence interval 1.24 to 1.63).
Patients admitted for ADHF with a history of AF or new-onset AF were, on average, older and more likely to be white than were patients with no AF ( Table 1 ). Patients with new-onset AF had a lower systolic blood pressure and heart rate but diastolic blood pressure values similar to those of patients with no AF on admission. Patients with pre-existing AF, but not new-onset AF, were more likely to report a history of cardiovascular and noncardiovascular disease.
The demographic characteristics of patients with new-onset AF differed little from those of the patients with pre-existing AF. However, those with new-onset AF had a lower burden of co-morbid disease and a poorer hemodynamic profile on hospital presentation ( Table 1 ). Likely reflecting the lower prevalence of diabetes and obesity among patients with pre-existing and new-onset AF, both groups had lower admission blood glucose and total cholesterol levels than did the patients with no previous AF.
The treatment of patients with ADHF and either new-onset or pre-existing AF was significantly different from those with no AF ( Table 2 ). Patients with new-onset and pre-existing AF were less likely to have been prescribed aspirin, nitrates, or statins but were more likely to have received digoxin, amiodarone, or anticoagulants (>½ were prescribed warfarin) during hospitalization for ADHF. Patients with any type of AF were less likely to have undergone percutaneous coronary revascularization but were more likely to have received a permanent pacemaker than those with no AF. The use of evidence-based HF medications differed little between the patients with ADHF with pre-existing and new-onset AF ( Table 2 ). The patients developing AF in-hospital were more commonly prescribed heparin but were less commonly prescribed warfarin or amiodarone than those with pre-existing AF. Patients with pre-existing AF were less likely to have undergone percutaneous coronary intervention than those with new-onset AF.
| Treatment | New-Onset AF (n = 449) | p Value (New vs No) | Pre-Existing AF (n = 3,868) | p Value (Pre vs No) | No AF (n = 5,431) | p Value (New vs Pre) |
|---|---|---|---|---|---|---|
| In-hospital medications | ||||||
| Aspirin | 239 (53.2%) | <0.001 | 1,922 (49.7%) | <0.001 | 3,325 (61.2%) | 0.16 |
| β Blocker | 249 (55.5%) | 0.78 | 2,163 (55.9%) | 0.27 | 2,974 (54.8%) | 0.85 |
| Angiotensin-converting enzyme inhibitor | 220 (49.0%) | 0.18 | 1,960 (50.7%) | 0.12 | 2,841 (52.3%) | 0.50 |
| Angiotensin receptor blocker | 22 (4.9%) | 0.52 | 264 (6.8%) | <0.05 | 305 (5.6%) | 0.12 |
| Statin | 100 (22.3%) | <0.01 | 1,022 (26.4%) | <0.05 | 1,541 (28.4%) | 0.05 |
| Digoxin | 257 (57.2%) | <0.001 | 2,382 (61.6%) | <0.001 | 1,603 (29.5%) | 0.08 |
| Nitrate | 244 (54.3%) | 0.09 | 2,136 (55.2%) | <0.01 | 3,177 (58.5%) | 0.72 |
| Diuretic | 439 (97.8%) | 0.34 | 3,757 (97.1%) | 0.75 | 5,269 (97.0%) | .042 |
| Amiodarone | 31 (6.9%) | <0.05 | 471 (12.2%) | <0.001 | 193 (3.6%) | <0.01 |
| Anticoagulants | 314 (69.9%) | <0.001 | 2,891 (74.7%) | <0.001 | 3,002 (55.3%) | <0.05 |
| Warfarin | 183 (40.8%) | <0.001 | 2,040 (52.7%) | <0.001 | 616 (11.3%) | <0.001 |
| Heparin | 206 (45.9%) | 0.59 | 1,316 (34.0%) | <0.001 | 2,420 (44.6%) | <0.001 |
| Enoxaparin | 49 (10.9%) | <0.001 | 317 (8.2%) | <0.01 | 352 (6.5%) | 0.06 |
| Procedures | ||||||
| Percutaneous coronary intervention | 25 (5.6%) | 0.23 | 134 (3.5%) | <0.001 | 381 (7.0%) | <0.05 |
| Coronary artery bypass grafting | 2 (0.5%) | 0.32 | 15 (0.4%) | <0.01 | 46 (0.9%) | 0.86 |
| Intra-aortic balloon pump | 1 (0.2%) | 0.94 | 6 (0.2%) | 0.37 | 13 (0.2%) | 0.75 |
| Permanent pacemaker | 11 (2.5%) | <0.05 | 92 (2.4%) | <0.001 | 63 (1.2%) | 0.93 |
The patients admitted with ADHF and either pre-existing or new-onset AF had greater in-hospital and postdischarge mortality rates than did those with no AF ( Figure 2 ). After adjustment for differences in the factors known to influence the prognosis of patients with ADHF, the patients with new-onset AF remained nearly 70% more likely to die during their index hospitalization. In contrast, patients with pre-existing AF were at 30% greater odds of dying at 1 and 2 years after hospital discharge compared to the patients without AF ( Table 3 ).





