Cardiovascular (CV) diseases and chronic kidney disease (CKD) have common predisposing factors that subsequently cause microvascular dysfunction. In the absence of obstructive coronary artery disease, coronary flow reserve (CFR) represents the status of coronary microcirculation. This study aimed to investigate the prognostic importance of impaired CFR, as a marker of microvascular dysfunction, on long-term CV outcomes in patients with CKD. This study consisted of 139 patients with an estimated glomerular filtration rate of <60 ml/min/1.73 m 2 who had no obstructive narrowing of the left anterior descending artery. Transthoracic Doppler echocardiography was used to measure CFR in the left anterior descending artery. During the follow-up period (3.3 ± 1.6 years), CV events occurred in 26 patients (18.7%). Multivariate analysis that included CFR as a continuous value identified a serum level of C-reactive protein (hazard ratio 1.41, p = 0.03) and a value of CFR (hazard ratio 0.21, p = 0.009) as determinants for CV events, independent of traditional CV risk factors. Patients with a CFR of <2.0 had worse CV outcomes compared with those with a CFR of ≥2.0 (p <0.001). In conclusion, transthoracic Doppler echocardiographically derived CFR was useful for the risk stratification of CV outcomes in patients with CKD. The presence of microvascular dysfunction may play an important role in the association between CKD and future CV events.
The presence of chronic kidney disease (CKD) is strongly associated with an increased risk of cardiovascular (CV) events and total mortality, independent of traditional CV risk factors. Patients with CKD are more likely to die from a CV event, rather than renal failure itself, and risk stratification for predicting future CV events is a key issue for patients with CKD, even at early stages. Coronary microcirculation is deteriorated by traditional CV risk factors and their co-morbid conditions such as endothelial dysfunction and chronic inflammation, which play a central role in the association between CKD and CV diseases. We therefore hypothesized that the assessment of coronary flow reserve (CFR) predicts long-term CV events in patients with CKD, as a marker of microvascular function. This study therefore aimed to investigate whether CFR measurement by transthoracic Doppler echocardiography (TTDE) predicts long-term CV outcomes in patients with CKD.
Methods
This study consisted of 139 patients (85 men, mean age 73 ± 11 years) with an estimated glomerular filtration rate (eGFR) of <60 ml/min/1.73 m 2 and/or the presence of microalbuminuria who underwent TTDE examination. The indication for CFR measurement was suspected coronary artery disease (CAD) in 75 subjects (54%) and risk stratification of known CAD in 64 subjects (46%). Patients with obstructive narrowing (≥50%) of the left anterior descending artery (LAD) on invasive coronary angiography were excluded. Other exclusion criteria were (1) a history of myocardial infarction, (2) a history of coronary revascularization in the LAD, (3) more than moderate valve disease, (4) dilated or hypertrophic cardiomyopathy, (5) hemodialysis, (6) peritoneal dialysis, and (7) a history of a kidney transplant. This study was approved by the ethics committee of the Osaka Ekisaikai Hospital and Higashisumiyoshi Morimoto Hospital.
The presence or absence of the following CV risk factors was evaluated on the basis of data retrieved from the medical records: hypercholesterolemia (serum total cholesterol level ≥200 mg/dl or statin treatment), diabetes (fasting plasma glucose level >126 mg/dl, taking hypoglycemic drugs or insulin, or a combination of the two), smoking, and obesity (body mass index ≥30 kg/m 2 ) in each patient.
Following baseline biophysical and laboratory parameters were assessed at CFR examination: body weight, body mass index, hemoglobin, glucose, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, C-reactive protein (CRP), and creatinine. eGFR was calculated using the Modification of Diet in Renal Disease (MDRD) study equation.
All patients were followed up in the hospital or with a clinic visit every month. The end points of this analysis were all-cause deaths including cardiac, cerebral, vascular, and other deaths and cardiac, cerebral, and vascular events. Cardiac events were defined as fatal and nonfatal myocardial infarction, unstable angina pectoris, congestive heart failure, coronary bypass graft surgery, resuscitated cardiac arrest, and cardiopulmonary arrest on arrival. Angiographic restenosis incidentally found on routine follow-up coronary angiography without clinical symptoms was excluded from the events registration. Cerebral events included cerebral hemorrhage, cerebral infarction, and transient ischemic attack. Aortic dissection and rupture of an aortic aneurysm were classified as vascular events.
Echocardiographic examinations were performed with a Vivid 7 echocardiography device (General Electric, Milwaukee, Wisconsin) or a Sequoia 512 (Siemens Medical Solution Inc., Mountain View, California). A modified foreshortened 2-chamber view was applied to explore the flow in the distal portion of the LAD. If the angle between color flow and the Doppler beam was >20%, angle correction was performed. Coronary blood flow velocity was obtained at baseline and after intravenous infusion of adenosine triphosphate at a rate of 0.14 mg/kg/min for 2 minutes to produce hyperemia. Mean diastolic flow velocity was measured by tracing the contour of the spectral Doppler signal. CFR was calculated as the ratio of hyperemic to basal flow velocity. For each variable in the CFR measurements, the values of 3 cycles were averaged.
The dimensions of the cardiac chambers were measured in the standard manner. Left ventricular ejection fraction was obtained using the Simpson’s methods from the apical 4- and 2-chamber views. Left ventricular mass was calculated based on the area-length formula. Pulsed-wave Doppler examination of mitral inflow was performed to measure peak velocity (E) and deceleration time of the early diastolic flow. Early diastolic mitral annular velocity (e′) was also measured from tissue Doppler imaging in the septal wall. The ratio of E to e′ was then calculated (E/e′). TTDE examination was performed by 2 expert sonographers who had >5 years of experience in echocardiography with approximately 100 CFR examinations. They were blinded to all clinical information.
Categorical variables are presented as frequencies and continuous variables as mean ± SD. The chi-square test was used for comparison of categorical variables. Between-group comparisons were made using the independent-samples t test or Mann-Whitney U test, as appropriate. Cox proportional hazard analysis was performed to identify predictors of CV events. Baseline variables that were considered clinically relevant or that showed a univariate relation with outcomes were entered into the analysis. The Kaplan-Meier survival method was used to compare survival according to the value of CFR, using the log-rank test. Differences were considered significant at p <0.05.
Results
CFR examinations were adequately performed in all subjects. The baseline clinical characteristics are listed in Table 1 . Of the 139 patients, 107 (77%) had reduced eGFR with microalbuminuria, 18 (13%) had reduced eGFR without microalbuminuria, and 14 (10%) had microalbuminuria preserving eGFR. The cause of renal dysfunction was diabetes in 41 patients (29%), hypertension in 35 (26%), glomerular disease in 22 (16%), and other causes in 41 (29%), such as polycystic kidney disease, gouty kidney, and amyroid kidney.
| Variables | All Patients (n = 139) | Event (+) (n = 26) | Event (−) (n = 113) | p |
|---|---|---|---|---|
| Age (yrs) | 73 ± 10 | 75 ± 9 | 73 ± 11 | 0.3 |
| Men | 85 (61) | 12 (46) | 73 (64) | 0.08 |
| Hypertension | 108 (78) | 20 (77) | 88 (78) | 0.9 |
| Diabetes mellitus | 41 (29) | 8 (33) | 33 (29) | 0.8 |
| Hypercholesterolemia | 65 (47) | 11 (42) | 54 (48) | 0.6 |
| Smoker | 46 (33) | 7 (27) | 39 (35) | 0.5 |
| Obesity | 5 (4) | 2 (8) | 3 (3) | 0.2 |
| Coronary narrowing | ||||
| Right | 24 (17) | 4 (17) | 20 (18) | 0.8 |
| Left circumflex | 36 (26) | 8 (31) | 28 (24) | 0.5 |
| Medications | ||||
| ACEI or ARB | 68 (49) | 15 (58) | 53 (47) | 0.3 |
| Calcium channel blocker | 52 (37) | 8 (31) | 44 (39) | 0.4 |
| Statin | 41 (29) | 6 (23) | 35 (31) | 0.4 |
| CRP (mg/L) | 2.0 ± 1.6 | 2.8 ± 1.6 | 1.8 ± 1.6 | 0.006 |
| eGFR (ml/min/1.73 m 2 ) | 46 ± 12 | 38 ± 15 | 47 ± 11 | <0.001 |
| Microalbuminuria | 121 (87) | 25 (96) | 96 (85) | 0.1 |
| Echocardiographic parameters | ||||
| Left ventricular ejection fraction (%) | 56 ± 11 | 53 ± 11 | 57 ± 11 | 0.09 |
| Left ventricular mass index (g/m 2 ) | 115 ± 34 | 128 ± 44 | 111 ± 31 | 0.03 |
| Left atrial diameter (mm) | 40 ± 7 | 43 ± 7 | 39 ± 7 | 0.03 |
| E/e′ ratio | 12.8 ± 5.3 | 15.7 ± 7.3 | 12.0 ± 4.4 | 0.002 |
| CFR | 2.5 ± 0.7 | 2.0 ± 0.7 | 2.6 ± 0.7 | <0.001 |
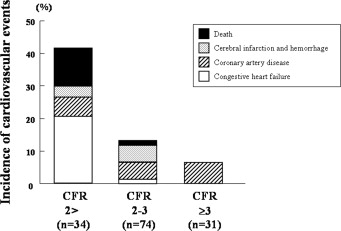
During a mean follow-up period of 3.3 ± 1.6 years, ranging from 1 year to 8 years, the primary end point was observed in 26 patients (18.7%); 18 cardiac events and 8 noncardiac events. Cardiac events included cardiac death in 2 patients, nonfatal myocardial infarction in 4, unstable angina pectoris in 3, elective coronary bypass graft surgery in 1, and heart failure in 8; noncardiac events included noncardiac death in 3 patients, cerebral infarction in 4, and cerebral hemorrhage in 1. Figure 1 demonstrates the incidence of all CV events according to CFR values. Of the 34 patients with CFR <2.0, CV events occurred in 14 patients (41%). In contrast, only 2 patients (6.5%) developed CV events of those with a CFR of ≥3.0. Table 1 summarizes the clinical characteristics of patients with and without CV events. Patients with CV events had a higher serum CRP level, lower eGFR, increased left ventricular mass index, enlarged left atrium, higher E/e′ ratio, and decreased CFR than those without CV events. Cox proportional hazard analysis adjusted for CV risk factors identified serum CRP level and CFR as independent risk factors for CV events ( Table 2 ). Kaplan-Meier analysis showed significantly worse event-free survival in patients with CFR of <2.0 compared with those with CFR of ≥2.0 ( Figure 2 ).
| Variables | Hazard Ratio | 95% CI | p |
|---|---|---|---|
| Model 1: no adjustment | |||
| CRP (mg/L) | 1.36 | 0.99–1.84 | 0.05 |
| eGFR (ml/min/1.73 m 2 ) | 0.99 | 0.95–1.03 | 0.5 |
| Left ventricular mass index (g/m 2 ) | 1.01 | 0.99–1.02 | 0.4 |
| Left atrial diameter (mm) | 1.02 | 0.95–1.08 | 0.6 |
| E/e′ ratio | 1.08 | 0.99–1.16 | 0.05 |
| CFR | 0.32 | 0.13–0.83 | 0.02 |
| Model 2: adjusted for age, gender, hypertension, hypercholesterolemia, and diabetes mellitus | |||
| CRP (mg/L) | 1.41 | 1.04–1.94 | 0.03 |
| eGFR (ml/min/1.73 m 2 ) | 1.01 | 0.95–1.07 | 0.7 |
| Left ventricular mass index (g/m 2 ) | 1.01 | 0.99–1.02 | 0.4 |
| Left atrial diameter (mm) | 1.02 | 0.95–1.09 | 0.6 |
| E/e′ ratio | 1.08 | 0.99–1.17 | 0.09 |
| CFR | 0.21 | 0.06–0.68 | 0.009 |
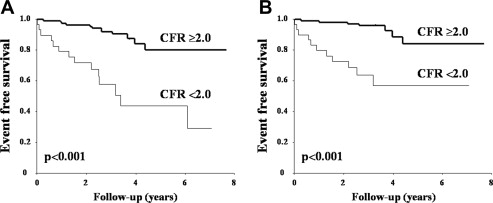
Cox proportional hazard analysis with the adjustment of CV risk factors was repeated including only cardiac events as the primary end point and identified serum CRP level and CFR as significant determinants of future development of cardiac events ( Table 3 ). An increased frequency of cardiac events was observed in patients with CFR of <2.0 compared with those with CFR of >2.0 ( Figure 2 ).



