Inappropriate shock is a frequently seen clinical problem despite advanced technologies used in modern implantable cardioverter-defibrillator (ICD) devices. Our aim was to investigate whether simply raising the ICD detection zones can decrease inappropriate therapies while still providing appropriate therapy. We randomized 223 patients with primary prevention to either the conventional programming group with 3 zones as VT 1 (167 to 182 beats/min) with discriminators, VT 2 (182 to 200 beats/min) with discriminators, and ventricular fibrillation (>200 beats/min) (n = 100) or the high-zone programming group with 3 zones as VT 1 (171 to 200 beats/min) with discriminators, VT 2 (200 to 230 beats/min) with discriminators, and ventricular fibrillation (>230 beats/min; n = 101). Twenty-two patients were lost to follow-up. The primary objectives were the first episode of appropriate and inappropriate therapies. The secondary objectives were all-cause mortality and hospitalization for heart failure. During 12-month follow-up, the first episode of appropriate therapy was higher (22% vs 10%, hazard ratio [HR] 2.18, 95% confidence interval [CI], 1.09 to 4.36, p = 0.028) and the first episode of inappropriate therapy was lower (5% vs 28%, HR 0.18 [95% CI 0.07 to 0.44], p <0.001) in the high-zone group compared with the conventional group. Although all-cause mortality did not differ (2% for the high-zone group vs 3% for the conventional group, HR 0.65 [95% CI 0.11 to 3.99], p >0.05), hospitalization for heart failure was significantly higher in the conventional group (13% vs 4%, HR 0.28 [95% CI 0.09 to 0.88], p = 0.021). In conclusion, in a real-world population, high-zone settings of the single-, dual-, and triple-chamber ICDs were associated with reduction in inappropriate therapy while still providing appropriate therapy.
The efficacy of the implantable cardioverter-defibrillator (ICD), either alone or in combination with the cardiac resynchronization therapy (CRT), to reduce the mortality in heart failure has been shown in several studies. Therefore, the current European and American device guidelines recommend that high-risk patients with heart failure receive an ICD for primary prevention. However, a significant amount of these patients receive inappropriate or unnecessary ICD therapies for nonventricular and nonsustained ventricular tachyarrhythmia including ventricular tachycardia (VT) and ventricular fibrillation (VF) despite technologically well-designed detection algorithms to differentiate ventricular from nonventricular arrhythmia. Inappropriate shocks cause impaired quality of life, psychiatric disturbances, and, moreover, increased mortality. Although various studies have been designed to reduce inappropriate shocks, the best method for programming to reduce inappropriate therapies is unknown. The modification of the detection zone settings was evaluated in the Multicenter Automatic Defibrillator Implantation Trial–Reduce Inappropriate Therapy (MADIT-RIT) study. However, this trial included only patients with sinus rhythm, receiving a dual- or triple-chamber ICD. There was a significant reduction in the first occurrence of inappropriate therapy, either antitachycardia pacing (ATP) or shock. Therefore, we conducted a single-center, prospective, randomized the Reduction of Inappropriate Shocks by Increased Zones (RISSY-ICD) study to show that a simple ICD programming would be able to reduce the number of inappropriate therapies while still providing appropriate therapy in all patients with heart failure who received an ICD for primary prevention.
Methods
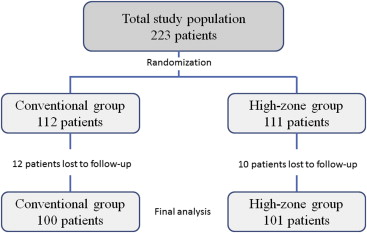
The RISSY-ICD study was designed to evaluate whether the higher rate detection zones in patients with primary prevention would reduce the incidence of inappropriate ICD therapies. This prospective, single-center, randomized, controlled study included patients with single-, dual-, and triple-chamber ICDs in both sinus rhythm and atrial fibrillation (AF). The patients were enrolled from January 2012 to December 2012. The study included 223 patients from a tertiary center hospital ( Yuksek Ihtisas Heart-Education and Research Hospital ) in Turkey. Study patients were followed for 12 months. Twenty-two patients were lost to follow-up during the study period, and the data for the remaining 201 patients were analyzed ( Figure 1 ). The study protocol was approved by the institutional ethical committee. All patients provided written informed consent before randomization. There was no financial or any other support for the trial. The design of the study was registered previously ( ClinicalTrials.gov number, NCT02044315 ).
Patients with the age ≥18 years were included if they had ischemic or nonischemic heart failure and met approved guidelines for primary prevention for either an ICD or a Cardiac Resynchronization Therapy-Defibrillator (CRT-D). Patients were excluded if they had previously implanted pacemaker/ICD/CRT-D, underwent coronary revascularization, or had an enzyme-positive myocardial infarction within 3 months before the enrollment, history of hemodynamically relevant ventricular tachyarrhythmia, primary electrical disease, pregnancy, major psychological disease, <1 year of life expectancy, inability to provide written informed consent, and unwilling to participate in the study.
Patients were followed before hospital discharge and at 3-month intervals until the termination of the study. At baseline, all patients underwent clinical evaluation, estimation of the NYHA functional class, and left ventricular ejection fraction. Patients received optimal medical therapy according to the current practice guidelines, and antiarrhythmic drug use was recorded. At each follow-up visit, the device was interrogated, and adverse events and changes in medication were noted. AF was defined as the long-standing persistent AF as the only conducted rhythm.
Patients were randomized in equal numbers to either a conventional ICD programming (conventional group) or an ICD programming with high detection zones (high-zone group) using permuted block randomization. All study participants were blinded for the allocated intervention.
In the present study, a single type of ICD from a single manufacturer was used (D384VRG Cardia VR, D384DRG Cardia DR, and D384TRG Cardia CRT-D; Medtronic Inc, Minneapolis, MN). All patients were programmed according to a standardized protocol with 3 detection zones: a slower detection zone for VT (VT 1 zone; VT label in Cardia ICDs) and 2 faster detection zones for fast VT (VT 2 zone; fast VT (FVT) label in Cardia ICDs) and VF (VF zone; VF label in Cardia ICDs). Both the conventional and the high-zone groups had 3 zones as VT 1 , VT 2 , and VF. In addition, the monitor zone was set to 133 beats/min with the number of intervals detected of 40. In all ICDs, ATP was followed by biphasic shock if pacing did not terminate the tachyarrhythmia. For discriminating VT from supraventricular tachyarrhythmia (SVT), all discriminators were activated. The programmed parameters were summarized in Table 1 . Detailed descriptions of ATP/shock features and SVT-VT discriminators are available in the Supplementary Materials .
| Programmed parameters | Conventional group | High-zone group |
|---|---|---|
| Detection | ||
| VT 1 zone (bpm) | 167-182 | 171-200 |
| NID, initial | 32 | 32 |
| NID, redetection | 12 | 12 |
| VT 2 zone (bpm) | 182-200 | 200-230 |
| NID, initial | 30/40 | 30/40 |
| NID, redetection | 12/16 | 12/16 |
| VF zone (bpm) | >200 | >230 |
| NID, initial | 30/40 | 30/40 |
| NID, redetection | 12/16 | 12/16 |
| Monitor zone (bpm) | 133-167 | 133-171 |
| NID, initial | 40 | 40 |
| Supraventricular tachycardia discriminators | ||
| Single-chamber ICDs | ||
| Wavelet | ON | ON |
| Onset | ON | ON |
| Stability | ON | ON |
| Dual-/Triple-chamber ICDs | ||
| PR logic | ON | ON |
| Onset | ON | ON |
| Stability | ON | ON |
| Therapy | ||
| VT 1 zone | ATP x 6, then shock | ATP x 6, then shock |
| VT 2 zone | ATP x 4, then shock | ATP x 4, then shock |
| VF zone | ATP during charging and shock | ATP during charging and shock |
| Monitor zone | None | None |
The primary end point of this study was the first occurrence of inappropriate therapy with either ATP or shock. The investigators could change the device programming after the first occurrence of inappropriate therapy. Arrhythmia episodes were classified as sustained VT/VF, SVT, oversensing, and AF. Appropriate ICD therapy was defined as sustained VT/VF treated by ATP and/or shock within the respective detection zone. Inappropriate therapy was defined as ATP and/or shock for nonventricular tachyarrhythmia or because of oversensing. The other primary end point was the first occurrence of appropriate ICD therapy with either ATP or shock. Inappropriate event episodes were classified as SVT, oversensing, and AF. The number and cycle length of all tachycardia episodes were documented. Predefined 2 secondary end points were all-cause mortality and hospitalization for heart failure.
Two independent electrophysiologists blinded to study design performed ICD interrogations, reviewed, and classified the arrhythmia episodes. When no consensus was reached, a third physician was included, and the final judgment was based on the majority decision. All device interrogations were performed in a core laboratory, specifically equipped with pacemaker and ICD analyzers.
Analyses were performed using SPSS Statistics, version 17.0 (SPSS Inc., Chicago, Illinois). To test the distribution pattern, the Kolmogorov-Smirnov method was used. Data were summarized as the mean ± SD, median and interquartile range, or proportion as appropriate. The Student’s t test was used to compare the data between the groups displaying normal distribution. The Mann-Whitney U test was applied to compare the data without normal distribution. Categorical variables were compared with the chi-square or Fisher’s exact test. Cox proportional hazard regression model was used to estimate the risk of a first occurrence of inappropriate and appropriate therapies. The survival curve during follow-up for inappropriate and appropriate therapies was analyzed using the Kaplan-Meier method, and the statistical assessment was performed using the log-rank test. A p value <0.05 was considered to be statistically significant for all analyses.
Using hazard ratio for total first inappropriate therapy of 0.18 with the high-zone programming, compared with the conventional programming, representing a total of 33 events in the 2 groups, 99% power was achieved with a 2-tailed α of 0.05.
Results
The clinical characteristics of the 201 randomized patients are listed in Table 2 . Baseline characteristics, including antiarrhythmic use and device type, were similar in both groups. The majority of study population were men (85.1%). Ischemic origin was 73.6%, and 26.4% had AF. The ICDs were implanted alone in 83.1% of patients, in combination with CRT in 16.9% of the entire population. All patients were followed for 12 months. There was a total of 5 all-cause mortality in the study population during the follow-up period. In addition, the overall number of syncope events was very low in the total study population during the follow-up: 2 syncopes were observed in the high-zone group, whereas 1 episode occurred in the conventional group (based on device diagnostics, all because of fast VT acceleration after ATP; 2.0% vs 1.0%, p = 0.574).
| Characteristics | Conventional group (n = 100) | High-zone group (n = 101) | P |
|---|---|---|---|
| Men | 84 | 87 | 0.671 |
| Age (years) | 57.0 ± 12.4 | 57.2 ± 11.9 | 0.908 |
| Heart failure etiology | 0.749 | ||
| Ischemic | 75 | 73 | |
| Non-ischemic | 25 | 28 | |
| Hypertension | 50 | 53 | 0.726 |
| Diabetes mellitus | 22 | 19 | 0.603 |
| Smoker | 7 | 10 | 0.613 |
| Atrial fibrillation | 30 | 23 | 0.245 |
| NYHA class | 0.713 | ||
| Class I | 27 | 28 | |
| Class II | 56 | 54 | |
| Class III | 15 | 14 | |
| Class IV | 2 | 5 | |
| Systolic blood pressure (mmHg) | 110 (100 – 120) | 110 (110 – 120) | 0.106 |
| Diastolic blood pressure (mmHg) | 80 (70 – 85) | 80 (70 – 80) | 0.599 |
| Heart rate (bpm) | 70 (65 – 80) | 75 (65 – 80) | 0.278 |
| Left ventricular ejection fraction (%) | 25 (25 – 30) | 25 (24 – 29) | 0.139 |
| Device type | 0.735 | ||
| Single-chamber ICD | 61 | 65 | |
| Dual-chamber ICD | 20 | 21 | |
| Cardiac resynchronization therapy ICD | 19 | 15 | |
| Pacemaker dependent | 20 | 23 | 0.731 |
| Medications | |||
| ACE-I/ARB | 94 | 95 | 0.986 |
| Spironolactone | 51 | 48 | 0.673 |
| Aspirin | 74 | 70 | 0.532 |
| Digoxin | 32 | 36 | 0.655 |
| Diuretic | 71 | 74 | 0.755 |
| Statin | 36 | 34 | 0.768 |
| β-blocker | 94 | 97 | 0.537 |
| Mexiletine | 1 | 2 | 0.567 |
| Amiodarone | 9 | 14 | 0.279 |
The number of patients with a first occurrence of appropriate or inappropriate therapy, with any occurrence of device-delivered therapy, and the total occurrences of appropriate and inappropriate therapies, according to randomization group and the type of therapy (ATP or shock), showed that the high-zone group had significantly less patients with a first occurrence of inappropriate therapy (ATP or shock) compared with the conventional group, driven by the reduction in both first inappropriate shock and ATP. The first occurrence of inappropriate shock was most frequent with atrial flutter/fibrillation (72.7%), regular SVT (24.2%), and oversensing (3.0%) ( Table 3 ). Specifically, SVT including irregular and regular heart rates causing inappropriate device therapies were more frequent in the conventional group compared with the high-zone group. High-zone programming also resulted in a higher incidence of appropriate therapy. Accordingly, the increment was driven by the higher number of patients with detected VT episodes treated by ATP, whereas the number of patients with an appropriate shock remained similar. Moreover, neither total shock nor total ATP was different between the 2 groups ( Table 4 ).
| Event type | Conventional group (n = 100) | High-zone group (n = 101) | P |
|---|---|---|---|
| Atrial fibrillation/flutter | 20 | 4 | <0.001 |
| Supraventricular tachycardia | 7 | 1 | 0.035 |
| Oversensing | 1 | 0 | 0.498 |
| Variable | Conventional group (n = 100) | High-zone group (n = 101) | HR (95% CI) | P |
|---|---|---|---|---|
| First inappropriate shock | 10 | 2 | 0.20 (0.04-0.88) | 0.034 |
| First inappropriate ATP | 18 | 3 | 0.17 (0.05-0.54) | 0.003 |
| Total first inappropriate therapy | 28 | 5 | 0.18 (0.07-0.44) | <0.001 |
| First appropriate shock | 5 | 8 | 1.58 (0.54-4.68) | 0.405 |
| First appropriate ATP | 5 | 14 | 2.77 (1.04-7.41) | 0.042 |
| Total first appropriate therapy | 10 | 22 | 2.18 (1.09-4.36) | 0.028 |
| Total first shock | 15 | 10 | 0.66 (0.31-1.40) | 0.278 |
| Total first ATP | 23 | 17 | 0.73 (0.42-1.28) | 0.277 |
| Total first therapy | 38 | 27 | 0.70 (0.47-1.06) | 0.092 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


