Chapter 24 Pulmonary Atresia with Intact Ventricular Septum
Thomas Peacock,1 in his first edition of Malformations of the Human Heart, wrote:
“… the orifice or trunk of the pulmonary artery is entirely impervious. A case of this description was described by John Hunter in 1783.2 The child was born at the eighth month, was very livid … and died in convulsions on the thirteenth day. The pulmonary artery was found entirely impervious. The septum of the ventricles was entire, and the right ventricle had scarcely any cavity left, while the left ventricle was large and powerful. The foramen ovale continued open, and the pulmonary branches received their supply of blood from the aorta, through the medium of the arterial duct.”
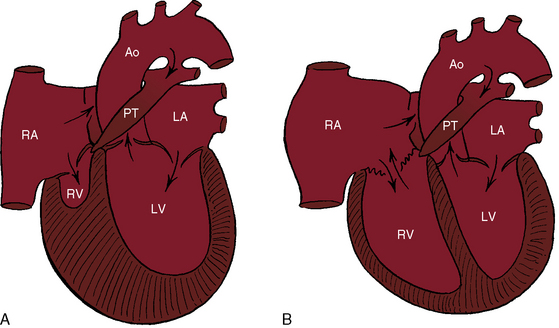
Peacock referred to what is now called pulmonary atresia with intact ventricular septum, a malformation in which an imperforate pulmonary valve completely obstructs forward flow into the pulmonary trunk (Figure 24-1). The ventricular septum is, by definition, intact, and a restrictive interatrial communication is the only exit from the right atrium. The imperforate pulmonary valve consists of three fused but well-formed cusps with triradiate commissural ridges that converge at the center of a sealed orifice that is structurally similar, if not identical, to pinpoint pulmonary valve stenosis (see Chapter 11).3 Less commonly, commissural ridges are confined to the periphery of the valve, which has an imperforate dimple at the center.3 The atresia is valvular (i.e., membranous) in 75% of cases and muscular (i.e., infundibular) in the remainder.4,5 Muscular obliteration within the right ventricle results in a “unipartite, bipartite, or tripartite” ventricular chamber with an obliterated apex.4,5
The reported incidence rate of pulmonary atresia with intact ventricular septum is 1 per 22,000 live births6 to 4.2 per 100,000 live births.5,7 A well-developed pulmonary trunk (see Figure 24-1) implies that forward flow once occurred across a pulmonary valve that was stenotic but patent during much, if not most, of fetal life. A normally formed ductus arteriosus implies that intrauterine blood flow was from the right ventricle into the pulmonary trunk through the ductus and into the aorta (see Figure 24-5), in contrast to Fallot’s tetralogy with pulmonary atresia in which a long tortuous ductus functions in utero as a systemic artery that carries blood from the aorta into the pulmonary artery (see Chapter 18).
The normal right ventricle consists of an inlet portion that is part of the diastolic filling mechanism and a trabecular and an infundibular portion that are parts of the systolic pump mechanism. More than three quarters of cases of pulmonary atresia with intact ventricular septum are characterized by a small thick-walled right ventricle (Figures 24-1A and 24-2A, B) that is equipped with all three of these morphologic portions (see Figures 24-1A and 24-2A, B),8,9 together with fiber disarray, capillary disorganization, and endocardial fibroelastosis.10,11 Pinpoint pulmonary valve stenosis in the neonate occasionally exists with a diminutive right ventricular cavity analogous to pulmonary atresia with intact ventricular septum.
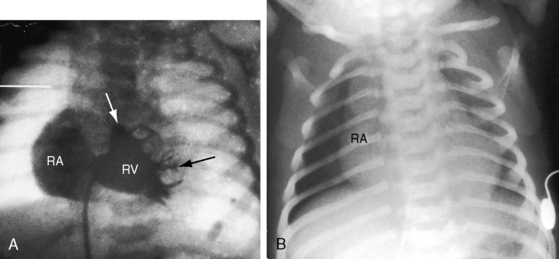
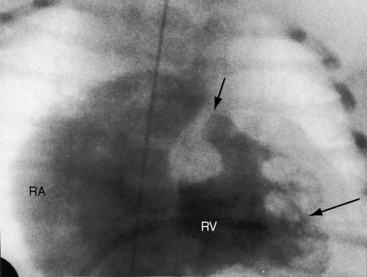
When the right ventricle is small and thick-walled, the tricuspid annulus is also small and houses a small, thickened valve with poorly delineated chordal attachments and hypoplastic papillary muscles. When the right ventricle is dilated and thin-walled, the tricuspid valve is incompetent and either resembles Ebstein’s malformation or is dysplastic with normally attached tricuspid leaflets. Functional pulmonary atresia has been applied when a dilated mechanically inadequate right ventricle with tricuspid regurgitation cannot generate sufficient systolic pressure to open a stenotic but nonatretic pulmonary valve.12 Functional pulmonary atresia also occurs during transient neonatal tricuspid regurgitation.13 In a small subset of patients with florid tricuspid regurgitation, the right ventricle and right atrium are enormous—“wall-to-wall hearts” (see section X-Ray).14 Rarely, a suprasystemic right ventricle causes leftward displacement of the ventricular septum and obstruction to left ventricular outflow.15,16
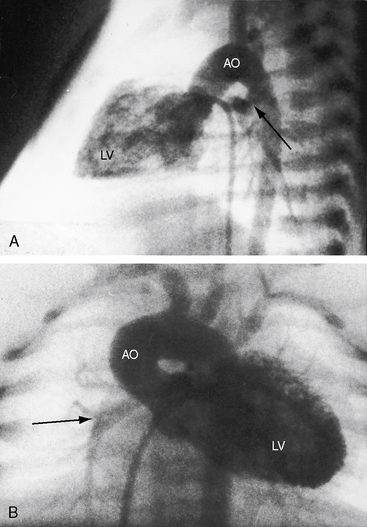
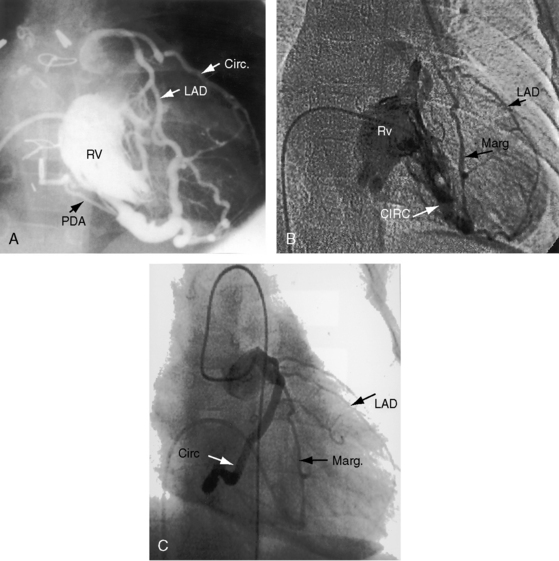
The coronary circulation in pulmonary atresia with intact ventricular septum and small right ventricle has long been the focus of lively interest.11,17–24 Intramyocardial sinusoids were described in 192625 and play important roles in the pathogenesis of right ventricular-to-coronary artery communications (see Figure 24-2).17,18 Morphogenetic studies have shed new light on coronary vascular bed abnormalities in this malformation (see Chapter 32).19,26 The normal coronary circulation develops in an orderly sequence of blood islands, coronary venous connections, and coronary artery-to-aortic connections. The blood islands proliferate and coalesce to form networks of vascular channels that have no connection with other blood islands or with the ventricular cavity. Suprasystemic systolic pressure from the small isovolumetrically contracting right ventricle drives blood through primitive vascular channels that are composed of thickened intima and fibroelastic walls19 and that connect the right ventricular cavity to epicardial coronary arteries (see Figure 24-2A, B).18,19 Abnormalities of the coronary vascular bed occur in 50% of patients with pulmonary atresia, intact ventricular septum, and a small right ventricle and are either secondary to the hemodynamic derangements of the malformation or are coexisting morphologic abnormalities,18,23 such as ostial atresia24,27or fibromuscular dysplasia with focal luminal narrowing.17 Myocardial sinusoids are rarely primary developmental faults.28 Epicardial veins may be prominent and thick-walled.19 Ventriculocoronary arterial connections are located chiefly in the region of the apex of right ventricle and communicate chiefly with the distal left anterior descending coronary arterial system (see Figure 24-2A, B).19 Intramyocardial channels that end blindly punctuate the endocardium of the thick-walled right ventricle, creating the appearance of a highly trabeculated muscular wall (Figures 24-3 and 24-4).19
Ventriculocoronary arterial communications have been found in the inverted left ventricle of congenitally corrected transposition of the great arteries with pulmonary atresia and intact ventricular septum.29,30 Left ventricular–to–coronary arterial connections in aortic atresia with intact ventricular septum differ from right ventricular–to–coronary arterial connections in pulmonary atresia with intact ventricular septum (see Chapters 31 and 32).19,31,32
Myocardial ischemia is an important sequel of ventriculocoronary arterial connections.18,19 Large unobstructed connections (see Figure 24-2A, C) function as a fistulous steal because blood from the aortic root flows freely into the right ventricular cavity during diastole. More commonly and more importantly, ischemia and occasionally myocardial infarction result from obstructing luminal abnormalities that range from mild medial and intimal thickening to luminal obliteration and that extend from the origins of the intramyocardial connections to the coronary artery ostia in the aortic sinuses.17–19 Luminal obstructive lesions that originate in the fetus and neonate can evolve into severe stenoses or obliteration.18,19 Proximal discontinuity of a coronary artery is the most egregious form of this prejudicial coronary circulation and is the result of acquired ostial obliteration or congenital atresia of an aortic sinus ostium. Left ventricular aneurysm9 and right ventricular rupture33,34 are consequences of myocardial ischemia and infarction that are largely responsible for the high mortality rate.18 Proximal discontinuity and luminal obstruction set the stage for a right ventricular–dependent coronary circulation in which suprasystemic systolic pressure is required to generate retrograde coronary blood flow on which myocardial perfusion depends.33 The right atrium enlarges only moderately when the right ventricle is diminutive, but when the right ventricle is dilated and tricuspid regurgitation is severe, the right atrium can be aneurysmal (see Figure 24-4). The left atrium enlarges because it receives venous return from both the systemic and the pulmonary circulations. The left ventricle is initially large and powerful as Peacock1 described (Figure 24-5), but its compliance and ejection fraction diminish because it pumps the entire output for both circulations.35 The course of the atrioventricular conduction system is normal.36
The physiologic derangements in pulmonary atresia with intact ventricular septum are implicit consequences of the anatomic features of the malformation. Physiologic classification is based on the tripartite morphology of the right ventricle and on whether the right ventricular hypoplasia is mild, moderate, or severe. Venous blood reaches the systemic circulation via an interatrial communication that is usually a restrictive patent foramen ovale, which is the only exit from the right atrium (see Figure 24-1; see previous). Unoxygenated right atrial blood mixes with oxygenated left atrial blood and flows into the left ventricle and into the aorta, so systemic arterial oxygen saturation is reduced. Blood from the aorta reaches the pulmonary circulation through a tenuously patent ductus arteriosus on which survival depends (see Figures 24-1 and 24-5).37 When the ductus closes, effective pulmonary blood flow ceases.37 Systemic-to-pulmonary collaterals are inadequate for survival.37
These physiologic pathways from the right atrium to the left side of the heart are relatively constant from patient to patient, but the patterns in the right side of the heart vary considerably. When the right ventricle is small, little blood enters or leaves its cavity because the diminutive chamber and the diminutive tricuspid valve obstruct right atrial flow, which is further compromised by a thick ventricular wall and endocardial fibroelastosis. Whatever blood enters the right ventricle during diastole is trapped during systole, except for the small portion that exits through ventriculocoronary arterial connections. When the right ventricle is dilated and thin-walled, and the tricuspid valve is incompetent, right atrial blood copiously enters the ventricular cavity during diastole, only to be returned to the right atrium during the next systole. Systolic pressure is comparatively low when the right ventricle and right atrium communicate freely across an incompetent tricuspid valve. Although right atrial blood readily flows into the right ventricle, no useful purpose is served because forward flow into the pulmonary trunk is impossible. Back-and-forth movement of blood across the tricuspid orifice results in progressive enlargement of the right side of the heart, which becomes massive (see previous).14
History
Pulmonary atresia with intact ventricular septum is equally prevalent in males and females.38 Reports exist of the malformation in siblings,39,40 in first cousins,41 and in monozygotic twins,42 but familial recurrence is rare. More than half of newborns die in the first month of life, a considerable majority die within the first 3 months, and very few live beyond the first year. Survival hinges on tenuous patency of the ductus arteriosus and on the adequacy of the interatrial communication, which is usually restrictive.37 Cyanosis begins immediately after birth, and the degree depends on patency of the ductus arteriosus.37 Pulmonary blood flow diminishes as the ductus involutes, and when the ductus closes, pulmonary blood flow ceases. Despite this ominous outlook, isolated examples of survival have been reported to age 3.5 years43 and 14 years,44 and four patients lived for 20 to 21 years.45–48 The 21-year-old patient had a closed ductus arteriosus at necropsy and had instead a sizable connection between the aortic root and pulmonary trunk and a large atrial septal defect.48 Another 21-year-old woman survived without a patent ductus because the anterior descending branch of the left coronary artery originated from the pulmonary trunk and provided pulmonary blood flow via intercoronary anastomoses.49