, Gregory D. Lewis2 and Gregory D. Lewis3
(1)
Harvard Medical School Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
(2)
Mass General Cardiopulmonary Exercise Laboratory, Cardiology Division, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
(3)
Harvard Medical School, Boston, USA
Abstract
The right ventricular-pulmonary vascular unit is a low resistance, high compliance system that is normally capable of accommodating large increases in blood flow with a minimal increment in pressure. The development of elevated pulmonary arterial pressures, either in unselected populations or in individuals with a variety of cardiopulmonary diseases, is increasingly recognized to be associated with a markedly increased risk of mortality. Regardless of the etiology, pulmonary hypertension leads to right ventricular dysfunction that is closely associated with impaired exercise capacity, renal and hepatic dysfunction. This chapter will briefly review the epidemiology and pathophysiology of pulmonary hypertension (PH) in addition to current diagnostic and treatment approaches with particular emphasis on PH arising in the setting of other cardiovascular diseases.
Abbreviations
6 MW
6 Minute Walk
APAH
Associated with Pulmonary Arterial Hypertension
BMP
Bone Morphogenic Protein
CCB
Calcium Channel Blockers
COPD
Chronic Obstruction Lung Disease
CTEPH
Chronic Thromboembolic Pulmonary Hypertension
DVT
Deep Venous Throbosis
FPAH
Familial Pulmonary Arterial Hypertension
HFpEF
Heart Failure with preserved Ejection Fraction
IPAH
Idiopathic Pulmonary Arterial Hypertension
JVP
Jugular Venous Pressure
LFT
Liver Function Test
LVEF
Left Ventricular Ejection Fraction
mPAP
Mean Pulmonary Artery Pressure
NO
Nitric Oxide
NYHA
New York Heart Association
PA
Pulmonary Artery
PAH
Pulmonary Arterial Hypertension
PAP
Pulmonary Artery Pressure
PCH
Pulmonary Capillary Hemangiomatosis
PCWP
Pulmonary Capillary Wedge Pressure
PDE-5
Phosphodiesterase-5
PE
Pulmonary Embolism
PH
Pulmonary Hypertension
PVOD
Pulmonary Veno-Occlusive Disease
PVR
Pulmonary Vascular Resitance
RV
Right Ventricle
RVEF
Right Ventricular Ejection Fraction
TAPSE
Tricuspid Annular Plane Systolic Excursion
TTE
Transthoracic echocardiogram
WHO
World Health Organization
Introduction
The right ventricular-pulmonary vascular unit is a low resistance, high compliance system that is normally capable of accommodating large increases in blood flow with a minimal increment in pressure. The development of elevated pulmonary arterial pressures, either in unselected populations or in individuals with a variety of cardiopulmonary diseases, is increasingly recognized to be associated with a markedly increased risk of mortality. Regardless of the etiology, pulmonary hypertension leads to right ventricular dysfunction that is closely associated with impaired exercise capacity, renal and hepatic dysfunction. This chapter will briefly review the epidemiology and pathophysiology of pulmonary hypertension (PH) in addition to current diagnostic and treatment approaches with particular emphasis on PH arising in the setting of other cardiovascular diseases.
1.
Overview of pulmonary hypertension
2.
Diagnostic work up
3.
WHO Group Classification with particular attention to:
(a)
Idiopathic Arterial Pulmonary Hypertension
(b)
Pulmonary Venous Hypertension
(c)
Hypoxia Associated Pulmonary Hypertension
(d)
Chronic Thromboembolic Pulmonary Hypertension
Definitions
A.
Pulmonary Hypertension (PH)
Definition: An abnormally high blood pressure within the arteries of the lungs
Hemodynamic diagnostic criteria
Mean pulmonary artery pressure > 25 mmHg.
B.
Pulmonary arterial hypertension (PAH)
Definition: A syndrome caused from restricted blood flow through the pulmonary circulation leading to elevation in pulmonary resistance and subsequent right heart failure. Hemodynamic characteristics include
Mean pulmonary artery pressure (PAP) >25 mmHg and
Pulmonary capillary wedge pressure (PCWP) or left ventricular end diastolic pressure ≤15 mmHg and
Pulmonary vascular resistance (PVR) >3 Woods units
C.
Pathology
Elevated PVR due to
loss of vascular luminal cross sectional area due to vascular remodeling from excessive cell proliferation and decreased rates of apoptosis
impaired endothelial function with excessive vasoconstriction (low nitric oxide and prostaglandin bioavailability, increased thromboxane A2) thrombosis in situ (platelets depleted of serotonin)
smooth muscle cell proliferation
2 hit hypothesis
Permissive genotype (i.e. Bone Morphogenic Protein [BMP] 2 mutation)
Second insult (i.e. thromboembolism, toxin, infection)
Histology
Predominantly small pulmonary arteries
Intimal hyperplasia, medial hypertrophy, adventitial proliferation, thrombosis in situ, inflammation
Genetics
10 % of cases are familial
2 known genetic mutations: BMP-2 and activin-like kinase 1
D.
World Health Organization (WHO) Group Classifications
1.
Pulmonary arterial hypertension (PAH3)
1.1.
Idiopathic (IPAH)
1.2.
Familial (FPAH)
1.3.
Associated with (APAH):
1.3.1.
Collagen vascular disease
1.3.2.
Congenital systemic-to-pulmonary shunts
1.3.3.
Portal hypertension
1.3.4.
HIV infection
1.3.5.
Drugs and toxins
1.3.6.
Other (thyroid disorders, glycogen storage disease, Gaucher disease, hereditary hemorrhagic telangiectasia, hemoglobinopathies, myeloproliferative disorders, splenectomy)
1.4.
Associated with significant venous or capillary involvement
1.4.1.
Pulmonary veno-occlusive disease (PVOD)
1.4.2.
Pulmonary capillary hemangiomatosis (PCH)
1.5.
Persistent pulmonary hypertension of the newborn
2.
Pulmonary hypertension with left heart disease
2.1.
Left-sided atrial or ventricular heart disease
2.2.
Left-sided valvular heart disease
3.
Pulmonary hypertension associated with lung diseases and/or hypoxemia
3.1.
Chronic obstructive pulmonary disease
3.2.
Interstitial lung disease
3.3.
Sleep-disordered breathing
3.4.
Alveolar hypoventilation disorders
3.5.
Chronic exposure to high altitude
3.6.
Developmental abnormalities
4.
Pulmonary hypertension due to chronic thrombotic and/or embolic disease (CTEPH)
4.1.
Thromboembolic obstruction of proximal pulmonary arteries
4.2.
Thromboembolic obstruction of distal pulmonary arteries
4.3.
Non-thrombotic pulmonary embolism (tumor, parasites, foreign material)
5.
Miscellaneous
5.1.
Sarcoidosis,
5.2.
Histiocytosis X
5.3.
Lymphangiomatosis
5.4.
Compression of pulmonary vessels
Diagnostic Work Up
A.
History
Symptoms: Dyspnea on exertion, fatigue, chest pain, syncope, palpitations, lower extremity edema (Table 22-1)
Table 22-1
Medical history associated with pulmonary hypertension
Group I—Pulmonary arterial hypertension
Group II—PH with left heart involvement
Group III—PH associated with lung disease and/or hypoxia
Group IV—PH associated with to chronic thrombotic and/or embolic disease
Group V—Miscellaneous
Hemoglobinopathies
Atrial or ventricular disease
COPD
Pulmonary embolism
Sarcoidosis
Sickle cell
Systolic heart failure
Interstitial lung disease
Histiocytosis X
β-thalessemia+/+
Heart failure with preserved EF
Obstructive sleep apnea
Lymphangiomatosis
Hereditary spherocytosis
Constrictive or restrictive disease
Compression of pulmonary vessels
Family history of PAH (BMPR2 mutation)
Dilated cardiomyopathy
Adenopathy
Connective tissue disease
Valvular disease
Tumor
Limited cutaneous form of systemic sclerosis
Mitral regurgitation
Fibrosing mediastinitis
SLE
Mitral stenosis
MCTD
RA
Liver disease/cirrhosis
HIV
Congenital heart disease with systemic shunt
Drugs/toxin
Fenfluramine
Rapeseed oil
Methamphetamine
Cocaine
Other
Hereditary hemorrhagic telangiectasia
Glycogen storage disease
Gaucher disease
Thyroid disorders
Splenectomy
B.
Physical Exam (Table 22-2 [1])
Early PH | Moderate to severe PH | Advanced PH with RV failure |
|---|---|---|
Accentuated S2 (best heard at apex) | Holosystolic murmur that increases with inspiration | Right ventricular S3 |
Early systolic click | Increased jugular ‘v’ waves | Distension of jugular veins |
Mid systolic ejection murmur | Pulsatile liver | Heptomegaly |
Left parasternal lift | Diastolic murmur | Peripheral edema |
Right ventricular S4 | Hepatojugular reflux | Ascites |
Increased jugular ‘a’ wave | Hypotension, decreased pulse pressure, cool extremities |
C.
Diagnostic Studies
CXR
Right ventricular (RV) enlargement, peripheral hypovascularity, hilar enlargement
ECG
Right ventricular hypertrophy, right atrial enlargement, right axis deviation
Trans-thoracic echocardiography (Fig. 22-1)
Figure 22-1
Echocardiographic differentiation of elevated RV systolic pressure
Further testing for diseases associated with pulmonary hypertension
ANA & other connective tissue disease serologies
Sleep study
Liver function tests
Pulmonary function tests
V/Q scan
HIV
D.
Right heart catheterization
Assess pulmonary vascular resistance to isolate pre-capillary and post-capillary contributions to pulmonary artery pressure
Pulmonary arterial hypertension is characterized by elevations in both mean pulmonary artery pressure (mPAP) and transpulmonary gradient (pre-capillary pulmonary hypertension) (Fig. 22-2) [35]
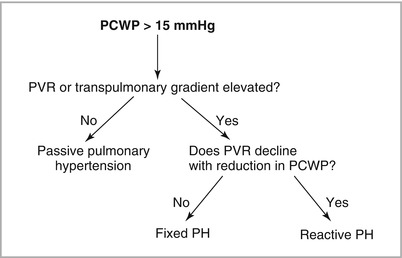
Figure 22-2
Diagnosing pulmonary venous/passive/post-capillary hypertension vs pulmonary arterial/pre-capillary hypertension (Adapted from Chatterjeee and Lewis [35])
mPAP>25 mmHg
PCWP <15 mmHg
PVR > 3 Woods units
Passive pulmonary hypertension (post-capillary pulmonary hypertension)
mPAP >25 mmHg
PCWP >15 mmHg
PVR <3 Woods Units
Mixed (or “Out of Proportion”) pulmonary hypertension
mPAP >25 mmHg
PCWP >15 mmHg
PVR >3 Woods Units
Pulmonary hypertension can be due to high pulmonary flow in the setting of high cardiac output
Assess for significant intra-cardiac shunt (O2 saturations from the superior vena cava, right ventricle, pulmonary artery, and femoral artery)
Assess for low cardiac output (<2.1 L/min/m2)
Assess for vasoreactivity to pulmonary vasodilators (Table 22-3)
Nitric oxide
Adenosine
Epoprostenol
Route of administration
Inhaled
IV infusion
IV infusion
Dose titration
Nne
50 mcg/kg/min every 2 min
2 ng/kg/min every 10–15 min
Dose range
20–40 ppm for 5 min
50–250 mcg/kg/min
2–10 ng/kg/min
Side effects
↑ Left heart filling pressures< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
