and John B. Hijjawi2
(1)
Department of Surgery, Hofstra North Shore – LIJ School of Medicine, Hempstead, NY, USA
(2)
Departments of Plastic Surgery and General Surgery, Medical College of Wisconsin, Milwaukee, WI, USA
10.1 Epidemiology
10.2 Etiology
10.3 Anatomy/Physiology
10.4 Clinical Assessment
10.5 Diagnostic Testing
10.5.1 Doppler Ultrasonography
10.6 Operative Management
10.6.1 Radial Artery Injury
10.6.2 Ulnar Artery Injury
10.6.3 Digital Artery Injury
10.8 Fasciotomies
10.8.1 Diagnostic Testing
10.9 Complications
10.10 Outcomes
10.11 Conclusion
Abstract
Trauma to the forearm and hand comprises nearly one-third of all upper extremity vascular injuries, often leading to complex injuries leading to significant loss of function due to concomitant nerve and muscle injury. Penetrating trauma is the most common cause of upper extremity vascular injury, and mastery of the anatomy of the distal upper extremity is essential to appropriate surgical management. Stabilization of any accompanying fractures precedes vascular repair; temporary shunting can be utilized in cases of profound ischemia. Primary repair can often be accomplished, but conduit using autogenous vein can be used when direct apposition of the vessel is not appropriate. Trauma to the radial artery can sometimes be addressed with simple ligation. However, this is not an option in patients who do not have a normally dominant ulnar artery. Duplication of the digital arteries typically permits loss of one of the two vessels to the fingers. Endovascular techniques have been described for the management of distal upper extremity trauma, but are not yet mainstream options. A multidisciplinary approach to the management of upper extremity trauma is essential to maximizing limb salvage rates and avoiding unnecessary morbidity and mortality.
10.1 Epidemiology
Traumatic injuries to the forearm and hand can be penetrating or blunt, which represent 4–36 % of upper extremity arterial trauma [1–3]. Because of the close proximity of the vessels and the nerves as they travel in the arm, injuries are rarely just vascular in nature, often complicating not only the presentation but also the long-term outcome. If not treated in a timely fashion and properly, such injuries can lead to loss of function, loss of limb, or even death [4, 5].
Patients with injuries to the forearm and hand can present in many different ways, from a seemingly clean laceration across the wrist or digit to a crush injury involving the hand and forearm (Fig. 10.1).


Fig. 10.1
(a) Laceration across the wrist with transection of radial artery, median nerve, and flexor tendons. (b) Industrial crush injury with multisystem, segmental damage
Injuries to the forearm and hand are often reported as part of upper extremity injuries, with brachial artery injuries accounting for 40–55 % and radial and ulnar arterial injuries 4–36 % of the injuries, with about 67 % resulting from penetrating trauma [2–4, 6]. Though it is associated with lower mortality, upper extremity injuries have a high amputation rate [7]. On the other hand, several studies have reported that vascular extremity trauma due to blunt mechanism leads to worse outcomes than penetrating injury [8]. This is likely due to the higher energy associated with crushing injuries and the higher potential for concomitant orthopedic trauma or soft tissue loss. The mortality rate of patients with upper extremity vascular injury is primarily related to concomitant injuries such as head injury or abdominal trauma. Morbidity with upper extremity injuries, and especially with the forearm and hand, is closely associated with damage to the accompanying nerve, tendons, and associated bone fractures.
10.2 Etiology
The most common cause of forearm and hand vascular injury is penetrating trauma secondary to gunshot wounds and lacerations from stab wounds or glass. As mentioned previously, blunt trauma is not a common cause of vascular injury. As a result, vascular compromise can be easily missed during the initial assessment of a bluntly injured extremity. Therefore, a basic neurovascular exam is a critical component of any extremity exam, regardless of the indication for the assessment or complaint. One consideration that should raise the index of suspicion is the amount of force associated with the blunt trauma. Closed bone fractures or dislocations can be associated with arterial injuries. These types of injuries result in intimal tears and subsequent thrombosis of the vessels without a frank of obvious vascular insult (Fig. 10.2) [9, 10]. An example is hypothenar hammer syndrome resulting from repetitive blunt trauma to the palm and subsequent injury to the ulnar artery via the same mechanism stated above [11].
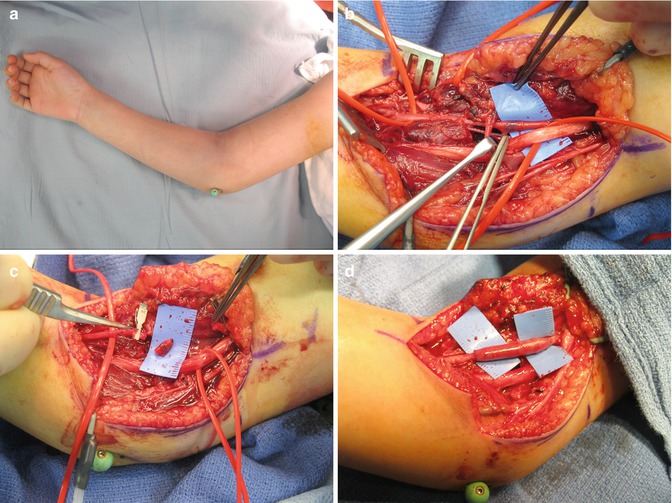
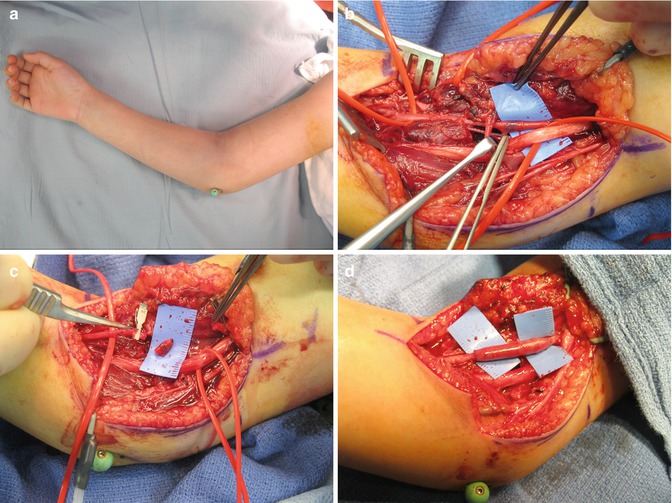
Fig. 10.2
(a) An 8-year-old girl treated for a closed supracondylar humerus fracture with closed reduction and percutaneous pin fixation. Postoperative examination revealed the extremity distal to the elbow to be ischemic. Urgent transfer was made. (b) The segment of brachial artery just proximal to the bifurcation is noted to have a thrombus within it. (c) The segment of brachial artery associated with the thrombus is presumed to have intimal damage given the blunt mechanism of injury and is resected. (d) A local vein graft is reversed and used to bypass the arterial gap created by debridement in a tension-free manner. Healing was uneventful
Injuries involving the hand and fingers usually often require microsurgical skills because of the small and delicate nature of the vessels, and therefore a hand or reconstructive surgeon is often involved. A basic understanding of the anatomy and surgical principles is still valuable when managing polytrauma patients with vascular injuries to the upper extremity.
10.3 Anatomy/Physiology
The brachial artery, a continuation of the axillary artery, divides just distal to the elbow into the radial and ulnar arteries. Prior to its bifurcation, it gives off collateral branches around the elbow. In the distal aspect, the brachial artery is adjacent to the median nerve (Fig. 10.3).
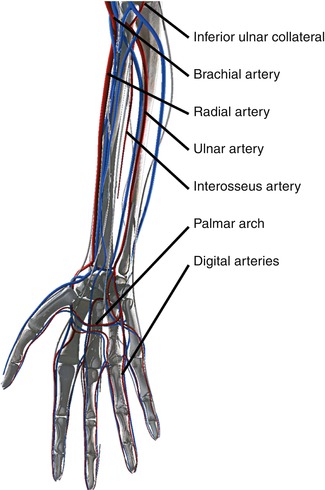
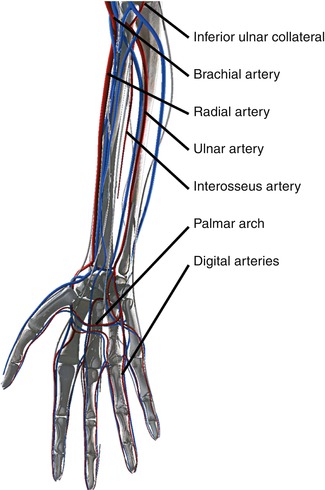
Fig. 10.3
Arterial anatomy of the ventral forearm and hand
Within the forearm, the radial artery begins near the neck of the radius and passes deep to the brachioradialis muscle, traveling distally on the anterior-radial part of the forearm. This serves as a landmark for the division between the anterior and posterior compartments of the forearm. As it approaches the wrist, it becomes more superficial and travels between the flexor carpi radialis and brachioradialis tendons and enters the wrist through the anatomical snuffbox and between the heads of the first dorsal interosseous muscle of the hand. It passes anteriorly between the heads of the adductor pollicis and becomes the deep palmar arch, which in turn will join with the deep branch of the ulnar artery.
As the radial artery travels down the forearm, it gives off several branches. In the forearm, the recurrent radial artery is the first branch, which will anastomose to the collateral arterial system around the elbow. Next, the palmar carpal branch arises near the lower border of the pronator quadratus and the superficial palmar branch just as it winds to the radial side of the wrist. At the wrist, the dorsal carpal branch and first dorsal metacarpal artery are noted and in the hand, the princeps pollicis artery, radialis indicis, and deep palmar arch.
The artery can be palpated on the radial aspect of the wrist, just radial to the flexor carpi radialis tendon, and in the anatomical snuffbox, and if during physical examination a pulse is present, it has been estimated to correlate with a systolic blood pressure of greater than 70 mmHg [12].
The ulnar artery is the larger branch of the two and runs under the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis but over the brachialis and flexor digitorum profundus. As the brachialis bifurcation, it travels next to the median nerve on the medial side for about 2.5 cm and reaches the ulnar aspect of the forearm about midway between the elbow and wrist. It continues to travel distally on the ulnar border over the flexor digitorum profundus between the flexor carpi ulnaris and flexor digitorum superficialis. About a third of the way down the forearm, the ulnar nerve travels on the medial side of the artery. At the wrist, it enters Guyon’s canal, crossing the transverse carpal ligament on the radial side of the pisiform bone, and then divides into two branches: the superficial one which forms the superficial palmar arch and the deep branch that joins the deep palmar arch (Fig. 10.4).
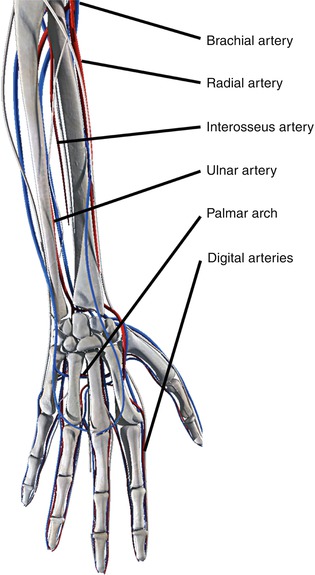
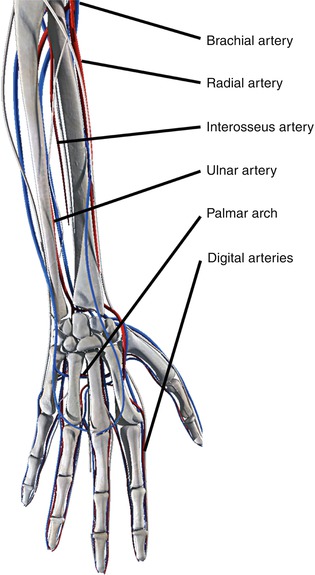
Fig. 10.4
Arterial anatomy of the dorsal forearm and hand
The superficial palmar arch lies deep to the palmar fascia and gives rise to the volar common digital arteries and branches to the intrinsic muscles of the hand. Distally, the common digital arteries bifurcate into the proper digital arteries. Each digit has a radial and ulnar digital artery supplying it. The deep palmar arch lies at the base of the metacarpals, deep to the flexor tendons. It provides blood supply to the thumb and radial half of the index finger by the first metacarpal artery.
10.4 Clinical Assessment
Upon initial evaluation of a patient and following advanced trauma life support (ATLS) approach by the American College of Surgeons, during secondary survey, a thorough assessment of the extremity is undertaken [13, 14]. If persistent bleeding is present, direct pressure can be applied, or if hemorrhaging, then a tourniquet or blood pressure cuff should be placed proximal to the injury and inflated at least 50 mmHg above systolic pressure (usually 200–250 mmHg). Two issues surrounding tourniquet use are the proper location and associated tourniquet pain. The position of the tourniquet, whether on the forearm or upper arm, is equally effective in controlling bleeding and well tolerated [15, 16]. Under no circumstances should hemostats or any kind of clamp be used to control bleeding from the arm or forearm. The risk of iatrogenic injury to adjacent nerves is very high in this setting. A thorough history and physical examination, if able, should be obtained (Table 10.1).
Table 10.1
History and physical exam are the initial most important steps when assessing a patient with signs of vascular injury
History | Physical exam |
|---|---|
Mechanism of injury | Radial and ulnar pulses – Allen’s test |
Time | Capillary refill |
Handedness | Warmth |
Occupation | Turgor |
Hand/wrist posture – tenodesis effect | |
Sensation – radial, ulnar, median distribution | |
Tendon exam |
The classic physical exam features of a vascular injury include diminished or absent distal pulses, a history of arterial bleeding, large or expanding hematoma, bruit at the site or injury, injury to anatomically related nerves, and injury in close proximity to a major artery [17]. These and other clinical signs have subsequently been stratified as “hard” and “soft” signs on their prediction of arterial injury in extremities, as shown in Table 10.2 [10]. The presence of a “hard” sign of vascular injury mandates immediate surgical intervention and repair, while “soft” signs are less specific and often need further studies to either confirm or exclude vascular injury [10].
Table 10.2
Clinical signs for the prediction of arterial injuries in extremities
“Hard” signs | “Soft” signs |
|---|---|
Active or pulsatile hemorrhage | Moderate hemorrhage occurring at the scene of injury |
Pulsatile or expanding hematoma | Stable and nonpulsatile hematoma |
Thrill or bruit (suggesting an AV fistula) | Proximity of wound to a major vessel |
Evidence of ischemia (pallor, paresthesia, paralysis, pain, and poikilothermia) | Peripheral neurological deficit |
Diminished or absent pulses | Asymmetric extremity blood pressures |
Presence of shock/hypoperfusion | |
Associated fracture or dislocation |
The hand is perfused by the ulnar and radial arteries which terminate as the palmar arches, as previously described. In order to determine whether a patent palmar arch is present, an Allen’s test should be performed (Fig. 10.5) [18]. This is done by applying firm pressure to both the ulnar and radial arteries just proximal to the wrist crease while the patient opens and closes his hand several times, until blanching is noted. The patient is asked to gently open his hand, in a position of rest, just short of full finger extension. The pressure over the ulnar artery is released while keeping pressure on the radial side, and perfusion of the hand is noted. This is then repeated but this time releasing the radial artery instead while holding pressure over the ulnar artery. Perfusion of the hand should take 5–10 s to suggest an intact palmar arch. Though it is an easy and simple exam to perform at the bedside, it is subjective and operator dependent, as shown by Benit et al. with up to 27 % of the population showing a discontinuous palmar arch based on this exam [19].
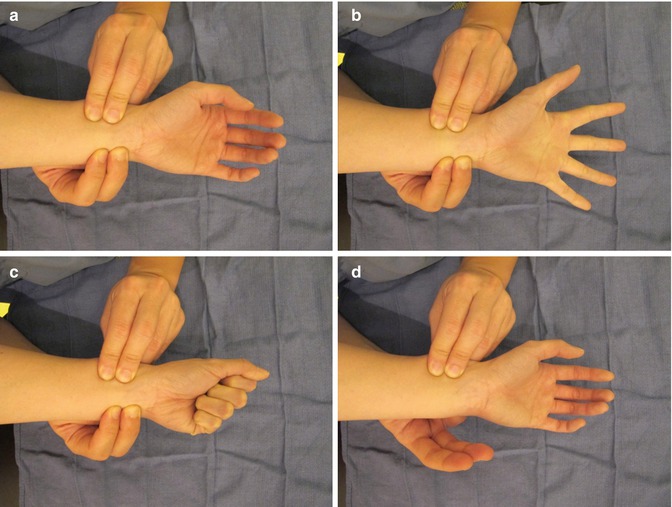
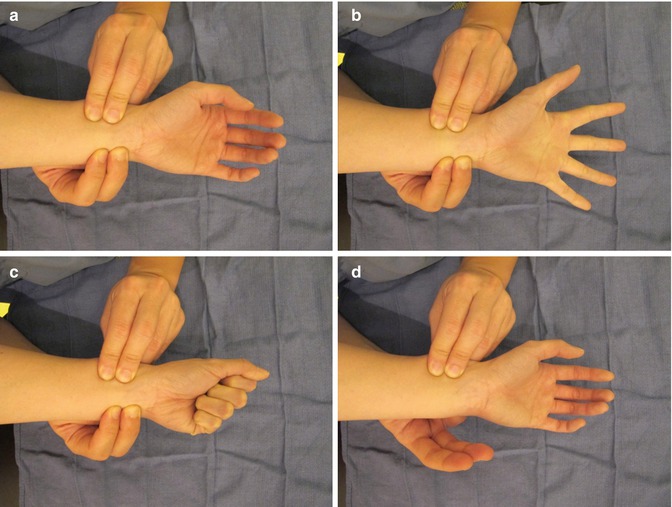
Fig. 10.5
Allen’s test. (a) Firm pressure applied to both sides of the wrist over the ulnar and radial arteries while (b) opening and closing the hand. (c) Ulnar artery pressure is released and time for capillary refill of the hand is noted. (d) This is then repeated with the radial artery released while pressure is maintained in the ulnar side
Evaluation of the vascular supply to the digits can be done in a similar fashion. Color, temperature, and turgor should be quickly assessed, while capillary refill can be used to assess adequate perfusion. It is generally brisk and less than 2 s. Another clinical test to assess blood flow to the digits is the pinprick test, usually done on an insensate finger or when the patient is anesthetized. Perfusion of the nail bed, which can be readily visualized through the nail plate, is helpful in darker-skinned patients. Allen’s test, similar to the one used to evaluate for palmar arch patency, can be performed on the digits. The digit is exsanguinated by flexing it, and then the radial and ulnar digital arteries at the base of the digit are occluded. With release of either artery, it should result in brisk capillary refill to the digit. However, Allen’s test is rarely required to determine if perfusion to a single digit is adequate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


