Many studies have reported comparable risk of hard end points between percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) for unprotected left main coronary artery (ULMCA) stenosis. However, there are limited data regarding the morbidity associated with ULMCA revascularization. This study sought to compare the cause and risk of readmissions after PCI and CABG for ULMCA stenosis. We evaluated the unadjusted and adjusted risk of readmissions in 1,352 patients (783 PCI treated and 569 CABG treated) who were consecutively enrolled in a multicenter registry of patients with ULMCA stenosis, named the Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease trial. Overall, 206 PCI-treated patients (26.3%) experienced at least 1 readmission after the index procedure during 48.7 ± 16.0 months of follow-up compared with 84 CABG-treated patients (14.8%, p <0.001). The most frequent causes of readmission were repeat revascularization after PCI (41%) and noncardiac readmissions after CABG (48%). Through repeated events analysis, PCI was associated with more frequent readmissions than CABG (hazard ratio 2.037, 95% confidence interval 1.542 to 2.692, p <0.001), being an independent predictor of readmission (hazard ratio 1.820, 95% confidence interval 1.420 to 2.331, p <0.001). Except for the acute period, defined as the first 3 months, when there was no significant difference in readmission rate, a higher readmission rate after PCI was consistently observed over the remainder of the follow-up period. In conclusion, PCI was shown to be associated with a higher risk of readmission than CABG in treating ULMCA disease. This higher risk was attributable to more frequent revascularization in the PCI group.
A substudy from a large randomized trial and many registry reports have shown that percutaneous coronary intervention (PCI) may be an acceptable substitute for coronary artery bypass grafting (CABG) in some patients with unprotected left main coronary artery (ULMCA) stenosis. However, these studies were conducted with regard to the risks of “hard” end points such as cardiovascular death, myocardial infarction, or their composite. The causes and incidence of all morbidity requiring readmission after CABG or PCI have not been evaluated thoroughly, and information on potential differences in the risk of morbidity may help patients who are facing a treatment choice to decide on a revascularization strategy. The Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease (PRECOMBAT) trial randomized patients suitable for revascularization by either PCI or CABG for the treatment of ULMCA stenosis. To investigate the morbidity of patients with ULMCA stenosis treated with PCI and CABG, we compared readmissions of the patients of the PRECOMBAT trial, in both the randomized group and the prespecified registry.
Methods
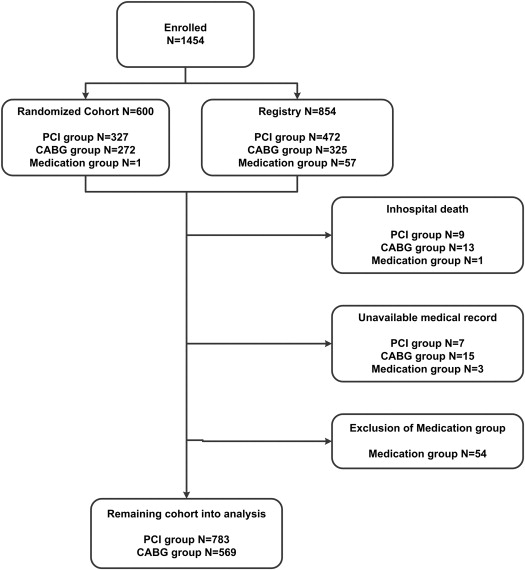
The study design and methods of the PRECOMBAT trial have been described previously in detail. In brief, the PRECOMBAT study (n = 600) was a randomized trial with a parallel registry (n = 854) including nonrandomized patients during the same study period. To analyze the outcomes of all patients with ULMCA stenosis with minimal exclusion, this study included both the randomized group and the patients from the nonrandomized registry of the PRECOMBAT study. Within this population, 799 and 597 patients received PCI and CABG, respectively. The remaining 58 patients, who were treated with medication alone, were not included in this study. Therefore, after excluding 23 cases of in-hospital death (PCI: 9 patients and CABG: 13 patients), 1,352 patients (783 PCI treated and 569 CABG treated) whose medical records were available at the time of event adjudication were included in the comparison of readmission rates ( Figure 1 ). The institutional review board approved the protocol, and all patients provided written informed consent.
The procedures for PCI and CABG have been described previously. During PCI, sirolimus-eluting stents were the default drug-eluting stents used. Use of intravascular ultrasound, adjunctive devices, or glycoprotein IIb/IIIa inhibitors was at the operator’s discretion. All patients who underwent PCI took aspirin plus clopidogrel (loading dose 300 mg) or ticlopidine (loading dose 500 mg) before or during the procedure. After PCI, all patients were prescribed 100 mg/day aspirin indefinitely and 75 mg/day clopidogrel or 250 mg/day ticlopidine for at least 1 year. During CABG, the internal thoracic artery was preferred for bypass of the left anterior descending artery. Medications after CABG were given according to the policy of the institution or the preference of the surgeon. During the index procedure or repeated revascularization, the decision of which lesion to be revascularized was at the operator’s discretion.
After PCI, all patients were asked to revisit for follow-up angiography 8 to 10 months after the procedure, or earlier if experiencing symptoms of angina. However, routine follow-up angiography was not performed for patients who underwent CABG. As a result, the patients treated with PCI (510 patients [65.1%]) underwent follow-up angiography more frequently than those with CABG (98 patients [17.2%], p <0.001). All other follow-up assessments were performed at 1, 6, 9, and 12 months and yearly thereafter at a clinic visit or through a telephone interview.
The primary end point of this study was readmission for any reason after discharge. Readmission related to routine angiographic surveillance of patients without ischemic symptom after PCI was not considered an event. All readmissions to hospitals participating in this trial were recorded during the follow-up period. The date of readmission and the primary reason for it were collected, with the cause of readmission judged by the Clinical Events Committee, which was made up of interventional and noninterventional cardiologists who were not participating in the study. The causes were grouped based on mechanism into 7 categories, including revascularization, nonrevascularization cardiac cause, procedure related, bleeding, cerebrovascular accident, noncardiac event, and unknown cause.
A descriptive analysis was performed by presenting data as mean ± SD or number (proportion). Continuous variables were compared with the t test or Wilcoxon rank sum test, and categorical variables were compared with chi-square statistics or Fisher’s exact test, as appropriate. When calculating the readmission rate, to adjust for the significantly different follow-up period between the 2 groups, an arbitrary unit, readmissions per patient–3 months, was derived. This was obtained by modifying the formula for person-years:
where D is the number of years each subject has been observed. To compare the interval readmission rate, follow-up dates were censored at the fixed time of 5 years because of the small number of patients with longer follow-up. In analyzing readmissions, a marginal approach proposed by Wei, Lin, and Weissfeld was used to analyze recurrent events (the Wei-Lin-Weissfeld method), because conventional time-to-first-event analysis excludes subsequent events after the first event. The subgroup analysis according to the Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) trial score was performed for 1,266 patients (93.6%), using the Wei-Lin-Weissfeld method, for whom independent angiographic analysis was available. To compare rates of revascularization-related readmission between the 2 groups, Cox proportional regression model was used. All statistical analyses were performed using SAS, version 9.3 (SAS Institute, Cary, North Carolina). A 2-tailed p value of <0.05 was considered statistically significant.
Results
Table 1 lists the baseline characteristics of the patients in each group. Patients treated with CABG were older, were more likely to have diabetes requiring insulin, had a history of myocardial infarction, and a higher EuroSCORE than those treated with PCI. Conversely, hyperlipidemia, a history of undergoing PCI, chronic renal failure, and peripheral vascular disease were more prevalent in the PCI group than in the CABG group. Hospital stay was longer in the CABG group than PCI group (2.9 ± 4.2 vs 9.5 ± 20.7, p <0.001). Median follow-up periods after discharge from the index procedure hospitalization were 49 months (interquartile range 37 to 60) and 58 months (interquartile range 39 to 61) for the PCI and CABG groups, respectively. During the follow-up period, 413 readmissions occurred, 299 in the PCI group and 114 in the CABG group.
| Variable | PCI (n = 783) | CABG (n = 569) | p Value |
|---|---|---|---|
| Age (yrs) | 62.2 ± 10.6 | 63.6 ± 9.1 | 0.014 |
| Men | 589 (75.2) | 438 (77.0) | 0.46 |
| Body mass index (kg/m 2 ) | 24.5 ± 2.8 | 24.7 ± 3.0 | 0.33 |
| Medically treated diabetes | |||
| Any | 269 (34.4) | 215 (37.8) | 0.19 |
| Requiring insulin | 23 (2.9) | 41 (7.2) | <0.001 |
| Hypertension ∗ | 437 (55.8) | 315 (55.4) | 0.87 |
| Hyperlipidemia † | 318 (40.6) | 195 (34.3) | 0.018 |
| Current smoker | 212 (27.1) | 164 (28.8) | 0.48 |
| Previous PCI | 149 (19.0) | 73 (12.8) | 0.002 |
| Previous myocardial infarction | 40 (5.1) | 51 (9.0) | 0.005 |
| Previous heart failure | 11 (1.4) | 4 (0.7) | 0.22 |
| Chronic renal failure | 12 (1.5) | 2 (0.4) | 0.034 |
| Peripheral vascular disease | 51 (6.5) | 19 (3.3) | 0.009 |
| Chronic obstructive pulmonary disease | 19 (2.4) | 23 (4.0) | 0.091 |
| Clinical presentation | <0.001 | ||
| Stable angina pectoris or no symptoms | 422 (53.9) | 230 (40.4) | |
| Unstable angina pectoris | 304 (38.8) | 311 (54.7) | |
| Unstable angina pectoris and recent acute myocardial infarction | 57 (7.3) | 28 (4.9) | |
| Ejection fraction (%) | 60.7 ± 9.0 | 57.9 ± 10.7 | <0.001 |
| EuroSCORE value | 2.9 ± 2.0 | 3.2 ± 2.0 | 0.001 |
| Electrocardiographic findings | 0.081 | ||
| Sinus rhythm | 755 (96.4) | 560 (98.4) | |
| Atrial fibrillation | 20 (2.6) | 7 (1.2) | |
| Others | 8 (1.0) | 2 (0.4) | |
| Angiographic characteristics | |||
| Narrowed coronary arteries | <0.001 | ||
| Left main only | 110 (14.0) | 24 (4.2) | |
| Left main plus 1-vessel disease | 185 (23.6) | 55 (9.7) | |
| Left main plus 2-vessel disease | 275 (35.1) | 120 (21.1) | |
| Left main plus 3-vessel disease | 213 (27.2) | 370 (65.0) | |
| Involved location | 0.78 | ||
| Ostial and shaft involvement | 263 (33.6) | 187 (32.9) | |
| Distal bifurcation involvement | 520 (66.4) | 382 (67.1) | |
| Right coronary artery disease | 302 (38.6) | 422 (74.2) | <0.001 |
| Restenotic lesion | 6 (0.8) | 3 (0.5) | 0.74 |
| Chronic total occlusion | 5 (0.6) | 5 (0.9) | 0.75 |
| SYNTAX score ‡ | 23.0 ± 9.9 | 32.4 ± 12.5 | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


