Pulmonary Artery Sarcoma
Presentation
A 71-year-old woman presents to your office with complaints of a chronic dry cough. She has no significant past medical history. She walks every day for 30 minutes without symptoms of shortness of breath. She denies productive sputum, hemoptysis, weight loss, fever, chills, or night sweats. She is a lifetime nonsmoker and has not recently traveled outside the United States. She has an iodine allergy.
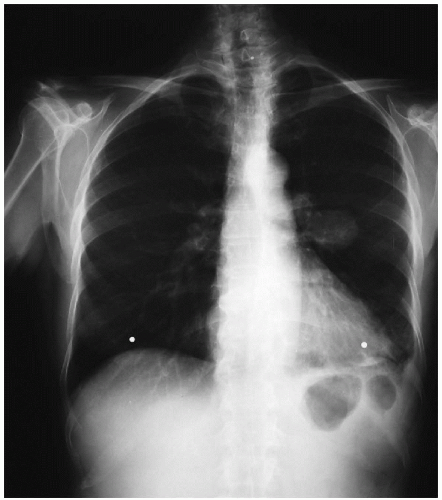
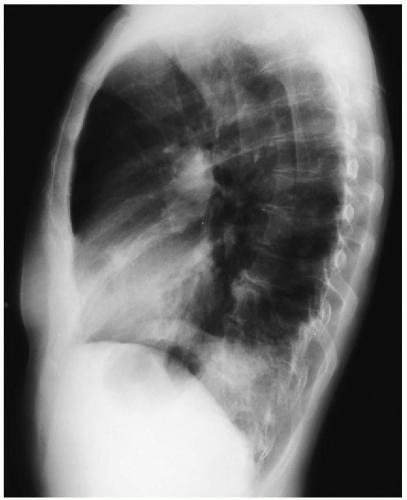
▪ Chest X-rays
Chest X-ray Report
The trachea is midline. The heart size is normal. There is a small pleural effusion in the left chest. There is a round, smooth-edged, well-circumscribed mass located in the left mid-lung field. There is a clear line of demarcation between the border of the heart and the mass. ▪
Differential Diagnosis
Although this patient is a nonsmoker and only about 5% of patients with lung cancer are nonsmokers, the diagnosis of lung cancer should be considered. Passive smoking accounts for 25% of lung cancer in nonsmokers. Moreover, the risk for lung cancer increases 35% to 53% in nonsmokers who live with smokers. Because the anatomic location of the mass is central, other diagnoses that should be considered include mesodermal tumors such as angiosarcoma and hemangioma, arteriovenous fistulas, metastatic disease, and pulmonary artery aneurysms. Finally, hamartomas should also be included in the differential diagnosis. These tumors can appear round or lobulated but have a smooth border. Hamartomas are often calcified, and the finding of “popcorn” calcifications on chest x-rays is suggestive of this diagnosis.
Discussion
Further anatomic delineation of the mass in addition to evaluation of mediastinal structures is important in achieving a diagnosis and planning a therapeutic approach. For these reasons, a computed tomography (CT) scan of the chest and bronchoscopy is necessary. Aspiration of the left pleural effusion through a thoracentesis may also yield a diagnosis. Cytology from a pleural effusion yields a diagnosis of malignancy in 20% to 60% of patients with cancer. A positron-emission tomography (PET) scan may be considered, but it is more commonly used to assess metastases instead of diagnosing the primary lesion.
Recommendation
CT scan of the chest, bronchoscopy, and thoracentesis are recommended.
Case Continued
The bronchoscopy reveals no evidence of intrabronchial lesions or extraluminal compression. The bronchial mucosa in the left upper lobe bronchus appears hyperemic. Biopsies demonstrate macrophages and chronic inflammatory cells, but no neoplastic cells. A thoracentesis is performed at the time of bronchoscopy, and 100 mL of clear fluid is aspirated and reveals no malignant cells on cytologic examination.