Little is known about the outcomes and indications of chronic total occlusion percutaneous coronary intervention (CTO-PCI), other than in high-volume centers. We sought to provide a real-world overview of the clinical outcomes and appropriateness of PCI for CTO. The analysis included 4,950 consecutive PCIs for nonacute indications registered in the multicenter Japanese PCI registry in collaboration with the US National Cardiovascular Data Registry (Cath-PCI). Data included demographics, clinical outcomes (procedural success and complication rates), and the indication appropriateness, based on the 2012 appropriate use criteria for revascularization. The overall procedural success and major adverse cardiac event rates of 501 cases with CTO-PCI (10.1%) were 76% and 3.2%, respectively. Based on the criteria, mapping failures occurred in 2,521 procedures; the remaining 2,429 PCIs were successfully mapped. The CTO-PCIs were performed for more appropriate indications than PCIs for lesions without CTO. The rate of inappropriate indications was significantly lower in CTO-PCIs than in non–CTO-PCIs (23.0% vs 31.4%, p = 0.04). Only 17% of CTO-PCIs were directly assigned to CTO-specific scenarios because such scenarios are only intended for “Lone” CTO; the rest of the CTO-PCI cases were secondarily mapped to non-CTO–specific scenarios. In conclusion, as many as 10% of the elective PCIs were performed for CTO lesions in a contemporary multicenter Japanese PCI registry; CTO-PCI was associated with lower procedural success and higher complication rates than non–CTO-PCI. Its indication was relatively appropriate; however, our findings emphasize the need for more rigorous evaluation in terms of the present insufficient CTO-related clinical scenarios.
The prevalence of chronic total occlusion (CTO), a coronary lesion that is completely occluded for >3 months, is reportedly 18% to 52% in large registries. Despite the development of novel equipment and techniques, percutaneous coronary intervention (PCI) for lesions with CTO is technically challenging and often referred to as “the last frontier” for interventional cardiologists; favorable success rates of CTO-PCIs ranging from 82.9% to 87.9% have been previously reported on the basis of data from high-volume centers or operators. However, real-world data and outcomes of contemporary CTO-PCIs in institutes other than high-volume centers have been limited ; despite the benefits associated with successful CTO-PCIs, it has been performed relatively infrequently in average-sized centers, mostly because of historically low success rates and fear of procedure-related complications. Therefore, an understanding of the patients’ backgrounds and complication rates is needed for the real-world implementation of CTO-PCIs. Furthermore, the appropriateness of CTO-PCI has not been investigated using internationally derived criteria. Appropriate use criteria (AUC) for revascularization was recently developed by the American College of Cardiology Foundation and 5 other societies in response to increasing momentum toward compliance with appropriate procedural indications. These AUC have been applied to various registries, the results of which indicate a strong possibility of PCI overuse in real-world practice. The indications for PCI should be rigorously considered, particularly when used for CTO, given the relatively high incidence of complications (1.8% to 3.1%) and risk of exposure to contrast media or radiation. The purpose of the present study was to clarify the outcomes of CTO-PCIs in real-world practice in Japan and to evaluate the appropriateness of PCI indications based on the US AUC in an effort to identify the gap between demographic and outcome information between CTO-PCIs performed in high-volume and average-sized centers and to determine whether registered CTO-PCI procedures are considered appropriate under validated standards and, conversely, whether the provided scenarios in these standards adequately cover “real-world” PCI cases.
Methods
Data were obtained from the Japan Cardiovascular Database Keio Inter-hospital Cardiovascular Studies (JCD-KICS) PCI registry, which is a prospective, multicenter registry designed to collect clinical variables and outcome data on consecutive patients with PCI, with dedicated clinical research coordinators assigned to each site. In this registry, 16 teaching hospitals within the metropolitan Tokyo area participated in and registered all PCI procedures performed during the study period, including failure cases, using an Internet-based interface. The annual average number of PCIs for each institution was 153. Approximately, 200 variables were collected for each patient; clinical variables and inhospital outcomes in the JCD-KICS were defined in accordance with the National Cardiovascular Data Registry (NCDR) version 4.1.
The data were checked for completeness and internal consistency. Quality assurance was achieved through automatic system validation and reporting of data completeness and through education and training for dedicated clinical research coordinators specifically trained for the present PCI registry. The senior study coordinator (IU) and exclusive onsite auditing by the investigators (SK and AK) ensured proper registration of each patient.
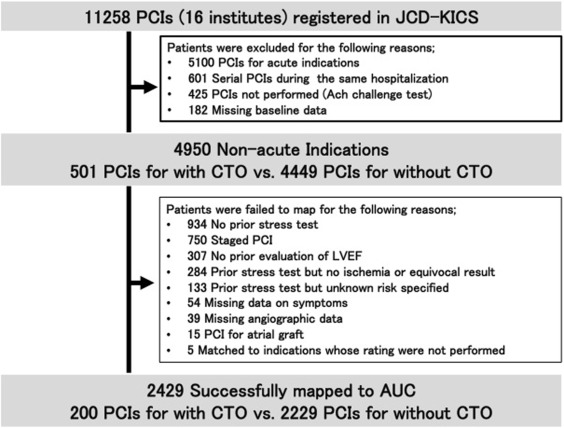
A total of 11,258 consecutive patients who underwent PCI procedures from September 2008 to March 2013 for acute and nonacute indications were registered in the database. Of these, 6,308 patients were excluded because they underwent PCIs for acute indications (n = 5,100), underwent serial PCIs during the same hospitalization (n = 601), underwent an acetylcholine challenge test (n = 425), or had insufficient baseline data (n = 182). CTO was defined as angiographic evidence of a total occlusion of Thrombolysis In Myocardial Infarction (TIMI) grade 0 flow for an estimated duration of at least 3 months based on the first onset of angina pectoris, a history of myocardial infarction in the target vessel territory, or comparison with a previous angiogram. In this study, cases with unknown occlusion duration were also identified as CTO. On the basis of this definition, CTO should not be the culprit lesion of ACS; therefore, we excluded the acute cases from this analysis. The remaining 4,950 patients underwent PCI for nonacute indications were included in the analysis ( Figure 1 ).
Procedural success was defined as successful CTO recanalization with achievement of <50% residual stenosis within the treated segment and restoration of Thrombolysis In Myocardial Infarction grade 3 anterior flow. Inhospital major adverse cardiac events (MACE) included any of the following adverse events before hospital discharge: myocardial infarction, recurrent angina requiring urgent repeat target vessel revascularization with PCI or coronary artery bypass surgery, tamponade requiring pericardiocentesis or surgery, or death from any cause. Bleeding was defined as follows: (1) occurring at the percutaneous entry site, during or after the catheterization laboratory visit until discharge, which may be external or a hematoma >10 cm for femoral, >5 cm for brachial, or >2 cm for radial access; (2) retroperitoneal; (3) gastrointestinal; (4) genitourinary; or (5) other/unknown origin during or after the catheterization laboratory visit until discharge. Only bleeding events requiring a transfusion and/or with a decrease in hemoglobin >3.0 g/dl were included. This bleeding criterion is also consistent with Bleeding Academic Research Consortium grade 3A to C. The definition of these complications was in accordance with the NCDR Cath-PCI registry, and any additional data elements and definitions can be found at their Web site.
The method to develop the AUC for coronary revascularization has been previously described. The AUC was originally developed through a collaboration of 6 American professional organizations (American College of Cardiology Foundation, Society for Cardiovascular Angiography and Intervention, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and American Society of Nuclear Radiology) in 2009 and updated in 2012. We used an algorithm to map PCIs in the JCD-KICS PCI registry to the updated 2012 AUC to rate the procedures as appropriate, uncertain, or inappropriate. This algorithm, which was validated in a previous study, enabled the mapping to be performed in an efficient manner. All the definitions in our study were identical to those in the AUC.
Baseline characteristics and clinical outcomes, including the technical success rate and inhospital MACE, as well as the appropriateness ratings were compared between the PCIs for lesions with and without CTO using the chi-square test or Fisher’s exact test for categorical variables and the Student unpaired t test or Wilcoxon rank-sum test for continuous variables. Data were analyzed using SPSS version 22 (IBM Corp, Armonk, New York). All p values were 2 sided, and significance was defined as p <0.05 for all analyses.
Results
In the 4,950 elective PCIs, CTO-PCI was performed for 501 cases (10.1%). Table 1 lists the demographics of the patients. The patients with CTO lesions were likely to be younger, male, and to have a lower prevalence of a previous history of PCI compared with patients without CTO. There were also differences in the preprocedural evaluation pattern between the patients with and without CTO lesions; in patients with CTO lesions, computed tomography angiography (CTA) was more frequently performed, whereas the use of myocardial perfusion imaging (MPI) was similar between the 2 groups. Furthermore, implementation of medical therapy at discharge was also different between the patients with and without CTO lesions; in patients with CTO lesions, optimal medical therapy, including the use of β blockers and statins, was more frequently implemented compared with patients without CTO. Notably, the prescription rate of clopidogrel was significantly lower and tended to be replaced with other antiplatelet/anticoagulant agents such as cilostazole or warfarin in patients with CTO.
| Variables | Chronic Total Occlusion | P value | |
|---|---|---|---|
| Yes (N=501) | No (N=4449) | ||
| Mean age (years) | 66.6±10.8 | 68.4±9.6 | <0.001 |
| Body mass index (kg/m 2 ) | 24.7±3.7 | 24.4±3.5 | 0.103 |
| Men | 429 (85.6%) | 3577 (80.4%) | 0.005 |
| Smoker | 157 (31.3%) | 1338 (30.1%) | 0.573 |
| Hypertension | 382 (76.2%) | 3492 (78.5%) | 0.253 |
| Dyslipidemia | 366 (73.1%) | 3206 (72.1%) | 0.674 |
| Diabetes mellitus | 219 (43.7%) | 2109 (47.4%) | 0.119 |
| Previous heart failure | 62 (12.4%) | 495 (11.1%) | 0.412 |
| Previous myocardial infarction | 188 (37.5%) | 1514 (34.0%) | 0.124 |
| Previous percutaneous coronary intervention | 230 (45.9%) | 2393 (53.8%) | 0.001 |
| Previous coronary bypass | 41 (8.2%) | 296 (6.7%) | 0.191 |
| Hemodialysis | 20 (4.0%) | 229 (5.1%) | 0.331 |
| Previous cerebrovascular disease | 55 (11.0%) | 400 (9.0%) | 0.143 |
| Previous peripheral artery disease | 62 (12.4%) | 463 (10.4%) | 0.193 |
| Previous chronic obstructive pulmonary disease | 15 (3.0%) | 141 (3.2%) | 1 |
| Canadian cardiovascular society class | |||
| Asymptomatic | 247 (49.3%) | 1912 (43.0%) | 0.109 |
| Ⅰ | 58 (11.6%) | 635 (14.3%) | |
| Ⅱ | 120 (24.0%) | 1251 (28.1%) | |
| Ⅲ | 48 (8.9%) | 420 (9.4%) | |
| Ⅳ | 8 (1.6%) | 72 (1.6%) | |
| Unknown | 16 (3.2%) | 112 (2.5%) | |
| Laboratory findings | |||
| Creatinine (mg/dl) | 0.9 (0.5-1.3) | 0.9 (0.6-1.2) | 0.813 |
| Hemogrobin (g/dl) | 13.2±1.9 | 13.2±2.1 | 0.985 |
| Preprocedural computed tomography angiography | 209 (41.7%) | 1366 (30.7%) | <0.001 |
| Preprocedural myocardial perfusion imaging | 138 (27.5%) | 1267 (28.5%) | 0.087 |
| Mild | 15 (3.0%) | 239 (5.4%) | 0.081 |
| Moderate | 66 (13.2%) | 553 (12.4%) | |
| Severe | 26 (5.2%) | 162 (3.6%) | |
| Unknown | 31 (6.2%) | 287 (6.5%) | |
| Chronic total occlusion site | |||
| Left anterior descending | 176 (35.1%) | Not applicable | |
| Left circumflex | 109 (21.8%) | ||
| Right coronary artery | 216 (43.1%) | ||
| Prescription at discharge | |||
| Aspirin | 491 (98.0%) | 4372 (98.3%) | 0.126 |
| Clopidogrel | 420 (83.8%) | 4002 (90.0%) | <0.001 |
| Ticlopidine | 27 (5.4%) | 223 (5.0%) | 0.66 |
| Cilostazole | 22 (4.4%) | 110 2.5%) | 0.044 |
| Warfarin | 57 (11.4%) | 396 (8.9%) | 0.227 |
| Angiotensin-converting enzyme inhibitor | 317 (63.3%) | 2763 (62.1%) | 0.76 |
| Angiotensin receptor blocker | |||
| Beta-blocker | 362 (72.3%) | 2864 (64.4%) | 0.004 |
| Calcium blocker | 164 (32.7%) | 1729 (38.9%) | 0.026 |
| Statin | 435 (86.8%) | 3637 (81.7%) | 0.027 |
Table 2 provides the clinical outcomes, including the rates of procedural success and complications. Overall success rate of CTO-PCI was 76.0%. The incidence of MACE was not significantly different between the 2 groups (3.2% for CTO-PCIs vs 2.5% for PCIs for lesion without CTO, p = 0.371), but tamponade, coronary perforation, cardiogenic shock after procedure, and bleeding were more frequently observed in CTO-PCIs. In addition, a greater amount of contrast media was used for CTO-PCIs.
| Chronic total occlusion | P value | ||
|---|---|---|---|
| Yes (N=501) | No (N=4449) | ||
| Procedural Success | 381 (76.0%) | 4295 (96.5%) | <0.001 |
| Major adverse cardiac events | 16 (3.2%) | 112 (2.5%) | 0.371 |
| Tamponade | 4 (0.8%) | 3 (0.1%) | 0.003 |
| Urgent Revascularization | 1 (0.2%) | 5 (0.1%) | 0.473 |
| Post-procedural myocardial infarction | 11 (2.2%) | 101 (2.3%) | 1 |
| In-hospital Death | 3 (0.6%) | 9 (0.2%) | 0.114 |
| Coronary Dissection | 10 (2.0%) | 51 (1.1%) | 0.129 |
| Coronary Perforation | 20 (4.0%) | 39 (0.9%) | <0.001 |
| Cardiogenic Shock | 8 (1.6%) | 28 (0.6%) | 0.025 |
| Heart Failure | 3 (0.6%) | 16 (0.4%) | 0.432 |
| Stroke | 2 (0.4%) | 8 (0.2%) | 0.269 |
| Contrast Volume | 230 (72 – 388) | 160 (81 – 239) | <0.001 |
| Hemodialysis | 2 (0.4%) | 7 (0.2%) | 0.229 |
| Bleeding Complication | 25 (5.0%) | 76 (1.7%) | <0.001 |
| Transfusion | 14 (2.8%) | 46 (1.0%) | 0.002 |
| Fluoroscopy time (minute) | 59.6±36.1 | 28.7±19.8 | <0.001 |
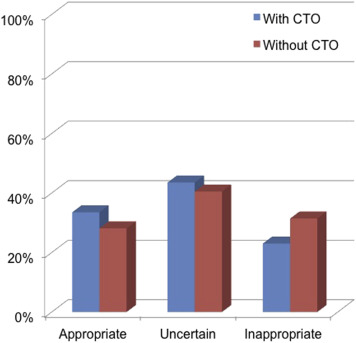
In the 4,950 elective PCIs, a rating could not be determined for 2,521 PCIs ( Figure 1 ) mainly because of one of the following reasons: no previous stress test performed (n = 934), staged PCI (n = 750), no previous evaluation of left ventricular systolic function (n = 307), or previous stress test with no ischemia or equivocal result (n = 284). Of the 2,429 PCIs that were rated, CTO-PCIs were performed for fewer inappropriate indications than PCIs for lesions without CTO (23.0% vs 31.4%, p = 0.04; Figure 2 ). However, because cases with multiple stenotic lesions were excluded from ratings in all CTO-specific scenarios ( Table 3 ), the vast majority of CTO-PCIs could not be related directly to CTO-specific scenarios. Therefore, in the present study, only PCIs for “Lone” CTO, which accounted for 17% of all CTO-PCIs, were successfully assigned directly to CTO-specific scenarios, and the remaining CTO-PCIs were mapped secondarily to non-CTO–specific scenarios ( Table 4 ).