FIGURE 34.1 Normal anatomy of the forearm and hand arteries, including the deep and superficial palmar arches of the hand.
TABLE 34.1 Prevalence of Incomplete Superficial and Deep Palmar Arches from Cadaver Studies
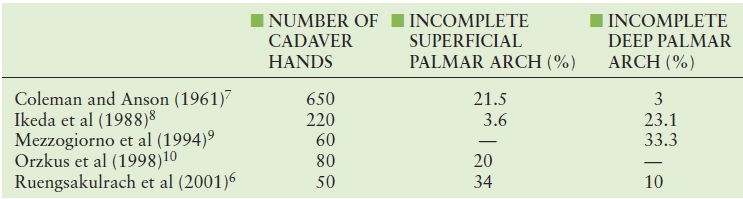
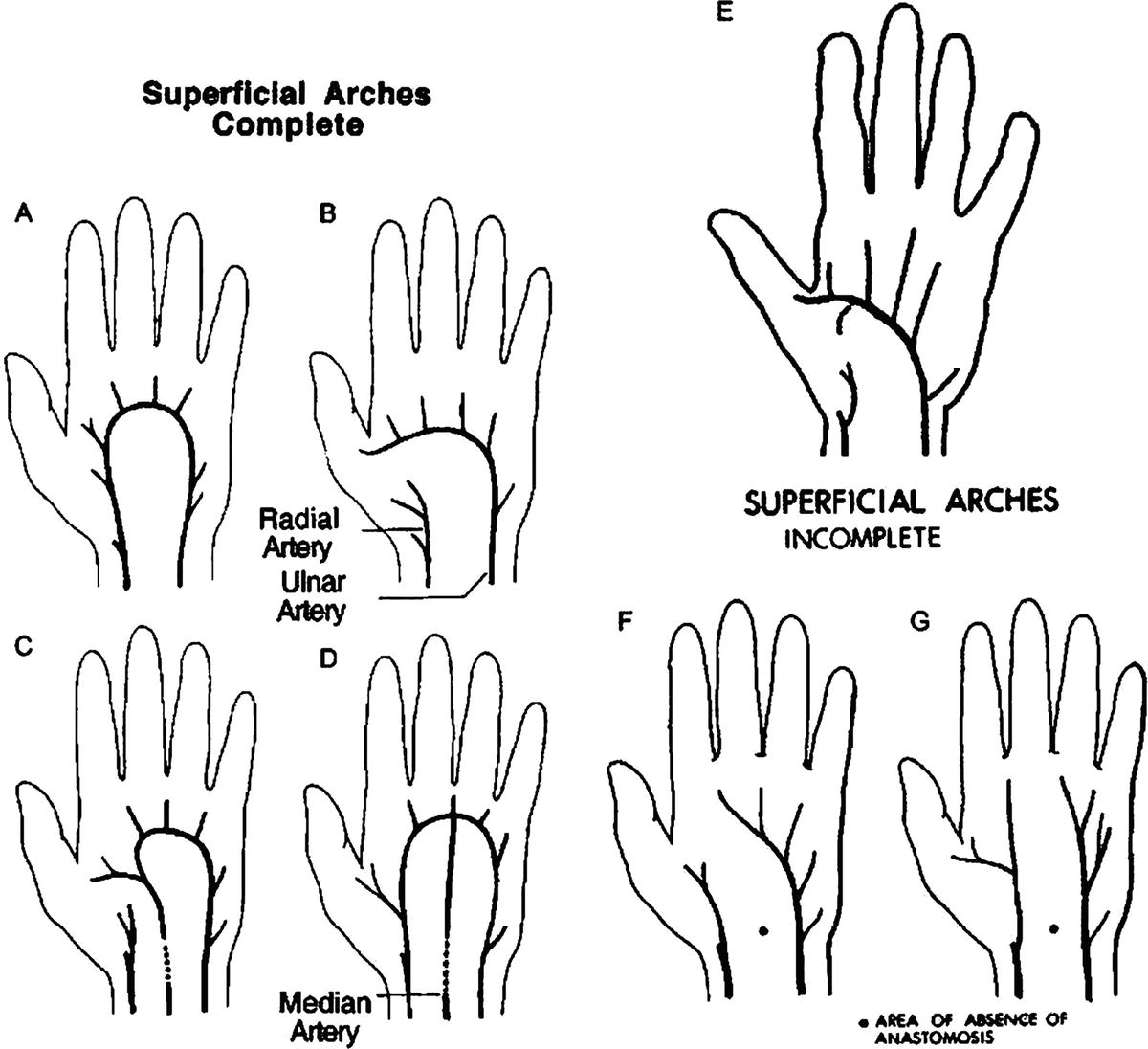
FIGURE 34.2 Examples of variations of the superficial palmar arch.
(From Gellman H, Botte MJ, Shankweiler J, et al. Arterial patterns of the deep and superficial palmar arches. Clin Orthop 2001;383:41–46, used with permission.)
TABLE 34.2 Summary of Anatomical Variants Found in a Cadaver Study of 384 Limbs
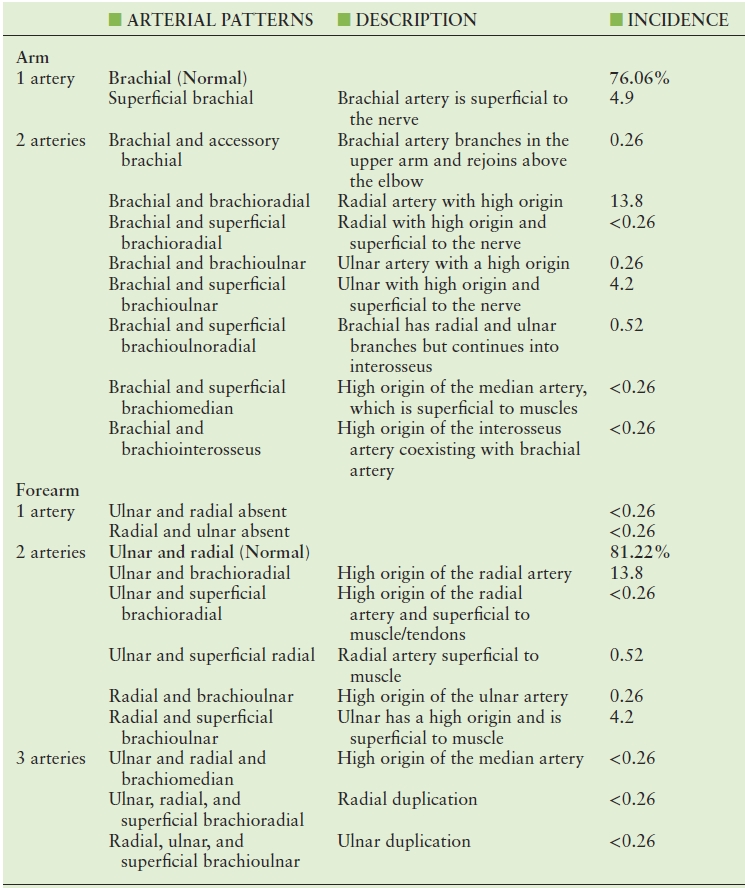
Adapted from Rodriguez-Niedenfuhr M, Vazquez T, Nearn L, et al. Variations of the arterial pattern in the upper limb revisited: A morphological and statistical study, with a review of the literature. J Anat 2001;199:547–566.
NONINVASIVE DIAGNOSTIC APPROACHES
Several protocols, with varying equipment and algorithms, have been described in an attempt to provide information on the upper extremity arterial circulation needed by the cardiac surgeon.14 The simplest method is Allen’s test. Allen’s test, first described in 1929, was originally performed by first having the patient make a tight fist to empty blood from the hand.15 The radial and ulnar arteries were then digitally compressed and the hand was opened, resulting in blanching of the palm (Fig. 34.3). After a few seconds, compression on the ulnar artery was released, and the length of time required for color to return to the palm was recorded (Fig. 34.4). In 2000, Jarvis et al5 described the limitations of this method. There was disagreement on the cutoff point between positive and negative tests, which varied between 5 and 10 seconds. They also reported observer bias in deciding when the normal palmar rubor had returned and found that false-negative results could occur if the wrist was hyperextended. Kamienski and Barnes16 reported a 73% false-positive rate due to subjectivity of the test or observer bias.

FIGURE 34.3 Allen’s test shows open left hand with radial and ulnar artery compression producing pallor of the hand and fingers.
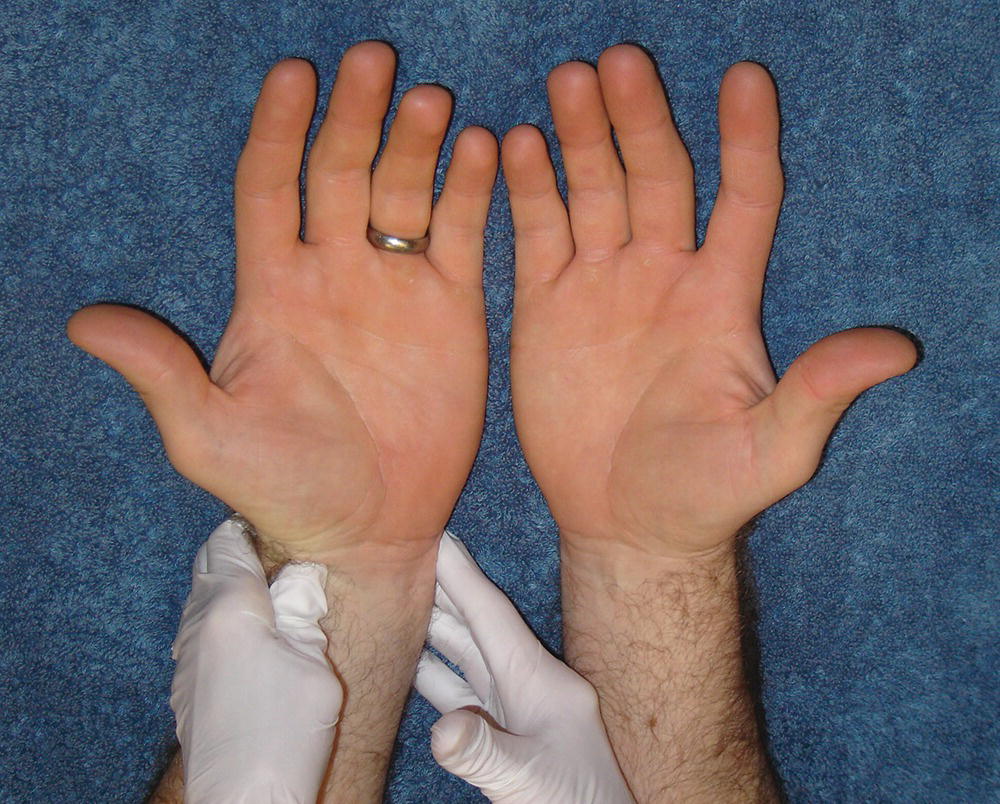
FIGURE 34.4 Allen’s test shows open left hand with release of ulnar artery compression while radial artery compression is maintained. Note return of normal color to the hand.
Prior to the report of Jarvis et al,5 Starnes et al17 compared a “modified” Allen’s test with direct digit pressure measurement. This modified Allen’s test was considered positive if radial artery compression caused a decrease in the audible Doppler flow signal from the superficial palmar arch. The change in the Doppler flow signal was compared with the digit pressure difference before and after radial artery compression (Fig. 34.5). A pressure drop in the first or second digit of 40 mm Hg or more suggested an inadequate collateral pathway in the hand. Both of these tests attempted to reduce the subjectivity noted by Jarvis et al5 and Kamienski and Barnes.16 Starnes et al17 reported a high false-positive rate of 50% with the modified Allen’s test and concluded that the change in digit pressure was more effective in avoiding complications after radial artery harvest. However, neither Starnes et al17 nor Jarvis et al5 were able to address specific anatomic variants or vessel diameters.
FIGURE 34.5 A digit blood pressure cuff and photoplethysmograph (PPG) are used to measure changes in the thumb pressure and volume pulses with and without manual compression of the radial artery.
In 2003, Sullivan et al18 compared changes in peak systolic velocity in the ulnar artery at the wrist with changes in digit pressures in response to radial artery compression. This study showed a poor correlation between ulnar artery velocities and digit pressures. For this reason, they favor the use of digit pressure measurement with and without radial artery compression. Their protocol includes segmental arm blood pressure measurements to identify arterial obstruction of the major arteries of the arm. The normal values for pressure measurements in the upper extremity were established by Sumner et al in 1979.19 Brachial, radial, and ulnar artery systolic pressures should differ by less than 15 mm Hg from side to side. A brachial artery systolic pressure difference of greater than 15 mm Hg suggests an obstruction involving the proximal arteries (brachial, axillary, subclavian, or innominate) on the side with the lower pressure. In addition, a gradient between adjacent levels in the same extremity (upper arm and forearm) of greater than 15 mm Hg is suggestive of obstruction between those two levels.
In 2004, Agrifoglio et al20 compared the modified Allen’s test with the snuffbox test using color duplex scanning. This was based on the theory that the region of the anatomic snuffbox is a junction between the dorsal branch of the radial artery and the deep palmar arch (Fig. 34.6). Duplex ultrasound with color flow allowed them to identify the dorsal branch. The snuffbox test included scanning of the radial artery in the snuffbox with and without ulnar artery compression. Radial artery flow was evaluated with compression, and reverse flow was considered evidence of good collateral circulation. Next, flow was measured in the palmar arch with radial artery compression; reverse flow in this artery indicated good perfusion of the superficial palmar arch. Lastly, the radial artery was scanned to rule out calcification or stenosis and to assess the diameter. In this study of 150 patients being evaluated for radial artery harvest, Allen’s test did not detect any abnormalities, whereas the snuffbox test detected inadequate collateral flow in 8 (5%). The radial artery was harvested in the remaining 142 patients without ischemic hand complications.
FIGURE 34.6 The arteries in the region of the anatomic snuffbox.
Abu-Omar et al21 were able to use 99% of all radial arteries in a group of 287 patients examined for bypass graft conduit. In their study, if Allen’s test was normal, they proceeded to surgery. If Allen’s test was abnormal, they performed a duplex scan to assess the radial and ulnar arteries. Only 15% of their patients had an abnormal Allen’s test. Of these 43 patients, 38 had normal duplex scans of the radial and ulnar arteries and went on to radial artery harvest. In the five remaining patients with an abnormal Allen’s test, the duplex examination identified stenosis or occlusion in either the radial or the ulnar arteries or both. These patients were not considered candidates for radial artery harvest. No postoperative ischemic complications occurred in any of the patients who underwent radial artery harvest in this study.
UNIVERSITY OF WASHINGTON PROTOCOL
The testing algorithm shown in Figure 34.7 is used to guide the vascular technologist through a three step process for determining the suitability of the radial artery for use as a coronary artery bypass graft conduit. The goals of this process are to assess the adequacy of collateral flow to the hand, detect significant occlusive lesions in the upper extremity arteries, and examine the radial artery to identify calcification and anatomic anomalies.
FIGURE 34.7 Testing algorithm for the radial artery evaluation prior to harvest.
Collateral flow in the hand is assessed with a modified Allen’s test. The modified Allen’s test is performed with duplex ultrasound by measuring ulnar artery peak systolic velocities with and without radial artery compression and radial artery peak systolic velocities with and without ulnar artery compression. Augmentation of velocities in the radial and ulnar arteries with the corresponding compression indicates adequate collateral flow and an intact palmar arch. We find this modification for assessing collateral flow to be effective in most patients. However, in equivocal cases, or if an increase in velocities is not detected, we perform the modified Allen’s test using a photoplethysmograph (PPG). This approach assesses changes in volume pulse waveforms in the thumb during radial artery compression, as shown in Figure 34.5. The PPG examination is not the initial method of choice for assessing the palmar arch because it requires additional equipment, time, and is less convenient for bedside examinations.
Significant upper extremity arterial obstruction is assessed with segmental limb blood pressures, and duplex scanning is used to measure the radial artery diameter and identify any anatomic anomalies of the upper extremity arteries. Calcification is identified with B-mode imaging and is recognized by highly echogenic vessel walls. The examination begins with the nondominant hand. Kohonen et al22 evaluated 33 patients with contraindications to radial artery harvest on the nondominant side using Doppler ultrasonography and PPG. They found that 73% of patients with contraindications on the nondominant side also had contraindications for harvest of the radial artery on the dominant side. If the radial artery to the nondominant hand is adequate by our criteria, a bilateral examination is usually not necessary. The findings are discussed with the cardiac surgeon before proceeding to a bilateral examination.
Patient Preparation
- Identify the nondominant hand to begin the examination.
- Query the length of conduit or number of grafts needed.
- Perform testing with the patient in the resting, supine position.
Equipment
- Blood pressure cuffs 10 and 12 cm in width
- Sphygmomanometer
- A 5-MHz continuous-wave Doppler transducer
- PPG and photocell
- Strip chart recorder
- Duplex ultrasound system
- Mid to superficial range linear array transducer (5 to 15 MHz)
Examination Technique
Step 1: Assess Collateral Flow in the Hand
Allen’s Test with Duplex Scanning
Evaluate collateral circulation to the hand with a duplex ultrasound system and a linear array transducer (Fig. 34.8). Place the transducer longitudinally along the lateral aspect of the wrist to locate the ulnar artery. Color flow is helpful for quickly visualizing small vessels; however, arterial pulsations can also be used for vessel identification. Obtain Doppler spectral waveforms using an insonation angle of 60 degrees to the vessel wall. Record ulnar artery waveforms continuously with and without radial artery compression. This same maneuver is performed with the radial artery while compressing the ulnar artery. During this process, the duplex image allows the vascular technologist to note differences in size (diameter) between the ulnar and the radial arteries. The ulnar artery is usually dominant (larger). If the ulnar artery appears small, diameter measurements are documented in the proximal, mid, and distal segments. In the case of a small ulnar artery, the surgeon may be reluctant to remove the radial artery. The peak systolic velocity response to compression maneuvers can be interpreted as follows.

FIGURE 34.8 Step 1 of the testing algorithm. The Allen’s test is performed with the duplex scanner (see text for details).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


