Although lesion complexity is predictive of outcomes after balloon angioplasty, it is unclear whether complex lesions continue to portend a worse prognosis in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI) with contemporary interventional therapies. We sought to assess the impact of angiographic lesion complexity, defined by the modified American College of Cardiology/American Heart Association classification, on clinical outcomes after PCI in patients with ACS and to determine whether an interaction exists between lesion complexity and antithrombin regimen outcomes after PCI. Among the 3,661 patients who underwent PCI in the Acute Catheterization and Urgent Intervention Triage strategy study, patients with type C lesions (n = 1,654 [45%]) had higher 30-day rates of mortality (1.2% vs 0.6%, p = 0.049), myocardial infarction (9.2% vs 6.3%, p = 0.0006), and unplanned revascularization (4.3% vs 3.1%, p = 0.04) compared with those without type C lesions. In multivariate analysis, type C lesions were independently associated with myocardial infarction (odds ratio [95% confidence interval] = 1.37 [1.04 to 1.80], p = 0.02) and composite ischemia (odds ratio [95% confidence interval] = 1.49 [1.17 to 1.88], p = 0.001) at 30 days. Bivalirudin monotherapy compared with heparin plus a glycoprotein IIb/IIIa inhibitor reduced major bleeding complications with similar rates of composite ischemic events, regardless of the presence of type C lesions. There were no interactions between antithrombotic regimens and lesion complexity in terms of composite ischemia and major bleeding (p [interaction] = 0.91 and 0.80, respectively). In conclusion, patients with ACS with type C lesion characteristics undergoing PCI have an adverse short-term prognosis. Treatment with bivalirudin monotherapy reduces major hemorrhagic complications irrespective of lesion complexity with comparable suppression of adverse ischemic events as heparin plus glycoprotein IIb/IIIa inhibitor.
The modified American College of Cardiology/American Heart Association (ACC/AHA) lesion morphology classification was devised and validated for outcomes after balloon angioplasty. Whether lesion complexity, as defined by the original ACC/AHA criteria, remains valuable in assessing the prognosis of patients with acute coronary syndrome (ACS) who undergo percutaneous coronary intervention (PCI) has not been studied in a contemporary trial. Furthermore, in the treatment of non–ST-segment elevation ACS, early use of antithrombin and antiplatelet therapy plays a key role in improving patient outcomes. The benefit of bivalirudin monotherapy in reducing bleeding risk while suppressing adverse ischemic events has been demonstrated to date in several high-risk patient groups including patients with diabetes and chronic kidney disease. However, the safety and efficacy of bivalirudin monotherapy in patients with ACS with high-risk angiographic lesions has not been evaluated. In the current analysis, we investigate the impact of angiographic lesion morphology and complexity on short-term outcomes and the safety and efficacy of bivalirudin monotherapy in angiographic high-risk patients treated with PCI.
Methods
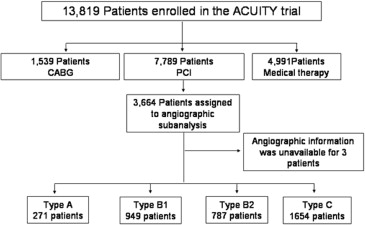
The design of the Acute Catheterization and Urgent Intervention Triage strategy (ACUITY) trial has been published previously. In brief, the ACUITY trial randomized 13,819 patients with moderate or high-risk non–ST-segment elevation ACS to receive unfractionated heparin or enoxaparin with a glycoprotein IIb/IIIa inhibitor (GPI), bivalirudin plus a GPI, or bivalirudin monotherapy. The antithrombin and antiplatelet drug-dosing regimens have been previously described. Patients assigned to heparin plus a GPI or bivalirudin plus a GPI were randomly assigned again in a 2-by-2 factorial design to either upstream or deferred initiation of a GPI. In patients assigned to bivalirudin monotherapy, GPI administration was reserved for “bail-out” use at operator discretion for procedural PCI complications or suboptimal results. Coronary angiography was required within 72 hours of randomization with subsequent triage to PCI, coronary artery bypass grafting (CABG), or medical management. The study was approved by the institutional review board or ethics committee at each participating center, and all patients signed a written informed consent.
The ACUITY trial included a prespecified angiographic substudy in 6,921 consecutive patients from selected centers in the United States. An independent angiographic core laboratory (Cardiovascular Research Foundation, New York, New York) analyzed all preprocedural and final angiograms using standardized definitions including the baseline ACC/AHA lesion complexity criteria (interobserver and intraobserver Kappa statistic >0.7; data on file at the Cardiovascular Research Foundation) by reviewers blinded to the treatment assignment. The lesions were classified according to the ACC/AHA grading system. In addition, we compared the outcomes based on the more recent Society for Cardiac Angiography and Interventions (SCAI) classification, which includes 4 subgroups: (1) nontype C with patent vessel (Thrombolysis in Myocardial Infarction [TIMI] grade 2/3 flow), (2) nontype C with occluded vessel (TIMI grade 0/1 flow), (3) type C with patent vessel, and (4) type C with occluded vessel. To quantify the extent and burden of coronary artery disease (CAD), the angiographic analysis also included the number of diseased vessels (defined by a diameter stenosis of at least 30% in a major epicardial vessel), the extent of CAD burden (the total length in millimeters of all lesions with a >30% diameter stenosis in a major epicardial vessel), the jeopardy score, baseline TIMI grade flow, and myocardial blush grade.
Patient demographics and outcomes were compared based on lesion complexity as defined by ACC/AHA type C versus nontype C lesions. For patients with ≥2 intervened lesions, patients were selected on the basis of the intervened lesion with the worst morphology, and thrombotic occlusions were not included in the definition of chronic total occlusions. The primary end point of this subanalysis was composite ischemia (defined as death from any cause, myocardial infarction [MI], or unplanned revascularization for ischemia) at 30 days. In addition, we analyzed (1) components of composite ischemia at 30 days, (2) stent thrombosis (Academic Research Consortium definition; definite or probable) at 30 days, and (3) non-CABG related major and minor bleeding at 30 days according to ACUITY protocol definitions. All end points were adjudicated by an independent blinded clinical events committee.
Categorical values were compared by the chi-square or Fisher’s exact test. Continuous variables are presented as medians with interquartile ranges, and these were compared using Kruskal-Wallis test. Thirty-day follow-up analysis was performed using time-to-event method and compared with the log-rank test, based on the ACC/AHA classification and SCAI lesion classification. Interaction testing was performed to assess interaction between treatment allocation (heparin plus a GPI vs bivalirudin plus a GPI vs bivalirudin monotherapy) and lesion complexity for composite ischemia and bleeding complications. To examine the impact of lesion complexity on 30-day outcomes, logistic regression analysis was conducted. The covariates included in the model were the lesion complexity (type A vs B1 vs B2 vs C), age, gender, diabetes, insulin-treated diabetes, hypertension, hyperlipidemia, smoking status, renal insufficiency, anemia, number of white blood cells, previous PCI, previous CABG, previous MI, cardiac biomarker elevation, ST-segment deviation, bivalirudin plus a GPI (vs heparin plus a GPI), bivalirudin monotherapy (vs heparin plus a GPI), PCI procedure (drug-eluting stent vs bare-metal stent), and the number of stents (single stent vs multiple stents). The p values, odds ratios, and corresponding 2-sided 95% confidence interval for predictors are presented. To compare the relative value of a predictive model based on ACC/AHA classification versus SCAI classification, we used receiver operating characteristic method and the C-statistic for the 30-day composite ischemia as well as the regression model previously mentioned forcing both classifications in the model. All statistical analyses were performed by SAS version 8.2 (SAS Institute Inc., Cary, North Carolina).
Results
Of the 13,819 patients in the ACUITY trial, 7,789 patients (56.4%) were triaged to PCI. Complete baseline and postprocedural angiographic data were available in 3,661 patients in the angiographic substudy, including 271 patients with type A lesions, 949 patients with type B1 lesions, 787 patients with type B2 lesions, and 1,654 patients with type C lesions ( Figure 1 ).
Patients with versus without type C lesions were more likely to be men, had lesser prevalence of co-morbidities including hypertension and hyperlipidemia, and had lower incidence of previous PCI ( Table 1 ). Although cardiac biomarker elevation and ST-segment deviation were more common in patients with type C lesions, the distribution of TIMI risk scores (low, intermediate, and high) was similar between groups.
| Variable | Type C Lesions | p value | |
|---|---|---|---|
| Yes (N=1654) | No (N=2007) | ||
| Age (years) | 61 [53, 70] | 61 [53, 71] | 0.71 |
| Men | 1204 (72.8%) | 1348 (67.2%) | 0.0002 |
| Weight (kilogram) | 86.3 [75.8, 100.0] | 88.0 [75.8, 102.0] | 0.10 |
| Diabetes mellitus | 509/1650 (30.8%) | 656/1995 (32.9%) | 0.20 |
| Insulin-treated diabetes | 141/1650 (8.5%) | 198/1995 (9.9%) | 0.17 |
| Hypertension | 1103/1651 (66.8%) | 1456/1995 (73.0%) | <0.0001 |
| Hyperlipidemia | 981/1633 (60.1%) | 1268/1984 (63.9%) | 0.02 |
| Current smoker | 549/1647 (33.3%) | 595/2000 (29.8%) | 0.02 |
| Prior myocardial infarction | 550/1616 (34.0%) | 691/1952 (35.4%) | 0.40 |
| Prior percutaneous coronary intervention | 716/1644 (43.6%) | 1038/2000 (51.9%) | <0.0001 |
| Prior coronary artery bypass grafting | 364/1648 (22.1%) | 445/2006 (22.2%) | 0.97 |
| Renal insufficiency ∗ | 265/1554 (17.1%) | 322/1870 (17.2%) | 0.93 |
| High risk † | 1160/1565 (74.1%) | 1135/1895 (59.9%) | <0.0001 |
| Creatinine Kinase-MB/troponin elevation | 1014/1543 (65.7%) | 916/1854 (49.4%) | <0.0001 |
| ST-segment deviation | 464/1654 (28.1%) | 481/2007 (24.0%) | 0.005 |
| Thrombolysis in myocardial infarction risk score | |||
| 0-2 (low) | 182/1360 (13.4%) | 204/1635 (12.5%) | 0.48 |
| 3-4 (intermediate) | 736/1360 (54.1%) | 934/1635 (57.1%) | 0.10 |
| 5-7 (high) | 442/1360 (32.5%) | 497/1635 (30.4%) | 0.22 |
∗ Renal insufficiency – calculated creatinine clearance <60 mL/min using the Cockcroft-Gault equation.
† High risk was defined as either: CKMB or troponin elevation or ST-deviation.
Patients with type C lesions had a lower ejection fraction and by definition more complex lesion characteristics, including a greater prevalence of TIMI flow grade 0 and/or 1, eccentricity, ulceration, moderate or severe calcification, thrombus, and collaterals ( Table 2 ). In addition, patients with type C lesions had a greater coronary atherosclerotic burden, including higher frequency of 3-vessel disease, greater number of diseased lesions, higher jeopardy score, and greater extent of CAD. The SCAI classification for this study cohort included 1,746 patients (47.8%) nontype C with patent vessel, 255 (7.0%) nontype C with occluded vessel, 1,102 (30.2%) type C with patent vessel, and 549 (15.0%) type C with occluded vessel.
| Variable | Type C Lesions | p value | |
|---|---|---|---|
| Yes (N=1654) | No (N=2007) | ||
| Ejection fraction (%) | 63 [55, 71] | 66 [58, 74] | <0.0001 |
| Target coronary artery | |||
| Left anterior descending | 656 (39.7%) | 846 (42.2%) | 0.13 |
| Left circumflex | 626 (37.8%) | 729 (36.3%) | 0.35 |
| Right | 728 (44.0%) | 711 (35.4%) | <0.0001 |
| No. coronary arteries narrowed: | |||
| 0 | 8 (0.5%) | 12 (0.6%) | 0.82 |
| 1 | 266 (16.1%) | 429 (21.4%) | <0.0001 |
| 2 | 554 (33.5%) | 683 (34.0%) | 0.75 |
| 3 | 826 (49.9%) | 883 (44.0%) | 0.0004 |
| Thrombolysis in myocardial infarction flow grade 0/1 | 549/1651 (33.3%) | 255/2001 (12.7%) | <0.0001 |
| Blush score 0/1 | 514/1557 (33.0%) | 263/1873 (14.0%) | <0.0001 |
| Number of coronary narrowings | 4.6 ± 2.6 | 4.1 ± 2.6 | <0.0001 |
| Number of treated arteries | 1.2 ± 0.4 | 1.1 ± 0.4 | <0.0001 |
| Extent of coronary artery disease (mm) | 40.7 [25.1, 61.7] | 28.0 [17.1, 43.3] | <0.0001 |
| Jeopardy score | 3.0 ± 2.3 | 2.3 ± 2.3 | <0.0001 |
| Worst lesion characteristics | |||
| Eccentric | 477/1652 (28.9%) | 445/2001 (22.2%) | <0.0001 |
| Ulceration | 146/1653 (9.0%) | 117/2001 (5.8%) | 0.0003 |
| Aneurysm | 77/1653 (4.7%) | 71/2001 (3.5%) | 0.09 |
| Calcium (moderate) | 614/1652 (37.2%) | 478/2001 (23.9%) | <0.0001 |
| Calcium (severe) | 181/1652 (11.0%) | 125/2001 (6.2%) | <0.0001 |
| Thrombus | 560/1653 (33.9%) | 244/2001 (12.2%) | <0.0001 |
| Collateral presence | 594 (35.9%) | 374 (18.6%) | <0.0001 |
Multiple stent implantation was more common in patients with type C lesions compared with those without ( Table 3 ). PCI of type C lesions was associated with a greater volume of contrast medium use and longer procedural time. Patients with type C lesions had a higher incidence of final TIMI flow grade 0/1 and blush score 0/1. Procedural complications including abrupt vessel closure, distal embolization, and no reflow phenomenon during the index PCI were rare in both groups, although significantly more common in patients with type C lesions. Patients with type C lesions also had a greater final percent diameter stenosis than those without.
| Variable | Type C Lesions | p value | |
|---|---|---|---|
| Yes (N=1654) | No (N=2007) | ||
| Procedural data | |||
| Stent implanted | 1570 (94.9%) | 1856 (92.5%) | 0.003 |
| Drug eluting stent | 1411 (85.3%) | 1680 (83.7%) | 0.18 |
| Bare metal stent | 285 (17.2%) | 280 (14.0%) | 0.007 |
| Drug eluting and bare metal stent | 126 (7.6%) | 104 (5.2%) | 0.003 |
| Multiple stents implanted | 515 (31.1%) | 428 (21.3%) | <0.0001 |
| Duration of procedure (minutes) | 32 [20, 51] | 21 [13, 35] | <0.0001 |
| Contrast media (milliliter) | 250 [180, 350] | 210 [160, 300] | <0.0001 |
| Randomization group | |||
| Heparin plus glycoprotein IIb/IIIa inhibitor | 545 (33.0%) | 645 (32.1%) | 0.62 |
| Bivalirudin plus glycoprotein IIb/IIIa inhibitor | 559 (33.8%) | 694 (34.6%) | 0.62 |
| Bivalirudin monotherapy | 550 (33.3%) | 668 (33.3%) | 1.00 |
| Final angiographic data | |||
| Thrombolysis in myocardial infarction flow grade | |||
| 0/1 | 45/1637 (2.7%) | 19/1989 (1.0%) | <0.0001 |
| 2 | 46/1637 (2.8%) | 35/1989 (1.8%) | 0.04 |
| 3 | 1547/1637 (94.5%) | 1935/1989 (97.3%) | <0.0001 |
| Blush score | |||
| 0/1 | 61/1403 (4.3%) | 23/1709 (1.3%) | <0.0001 |
| 2 | 185/1403 (13.2%) | 188/1709 (11.0%) | 0.07 |
| 3 | 1160/1403 (82.7%) | 1498/1709 (87.7%) | 0.0001 |
| Thrombus | 416/1638 (25.4%) | 112/1986 (5.6%) | <0.0001 |
| Abrupt closure | 21/1636 (1.3%) | 7/1986 (0.4%) | 0.002 |
| No reflow | 14/1636 (0.9%) | 5/1985 (0.3%) | 0.02 |
| Perforation | 6/1636 (0.4%) | 1/1986 (0.1%) | 0.051 |
| Distal embolization | 24/1628 (1.5%) | 5/1981 (0.3%) | <0.0001 |
| Quantitative coronary angiography | |||
| Reference diameter (millimeter) | 2.85 ± 0.57 | 2.75 ± 0.55 | <0.0001 |
| Minimum lumen diameter (millimeter) | 2.32 ± 0.59 | 2.32 ± 0.56 | 0.89 |
| Diameter stenosis (%) | 18.5 ± 13.0 | 16.0 ± 10.1 | <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


