Using a novel graded outcomes scale, the investigators evaluated whether left atrial (LA) volume measured by cardiac computed tomographic angiography is a predictor of pulmonary vein isolation success in patients with nonparoxysmal atrial fibrillation (AF) and paroxysmal AF (PAF). Data from 45 patients who underwent electrocardiographically gated computed tomographic angiography before pulmonary vein isolation for AF were used. LA volume was measured in the ventricular systolic and diastolic phases, defined as 40% and 75% of the interval between consecutive R waves. Outcomes were graded at 0 to 3, 3 to 6, 6 to 12, and 12 to 24 months after pulmonary vein isolation and scored on a 5-point scale: 1 = no AF recurrence off antiarrhythmic drug, 2 = no AF recurrence on antiarrhythmic drug, 3 = rare AF (<1 episode in 3 months), 4 = asymptomatic recurrent AF, and 5 = no reductions in AF frequency or severity. LA volumes were significantly larger in the nonparoxysmal AF group compared with the PAF group in systole (159.2 vs 128.2 ml, p <0.001) and diastole (137.1 vs 104.0 ml, p <0.001). In patients with PAF, larger LA volume was correlated with worse clinical outcomes in the first 12 months, but the results did not reach statistical significance (systole r = 0.25 to 0.41, diastole r = 0.20 to 0.34). In conclusion, these results show a significant difference in LA volume in patients with nonparoxysmal AF and PAF in systole and diastole. Additionally, there was a correlation between LA volume and clinical outcomes in patients with PAF, although this did not reach statistical significance.
Pharmacologic agents have been the long-standing mode of treatment for atrial fibrillation (AF) through the maintenance of sinus rhythm or management of heart rate. More recently, radiofrequency catheter ablation has been offered as an alternative or adjunct to pharmacologic therapy in patients either with refractory AF or with intolerance to antiarrhythmic drugs (AADs). Despite advances in ablation therapy, recurrences of AF occur, with success rates reported at 68% to 86% at 1 year. This study was performed to demonstrate the predictive value of left atrial (LA) size during systole and diastole for graded clinical outcomes at various time intervals after ablation procedures performed for AF, including patients with nonparoxysmal AF (NPAF) and paroxysmal AF (PAF).
Methods
We evaluated consecutive patients referred for pulmonary vein isolation (PVI) who underwent electrocardiographically gated computed tomographic angiography at our institution. PVI success was defined using a novel graded outcomes scale to quantify clinical success after ablation. Previous studies have used a binary scale (recurrence vs no recurrence of AF) to grade clinical outcome. For the present study, we used a graded scale to better quantify the success of ablation therapy ( Table 1 ).
| Score | Interpretation |
|---|---|
| 1 | No AF recurrence without AADs |
| 2 | No AF recurrence with AADs |
| 3 | Rare AF (<1 episode in 3 mos) |
| 4 | Asymptomatic recurrent AF |
| 5 | No improvement in AF frequency or severity |
All multidetector computed tomographic examinations were performed using a helical acquisition on a 256-slice iCT scanner (Philips Medical Systems, Cleveland, Ohio) during the injection of 60 to 70 ml of iodinated contrast material (iodine concentration 350 mg/ml). The standard scanning parameters for this study were a tube voltage of 120 kVp and a tube current of 600 mAs per section. Tube current was increased to 800 to 1,000 mAs per section on the basis of estimated weight for patients weighing 200 to 250 lb (90.7 to 113.4 kg). Electrocardiographically based tube current modulation was used for dose reduction in all patients with regular heart rates ≤65 beats/min.
For the purpose of LA volume measurements, transaxial images through the heart were reconstructed at end-systole and mid-diastole. To determine the end-systolic phase, contiguous images were reconstructed at 10 evenly spaced phases throughout the RR interval with a slice thickness of 3 mm. A cine loop encompassing the entire RR cycle was created with these phases to identify the phase with the largest LA size, typically at 30% or 40% of the RR interval. Diastolic phase images were obtained at 75% of the RR interval. LA volume was measured in the systolic and diastolic phases with automated chamber reconstruction using the EP Planning package (Brilliance Workstation; Philips Medical Systems), with automatic edge detection of the LA endocardial borders. The automated chamber reconstruction volume was manually checked and edited to ensure that it included the entire left atrium, including the LA appendage, but excluded the pulmonary veins. The LA volume determined using this technique was recorded, and the LA appendage was then manually removed and a second LA volume recorded without the LA appendage.
All patients were referred for catheter ablation of AF and provided written informed consent in accordance with institutional policy. AADs were variably stopped before the procedure. In brief, multipolar catheters were placed in the coronary sinus and right atrium, and a 10Fr diagnostic ultrasound catheter (5.5 to 10 MHz) (AcuNav; Biosense Webster, Diamond Bar, California) was placed in the right atrium. Two atrial transseptal punctures were performed, and an ablation catheter and a circular mapping catheter (Lasso; Biosense Webster) were advanced into the left atrium. Three-dimensional electroanatomic mapping was performed using the CARTO system (Biosense Webster). All pulmonary veins were routinely isolated. Radiofrequency ablation was delivered with an 8-mm tipped catheter or a 3.5-mm open-irrigated tip catheter. Lesions were routinely delivered for a maximum of 30 to 60 seconds to achieve an decrease in impedance of 5 to 10 Ω at the ablation site. Successful PV isolation was defined by the loss of all pulmonary vein potentials (entrance block) and failure to capture the left atrium when pacing from the Lasso catheter at the ostium of each pulmonary vein (exit block). Attempts at reinduction with burst pacing were performed and recorded.
Patients were followed up periodically with routine office visits at up 1, 3, 6, 12, and 24 months or if there was a report of symptoms. Standard electrocardiography was performed at each follow-up visit to assess AF status. Statistical analyses were performed using a 2-tailed Student’s t tests. A p value <0.05 was considered statistically significant. Data are expressed as mean ± SD or as number (percentage). Correlations between variables were determined using Pearson’s correlation coefficient. How well LA volumes differentiated patients with and without AF recurrence was assessed by means of the area under a receiver-operating characteristic curve. The LA ejection fraction was defined as (LA end-systolic volume − LA end-diastolic volume)/LA end-systolic volume.
Results
The patient population included a total of 45 patients with PAF or NPAF who subsequently underwent electrocardiographically gated computed tomographic angiography before PVI ( Table 2 ). Twenty patients (45%) had NPAF and 25 (55%) had PAF. Of the study group, there were 32 male patients (72%) and 13 female patients (28%). The mean age in each group was also similar. Thirty-two patients (73%) were receiving AAD therapy before PVI, whereas 13 (27%) were not. However, 11 of the 13 patients had been taking AADs at some point before PVI. The procedural end point of PVI (bidirectional block) was achieved in all patients. Data from the most recent procedure were recorded.
| Variable | PAF | NPAF |
|---|---|---|
| Age (yrs) | 54 | 53 |
| Men/women | 18/7 | 14/6 |
| AAD before PVI | 13 (54%) | 19 (95%) |
| Total | 25 | 20 |
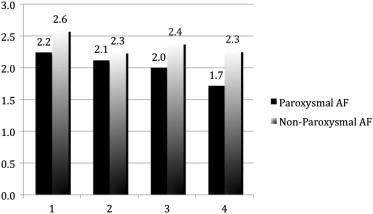
The mean results for LA volume attained from electrocardiographically gated cardiac computed tomographic angiography are shown in Figure 1 . As seen in previous studies, atrial volume measured in ventricular systole by computed tomography was markedly enlarged in patients with NPAF compared with those with PAF, as was diastolic volume. Those with NPAF had greater LA appendage volumes in systole and diastole compared with those with PAF. A receiver-operating characteristic curve showed that an optimal cutoff point of 153 ml yielded diagnostic accuracy of 73%, with sensitivity of 28% and specificity of 95% for AF recurrence. Thus, patients with very large LA volumes (>153 ml) are more likely to have recurrence.
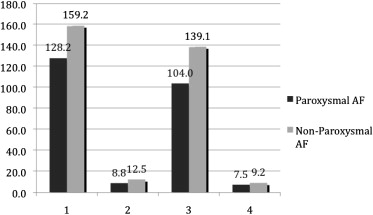
Of all 45 patients (with PAF and NPAF), 33 reached the follow-up period of 12 to 24 months, and all but 1 (lost to follow-up) reached 6 to 12 months after PVI. Nineteen patients (43.7%) were in sinus rhythm without any AADs at the end of the follow-up period, whereas 11 (25%) had done so with AADs. Seven patients (15.8%) had rare AF, 1 (2%) had recurrent AF without any symptoms, and 6 (13.5%) had no change in the frequency or severity of AF after PVI ( Figure 2 ).
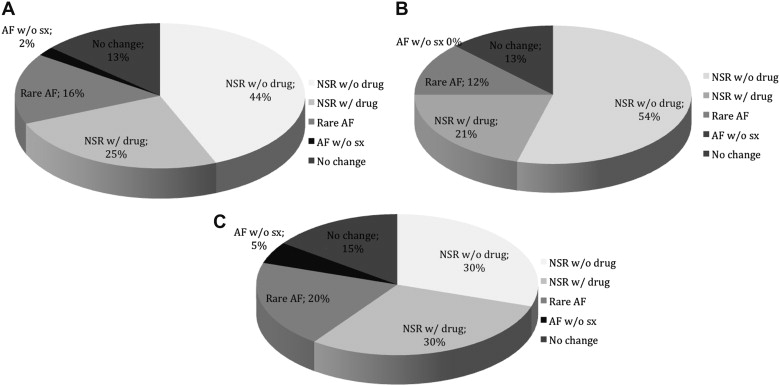
In the PAF population, 54% of patients maintained sinus rhythm without AADs and 21% with AADs ( Figure 2 ). In addition, 12% of patients in the PAF group had occurrences of rare AF, none had asymptomatic recurrent AF, and 13% had no changes in the frequency or severity of AF after PVI. In the NPAF group, 30% of patients maintained sinus rhythm without AADs, and 30% of patients maintained sinus rhythm with AADs ( Figure 2 ). Twenty percent of patients in the NPAF group had occurrences of rare AF, 5% had asymptomatic AF, and 15% had no changes in the frequency or severity of AF after PVI. Patients with NPAF had worse clinical outcomes compared with those with PAF at 3, 6, 12, and 24 months ( Figure 3 ). This difference was statistically significant (p = 0.036). In the entire cohort, those who achieved normal sinus rhythm with or without AADs had smaller LA volumes and LA appendage volumes in systole as well as diastole compared with those with recurrent AF or no change in AF severity ( Figure 4 ).