Pulmonary Function Test
Presentation
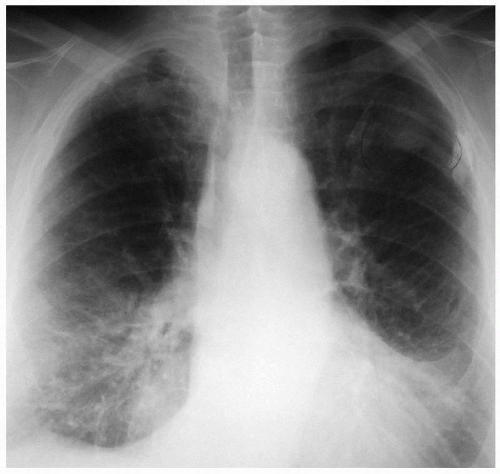
A 73-year-old man is referred to your office because of an incidental finding on a chest x-ray. The patient denies cough, fever, chills, weight loss, and appetite changes. He has a 50-pack-per-year smoking history and a past medical history of diabetes mellitus. On physical examination, there are diminished breath sounds at the bases of the lungs bilaterally. The following chest x-rays and computed tomography (CT) scan are obtained.
▪ Chest X-rays
Chest X-ray Report
The chest x-rays demonstrate a left upper lobe mass measuring 2.5 cm. There is bilateral apical and pleural thickening along the lateral aspect of the hemithoraces.
▪ CT Scan
CT Scan Report
The CT scan demonstrates a 2.7-cm × 3.2-cm mass in the peripheral portion of the left upper lobe. There are no other masses or infiltrates in the rest of the lung fields, and there are no pleural effusions. On additional images, there is no evidence of mediastinal adenopathy.
Discussion
The lung mass in a 73-year-old smoker is highly suspicious for malignancy. Sputum cytology, diagnostic fiberoptic bronchoscopy, fine-needle aspiration (FNA) of the mass under CT guidance, core needle biopsy under CT guidance, and excisional biopsy are modalities that enable the clinician to obtain tissue for diagnosis. Sputum cytology has a sensitivity of 20% to 70%; however, if the mass is peripheral, the yield for sputum cytology is small. The yield is higher when the tumor involves a main bronchus and when the patient presents with a productive cough or hemoptysis. Squamous cell cancer is more often diagnosed on sputum cytology than adenocarcinoma or small cell cancer. When sputum cytology identifies malignant cells, the specific cell type can be identified in 85% of the patients. Bronchoscopy has a high diagnostic yield if the tumor can be visualized in the endobronchial tree. Biopsy and brushings of a peripheral lesion yield a positive result in 25% of cases. Transthoracic FNA and core biopsy are applicable for peripheral lesions with a diagnostic accuracy of 80% to 95%. All of these diagnostic modalities are acceptable but do have a false-negative rate. For this reason, many surgeons would elect to perform an excisional biopsy either by video-assisted thoracoscopic surgery (VATS) or thoracotomy in order to obtain a proper tissue specimen for diagnosis. Achieving a diagnosis of cancer by less invasive means before thoracotomy allows for clinical staging and proper treatment planning such as preoperative chemoradiation in patients with positive (N2) lymph nodes on mediastinoscopy. Patients with negative needle biopsy may require surgical biopsy to verify that the mass is benign, if the clinical suspicion for cancer is high.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree