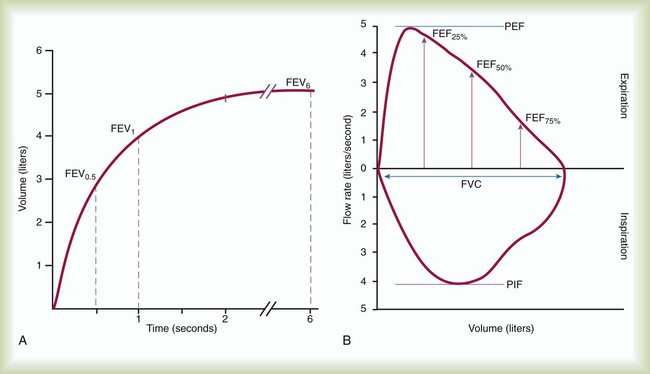
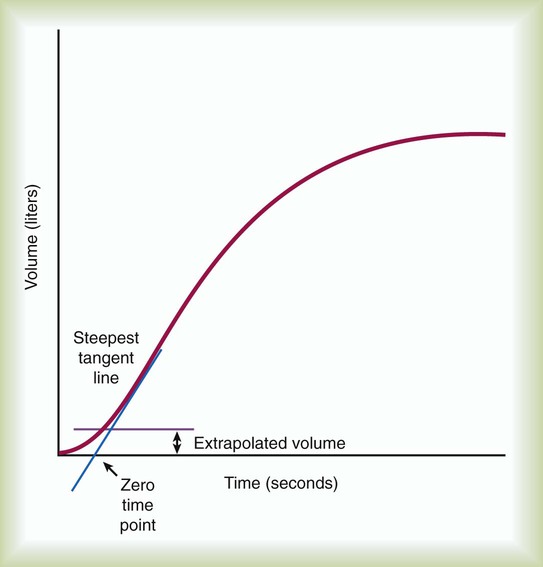
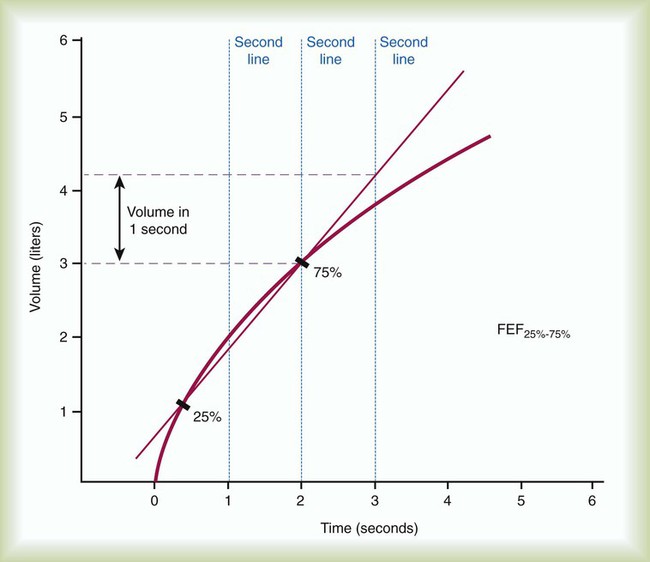
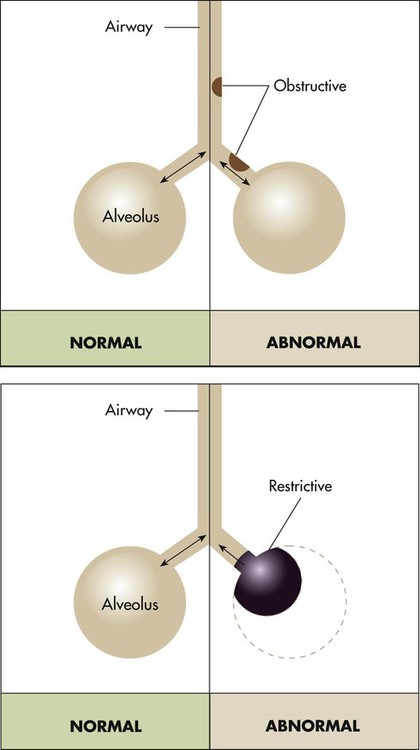
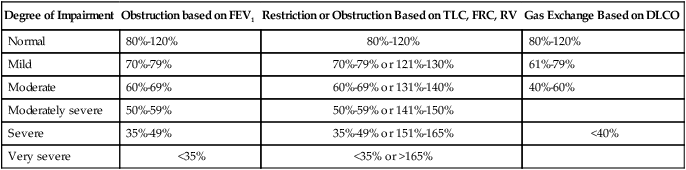
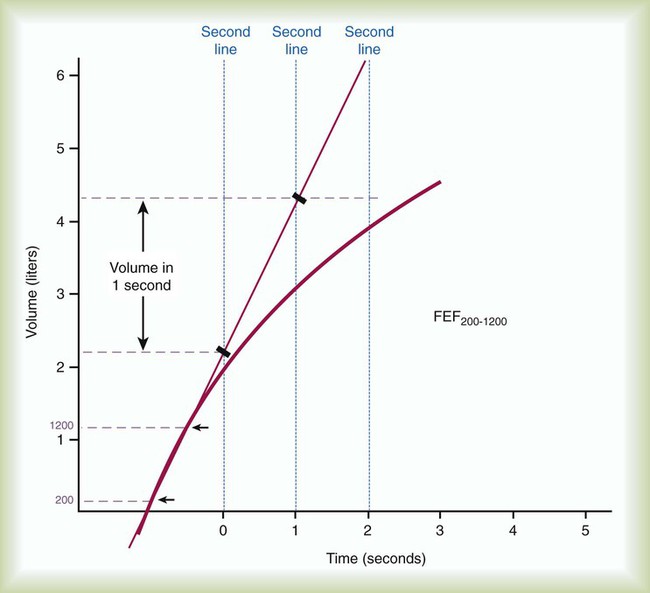
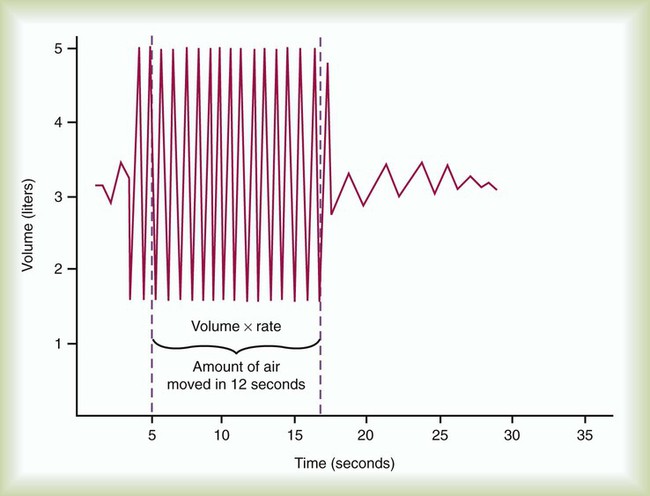
After reading this chapter you will be able to: 1. The diaphragm and thoracic muscles must be capable of expanding the thorax and lungs to produce a subatmospheric pressure. 2. The airways must be unobstructed to allow gas to flow into the lungs and reach the alveoli. 3. The cardiovascular system must circulate blood through the lungs and ventilated alveoli. 4. O2 and CO2 must be able to diffuse through the alveolar-capillary membrane. Pulmonary function tests can provide valuable information about these important individual processes that support gas exchange. Various measurements are available to aid in the diagnosis and assessment of pulmonary diseases, to determine the need for therapy, and to evaluate the effectiveness of respiratory care. For respiratory therapists (RTs), knowledge of these tests and the ability to interpret the measurements are essential for assessing patients objectively and for planning and implementing effective patient care. The key terms used in this chapter are terms adopted and defined by the pulmonary medical community and should become the standard vocabulary of all RTs.1 Generally, the primary purposes of pulmonary function testing are to identify pulmonary impairment and to quantify the severity of pulmonary impairment if present.2 Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease (Box 19-1). The indications for pulmonary function testing are as follows: • To identify and quantify changes in pulmonary function. The most common purposes of pulmonary function testing are to detect the presence or absence of pulmonary disease, to classify the type of disease as either obstructive or restrictive, and to quantify the severity of pulmonary impairment as mild, moderate, severe, or very severe. Over time, pulmonary function tests help quantify the progression or the reversibility of the disease.3 • To evaluate need and quantify therapeutic effectiveness.4 Pulmonary function tests may aid clinicians in selecting or modifying a specific therapeutic regimen or technique (e.g., bronchodilator medication, airway clearance therapy, rehabilitation exercise protocol). Clinicians and researchers use pulmonary function tests to measure changes in lung function objectively before and after treatment. • To perform epidemiologic surveillance for pulmonary disease. Screening programs may detect pulmonary abnormalities caused by disease or environmental factors in general populations, in people in occupational settings, in smokers, or in other high-risk groups. In addition, researchers have determined what normal pulmonary function is by measuring the pulmonary function of healthy people.5 • To assess patients for risk of postoperative pulmonary complications. Preoperative testing can identify patients who may have an increased risk of pulmonary complications after surgery.6 Sometimes the risk of complications can be reduced by preoperative respiratory care, and sometimes the risk may be significant enough to rule out surgery. • To determine pulmonary disability.7 Pulmonary function tests can also determine the degree of disability caused by lung diseases, including occupational diseases such as pneumoconiosis of coal workers. Some federal entitlement programs and insurance policies rely on pulmonary function tests to confirm claims for financial compensation. There are also contraindications to pulmonary function testing.4 Patients with acute, unstable cardiopulmonary problems, such as hemoptysis, pneumothorax, myocardial infarction, and pulmonary embolism, and patients with acute chest or abdominal pain should not be tested. Testing could be harmful if needed treatment would be delayed. Patients who have nausea and who are vomiting should not be tested because there is a risk of aspiration. Testing for patients who have had recent cataract removal surgery should be delayed because changes in ocular pressure may be harmful to the eye. Pulmonary function testing requires patient effort and cooperation. Patients with dementia or confusion may not achieve optimal or repeatable results. Pulmonary function testing should not be performed if valid and reliable results cannot be predicted. In patients who are acutely ill or who have recently smoked a cigarette, the test validity of measuring the forced vital capacity (FVC) may be hindered. Pulmonary function testing provides the basis for classifying pulmonary diseases into two major categories, obstructive pulmonary disease and restrictive pulmonary disease. These two types of lung diseases sometimes occur together as a mixed impairment. Obstructive and restrictive types of lung diseases differ in several important ways. Figure 19-1 shows normal lungs with the pathophysiologic aspects of obstructive lung diseases and restrictive lung diseases, and the differences are summarized in Table 19-1. The primary problem in obstructive pulmonary disease is an increased airway resistance (Raw). Raw is the difference in pressure between the ends of the airways divided by the flow rate of gas moving through the airway, according to the following formula: Raw = ΔP/ TABLE 19-1 Comparison of Obstructive and Restrictive Types of Pulmonary Diseases There is an inverse relationship between Raw and flow rates ( Determining if the patient’s value is within 1 or 2 standard deviations of the predicted normal value is an alternative method used in some laboratories. The predicted percentage or the number of standard deviations from the predicted normal value can be used to quantify severity of impairment. Typical degrees of severity are listed in Table 19-2. TABLE 19-2 Severity of Pulmonary Impairments Based on a Percentage of Predicted Normal Values Pulmonary function testing is considered safe, but there is potential to transmit infective microorganisms to patients and technologists.8 Transmission can occur by direct or indirect contact. Standard precautions should be applied because of the potential exposure to saliva or mucus, which could possibly contain blood or other potentially hazardous microorganisms. Patients with oral lesions pose the greatest potential hazard, and patients with compromised immune systems are at the greatest risk. Practitioners should wear gloves when handling potentially contaminated mouthpieces, valves, tubing, and equipment surfaces. When performing procedures on patients with potentially infectious airborne diseases, practitioners should wear a personal respirator or a close-fitting surgical mask, especially if the testing induces coughing. Practitioners should always wash their hands between testing patients and after contact with testing equipment. Although it is unnecessary to clean the interior surfaces of the testing instruments routinely between patients,9 the mouthpiece, nose clips, tubing, and any parts of the instrument that come into direct contact with a patient should be disposed, sterilized, or disinfected between patients. Any equipment surface showing visible condensation from exhaled air should be discarded, disinfected, or sterilized before reuse. When testing instruments are disassembled for cleaning and disinfecting, manufacturer recommendations should be considered, and recalibration may be necessary before testing resumes. The routine use of low-resistance, in-line barrier filters is controversial.10–12 Filters may be appropriate when internal surfaces of manifolds and valves proximal to mouthpieces are inaccessible or difficult to disassemble for cleaning and disinfecting. Filters provide visible evidence to reassure patients that their protection has been considered. Flow-measuring devices are commonly called pneumotachometers, although some practitioners reserve this term for only the device originally designed by Fleisch. These devices measure flow using a variety of unique principles. The Fleisch-type pneumotachometer measures the change in pressure as gas flows through a minimal, constant resistance according to the formula: Regardless of the type of device or the principle of measurement used, several important characteristics are common to all volume-measuring and flow-measuring devices. Having an understanding of these common characteristics provides RTs the ability to select and use these devices properly. Every measuring instrument has capacity, accuracy, error, resolution, precision, linearity, and output.14,15 The ideal instrument would have unlimited capacity to measure every pulmonary parameter, and it would have perfect accuracy and precision over its entire measurement range; there are no ideal instruments. The capacity of an instrument refers to the range or limits of how much it can measure. Most instruments are designed with capacities to measure volumes and flow rates of all adults. The accuracy of a measuring instrument is how well it measures a known reference value. For volume measurements, standard reference values are provided by a graduated 3.0-L calibration syringe.16 No measuring instrument is perfect, and there usually is an arithmetic difference between reference values and measured values. This difference is called the error. Accuracy and error are opposing terms; the greater the accuracy, the smaller is the error. Accuracy and error are commonly expressed as percentages, with their sum always equaling 100%. To determine percent accuracy and percent error, several reference values are measured, and the mean of the measured values is computed and compared with the reference values according to the following equations: In 1978, the American Thoracic Society (ATS) adopted the initial standards for diagnostic spirometers. These standards have been adopted by other medical organizations and government agencies. Updated most recently in 2005 in collaboration with the European Respiratory Society (ERS), the standards are now recognized internationally as the standards for the industry.17 Some instruments have been independently evaluated against the standards or compared with instruments that meet those standards. Regardless of the measuring principle used by the instrument or the purpose of the patient testing, RTs should use only devices that meet or exceed current ATS/ERS performance standards. According to the ATS/ERS standards, when measuring a slow VC, the spirometer should be able to measure for up to 30 seconds, and for the FVC, the time capacity should be at least 15 seconds. When measuring the VC, FVC, and forced expiratory volumes, a volume-measuring spirometer should have a capacity of at least 8 L and should measure volumes with less than a 3% error or within 50 ml of a reference value, whichever is greater. These standards, including the 8-L standard for capacity, also apply to children. A diagnostic spirometer that measures flow should be at least 95% accurate (or within 0.2 L/sec, whichever is greater) over the entire 0 to 14 L/sec range of gas flow. The standards are summarized in Table 19-3. TABLE 19-3 From Miller MR, Hankinson J, Brusasco V, et al: Standardisation of spirometry. Eur Respir J 26:319–338, 2005. In most pulmonary function laboratories, there are three components to pulmonary function testing: (1) performing spirometry for measuring airway mechanics, (2) measuring lung volumes and capacities, and (3) measuring the diffusing capacity of the lung (DL). For each component, there are various techniques and different types of equipment that make the measurements. When the purpose of the testing is to identify the presence and the degree of pulmonary impairment and the type of pulmonary disease, all three testing components are required. When the purpose of the testing is more limited, such as to assess postoperative pulmonary risk or to evaluate and quantify therapeutic effectiveness, the scope of measurement also is limited. Many pulmonary function laboratories also perform arterial blood gas analysis (see Chapter 18), and some laboratories provide more specialized and advanced tests, such as bronchial challenge tests and exercise stress tests. Spirometry includes the tests of pulmonary mechanics—the measurements of FVC, FEV1, several FEF values, forced inspiratory flow rates, and MVV. Measuring pulmonary mechanics is assessing the ability of the lungs to move large volumes of air quickly through the airways to identify airway obstruction. Some measurements are aimed at large intrathoracic airways, some are aimed at small airways, and some assess obstruction throughout the lungs. Measuring flow rates is a surrogate for measuring airways resistance according to the formula: Raw = ΔP ÷ Although performing tests of pulmonary mechanics is considered safe, some adverse reactions have occurred, including pneumothorax,18 syncope, chest pain, paroxysmal coughing, and bronchospasm associated with exercise-induced asthma.19 The contraindications for pulmonary function testing are primarily for testing mechanics. The ATS/ERS 2005 standards for spirometry17 specify the validity and reliability criteria of the measurements and accuracy and precision limits of the measuring equipment. These standards have been incorporated into the clinical practice guidelines of the AARC, medical societies, and government agencies.4,20–22 FVC is the most commonly performed test of pulmonary mechanics, and many measurements are made while the patient is performing the FVC maneuver (Figure 19-2). Measuring FVC often occurs under baseline or untreated conditions. For baseline testing, patients should temporarily abstain from bronchodilator medications. Short-acting bronchodilators (e.g., β-agonist albuterol, anticholinergic agent ipratropium bromide) should not be used for 4 hours before baseline spirometry, whereas long-acting β-agonist bronchodilators and oral therapy with aminophylline should be stopped for 12 hours. When a patient’s baseline results show airway obstruction, performing FVC after treatment (e.g., albuterol bronchodilator aerosol or metered dose inhaler) can help determine if the treatment is effective. The FVC maneuver is also performed repeatedly during bronchial provocation testing. FVC may be measured on a spirometer that measures volumes or flows, that presents a graph of volume and time or flow and volume, that is mechanical or electronic, and that has a calculator or computer. The forced expiratory VC sometimes is followed by a forced inspiratory VC to produce a complete image of forced breathing called a flow-volume loop.23 To ensure validity, each patient must perform a minimum of three acceptable FVC maneuvers. To ensure reliability, the largest FVC and second largest FVC from the acceptable trials should not vary by more than 0.150 L. To perform an FVC trial, the patient should inhale rapidly and completely to TLC from the resting FRC level. The forced exhalation of an acceptable FVC trial should begin abruptly and without hesitation. A satisfactory start of expiration is defined as an extrapolated volume at the zero time point less than 5% of FVC or 0.150 L, whichever is greater (Figure 19-3). The volume exhaled before the zero time point is called the extrapolated volume. To be valid, no more than 5% of the VC or 0.150 L is allowed to be exhaled before the zero time point. An acceptable FVC trial also is smooth, continuous, and complete. A cough, an inspiration, a Valsalva maneuver, a leak, or an obstructed mouthpiece while an FVC maneuver is being performed disqualifies the trial. FVC must be completely exhaled or an exhalation time of at least 6 seconds must occur for adults and children older than 10 years (longer times are commonly needed for patients with airway obstruction). A 3-second exhalation is acceptable for children younger than 10 years old. An end expiratory plateau must be obvious in the volume-time curve; the objective standard is less than 0.025 L exhaled during the final second of exhalation. Consistent with its definition, the largest acceptable FVC (BTPS) measured from the set of three acceptable trials is the patient’s FVC. During FVC testing, several other measurements are also made. FEV1 is a measurement of the volume exhaled in the first second of FVC (see Figure 19-2, A). To ensure validity of FEV1, the measurement must originate from a set of three acceptable FVC trials. The first second of forced exhalation begins at the zero time point (see Figure 19-3). To ensure reliability of FEV1, the largest FEV1 and second largest FEV1 from the acceptable trials should not vary by more than 0.150 L. Consistent with its definition, the largest FEV1 (BTPS) measured is the patient’s FEV1. The largest FEV1 sometimes comes from a different trial than the largest FVC. FEF200-1200 and FEF25%-75% represent average flow rates that occur during specific intervals of FVC. Both measurements can be made on a volume-time spirogram as the slope of a line connecting the two points in their subscripts. For FEF200-1200, the 200-ml point and the 1200-ml point are identified. A straight line is drawn connecting these points, and the line is extended to intersect two vertical time lines 1 second apart on the graph (Figure 19-4). The volume of air measured between the two time lines is FEF200-1200 in liters per second. The volume measured must be corrected to BTPS. FEF25%-75% is a measure of the flow during the middle portion of FVC, or the time necessary to exhale the middle 50%. For FEF25%-75%, the VC of the best curve is multiplied by 25% and 75%, and the points are identified on the tracing. A straight line is drawn connecting these points, and the line is extended to intersect two vertical time lines 1 second apart on the graph. The volume of air measured between the two time lines is FEF25%-75% in liters per second. The volume measured must be corrected to BTPS (Figure 19-5). PEF is difficult to identify on a volume-time graph of FVC. The peak flow is the slope of the tangent to the steepest portion of the FVC curve. PEF is easy to identify on a flow-volume graph as the highest point on the graph (see Figure 19-2, B).23 PEF is sometimes measured independently of FVC with a peak flowmeter. These devices are designed to indicate only the greatest expiratory flow rate. The validity of PEF rate is based on a preceding inspiration to TLC and a maximal effort. The FVC principles of ensuring reliability should apply to measurements of PEF rate. The two largest repeated measurements should agree within 5%. In addition to PEF rate, the other instantaneous flow rates, such as forced expiratory flow at 25% (FEF25%) of FVC, forced expiratory flow at 50% (FEF50%) of FVC, and forced expiratory flow at 75% (FEF75%) of FVC, during FVC are graphed on a flow-volume curve. When FVC is followed by a forced inspiratory VC, a flow-volume loop is produced (see Figure 19-2, B). On the flow-volume loop, the maximal forced inspiratory flow rate at 50% (FIF50%) of VC can be measured and compared with FEF50%. Another measurement of pulmonary mechanics is MVV. MVV is another effort-dependent test for which the patient is asked to breathe as deeply and as rapidly as possible for at least 12 seconds. MVV is a test that reflects patient cooperation and effort, the ability of the diaphragm and thoracic muscles to expand the thorax and lungs, and airway patency. Because of the potential for acute hyperventilation and fainting or coughing, the patient should be seated. Measuring systems that incorporate rebreathing may minimize hyperventilation. After a demonstration of the expected breathing pattern is performed, the patient should be instructed to breathe as rapidly and as deeply as possible for at least 12 seconds. The patient’s breathing is measured on a spirogram (Figure 19-6) or electronically for the specific number of seconds (t) and the volume (V) breathed when the MVV is converted to liters per minute. As with all volumes measured on a spirometer, the recorded values should be in BTPS conditions. The validity of MVV depends on the duration of the maneuver, which should be at least 12 seconds; the breathing frequency, which should be at least 90/min; and the average volume, which should be at least 50% of FVC. Patients should perform at least two MVV trials when the first trial does not exceed 80% of the subject’s FEV1 × 40, which may indicate less than maximal effort, or 80% of the predicted normal value, which may indicate disease. Reliability is shown when there is less than 20% variability between the two largest trials. The largest MVV (BTPS) should be reported.
Pulmonary Function Testing
 List the three categories of pulmonary function tests.
List the three categories of pulmonary function tests.
 State the primary purposes of pulmonary function testing.
State the primary purposes of pulmonary function testing.
 Describe the pathophysiologic patterns associated with obstructive and restrictive lung disease.
Describe the pathophysiologic patterns associated with obstructive and restrictive lung disease.
 State what is meant by the term spirometer, and list the parameters that can be measured by it.
State what is meant by the term spirometer, and list the parameters that can be measured by it.
 List and describe the four general principles that should be considered for pulmonary function tests.
List and describe the four general principles that should be considered for pulmonary function tests.
 List and describe the measurements that indicate pulmonary mechanics.
List and describe the measurements that indicate pulmonary mechanics.
 Describe the purpose and technique for the bronchial challenge test.
Describe the purpose and technique for the bronchial challenge test.
 List and describe the four volumes and four capacities that can be measured with pulmonary function testing.
List and describe the four volumes and four capacities that can be measured with pulmonary function testing.
 Describe the purpose and techniques used to measure diffusion capacity.
Describe the purpose and techniques used to measure diffusion capacity.
Pulmonary Function Testing
Purposes
Pathophysiologic Patterns
 .
.
Characteristic
Obstructive Disease
Restrictive Disease
Anatomy affected
Airways
Lung parenchyma, thoracic pump
Breathing phase difficulty
Expiration
Inspiration
Pathophysiology
Increased airway resistance
Decreased lung or thoracic compliance
Useful measurements
Flow rates
Volumes or capacities
 ). If the pressure difference is constant, a reduced flow rate indicates an increase in Raw. Because the radius of the airways normally lessens slightly during expiration, flow rates are usually measured during expiration. By rearranging the symbols in Poiseuille’s law (see Chapter 6), Raw is inversely related to the radius of the airways according to the following formula: Raw = ΔP/
). If the pressure difference is constant, a reduced flow rate indicates an increase in Raw. Because the radius of the airways normally lessens slightly during expiration, flow rates are usually measured during expiration. By rearranging the symbols in Poiseuille’s law (see Chapter 6), Raw is inversely related to the radius of the airways according to the following formula: Raw = ΔP/ = η8l/r4.
= η8l/r4.
Degree of Impairment
Obstruction based on FEV1
Restriction or Obstruction Based on TLC, FRC, RV
Gas Exchange Based on DLCO
Normal
80%-120%
80%-120%
80%-120%
Mild
70%-79%
70%-79% or 121%-130%
61%-79%
Moderate
60%-69%
60%-69% or 131%-140%
40%-60%
Moderately severe
50%-59%
50%-59% or 141%-150%
Severe
35%-49%
35%-49% or 151%-165%
<40%
Very severe
<35%
<35% or >165%
Infection Control
Equipment
 = ΔP ÷ R. Different manufacturers have used several materials to provide the resistance, including screens, capillary tubes, and fiber sheets made of silk, nylon, or filter paper. With multiple uses, condensation from exhaled air can collect in these devices and alter the resistance and accuracy of the device; some devices are heated to body temperature to prevent condensation. Known as thermistors or mass flowmeters, another type of flow-measuring device measures the temperature change created by gas flowing through it. There are also tubinometers, which use rotation of a fan or blades similar to a windmill. The number of rotations indicates volume, and the speed of the rotations indicates flow. How gas flow affects the transmission of sound waves and the force of flow stretching a spring have also been used to measure flow. Detailed descriptions and examples of each type of device are beyond the scope of this chapter and are available elsewhere.13
= ΔP ÷ R. Different manufacturers have used several materials to provide the resistance, including screens, capillary tubes, and fiber sheets made of silk, nylon, or filter paper. With multiple uses, condensation from exhaled air can collect in these devices and alter the resistance and accuracy of the device; some devices are heated to body temperature to prevent condensation. Known as thermistors or mass flowmeters, another type of flow-measuring device measures the temperature change created by gas flowing through it. There are also tubinometers, which use rotation of a fan or blades similar to a windmill. The number of rotations indicates volume, and the speed of the rotations indicates flow. How gas flow affects the transmission of sound waves and the force of flow stretching a spring have also been used to measure flow. Detailed descriptions and examples of each type of device are beyond the scope of this chapter and are available elsewhere.13
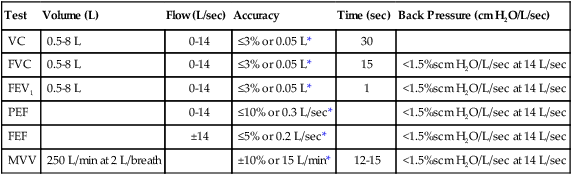
Test
Volume (L)
Flow (L/sec)
Accuracy
Time (sec)
Back Pressure (cm H2O/L/sec)
VC
0.5-8 L
0-14
≤3% or 0.05 L*
30
FVC
0.5-8 L
0-14
≤3% or 0.05 L*
15
<1.5%scm H2O/L/sec at 14 L/sec
FEV1
0.5-8 L
0-14
≤3% or 0.05 L*
1
<1.5%scm H2O/L/sec at 14 L/sec
PEF
0-14
≤10% or 0.3 L/sec*
<1.5%scm H2O/L/sec at 14 L/sec
FEF
±14
≤5% or 0.2 L/sec*
<1.5%scm H2O/L/sec at 14 L/sec
MVV
250 L/min at 2 L/breath
±10% or 15 L/min*
12-15
<1.5%scm H2O/L/sec at 14 L/sec
Principles of Measurement and Significance
Spirometry
 . A decrease in flow rate signifies an increase in airways resistance and the presence of airway obstruction when patient effort creating the difference between mouth pressure and lung pressure is constant (see Clinical Practice Guideline 19-1).17
. A decrease in flow rate signifies an increase in airways resistance and the presence of airway obstruction when patient effort creating the difference between mouth pressure and lung pressure is constant (see Clinical Practice Guideline 19-1).17
Forced Vital Capacity
Forced Expiratory Volume in 1 Second
Forced Expiratory Flow Between 200 ml and 1200 ml of Forced Vital Capacity and Forced Expiratory Flow Between 25% and 75% of Forced Vital Capacity
Peak Expiratory Flow
Maximal Voluntary Ventilation


 E)
E) ) decreases. Airway radius can be reduced by excessive contraction of the bronchial and bronchiolar muscles (bronchospasm), excessive secretions in the airways, swelling of the airway mucosa, airway tumors, collapse of the bronchioles, and other causes. By measuring flow rates, pulmonary function tests measure indirectly the size of the airways, Raw, and the presence of obstructive disease.
) decreases. Airway radius can be reduced by excessive contraction of the bronchial and bronchiolar muscles (bronchospasm), excessive secretions in the airways, swelling of the airway mucosa, airway tumors, collapse of the bronchioles, and other causes. By measuring flow rates, pulmonary function tests measure indirectly the size of the airways, Raw, and the presence of obstructive disease. ). Diagnostic spirometers usually measure and calculate vital capacity (VC), FVC, FEV1, peak expiratory flow (PEF) rate, and FEF rates. Some measure and calculate maximal voluntary ventilation (MVV). Some of these instruments may be a component of a laboratory system providing the volume-measuring or flow-measuring capability for other diagnostic tests of pulmonary function. For example, they may be used with gas analyzers to measure functional residual capacity (FRC) and total lung capacity (TLC) or the inspiratory VC during single-breath diffusing capacity (DLCOSB). Whether a spirometer or pneumotachometer is used in a diagnostic laboratory, a physician’s office, or at the bedside in an intensive care unit, it should meet or exceed the national performance standards for volume-measuring and flow-measuring devices.
). Diagnostic spirometers usually measure and calculate vital capacity (VC), FVC, FEV1, peak expiratory flow (PEF) rate, and FEF rates. Some measure and calculate maximal voluntary ventilation (MVV). Some of these instruments may be a component of a laboratory system providing the volume-measuring or flow-measuring capability for other diagnostic tests of pulmonary function. For example, they may be used with gas analyzers to measure functional residual capacity (FRC) and total lung capacity (TLC) or the inspiratory VC during single-breath diffusing capacity (DLCOSB). Whether a spirometer or pneumotachometer is used in a diagnostic laboratory, a physician’s office, or at the bedside in an intensive care unit, it should meet or exceed the national performance standards for volume-measuring and flow-measuring devices.