Several coronary disease scoring systems have been developed to predict procedural risk during revascularization. Many vary in complexity, do not specifically account for myocardium at risk, and are not applicable across all patient subsets. The British Cardiovascular Intervention Society myocardial jeopardy score (BCIS-JS) addresses these limitations and is applicable to all patients, including those with coronary artery bypass grafts or left main stem disease. We assessed the prognostic relevance of the BCIS-JS in patients undergoing percutaneous coronary intervention (PCI). A total of 663 patients who underwent PCI with previous left ventricular function assessment were retrospectively assessed for inclusion, incorporating 221 with previous coronary artery bypass grafting. Blinded observers calculated the BCIS-JS, before (BCIS-JS PRE ) and after (BCIS-JS POST ) PCI, using the revascularization index (RI) (RI = [BCIS-JS PRE − BCIS-JS POST ]/BCIS-JS PRE ), quantifying the extent of revascularization, 1 indicating full revascularization and 0 indicating no revascularization. The primary end point all-cause mortality, tracked via the Office of National Statistics. A total of 660 patients were included (66 ± 10.7 years), with 43 deaths (6.5%) occurring during 2.6 ± 1.1 years after PCI. All-cause mortality was directly related to BCIS-JS PRE (hazard ratio [HR] 2.96, 95% confidence interval [CI] 1.71 to 5.15, p = 0.001) and BCIS-JS POST (HR 4.02, 95% CI 2.41 to 6.68, p = 0.001). A RI of <0.67 was associated with increased mortality compared to a RI of ≥0.67 (HR 4.13, 95% CI 1.91 to 8.91, p = 0.0001). On multivariate analysis, a RI <0.67 (HR 1.99, 95% CI 1.03 to 3.87, p = 0.04), left ventricular dysfunction (HR 2.03, 95% CI 1.25 to 3.30, p = 0.004) and renal impairment (HR 3.75, 95% CI 1.48 to 8.64, p = 0.005) were independent predictors of mortality. In conclusion, the BCIS-JS predicts mortality after PCI and can assess the degree of revascularization, with more complete revascularization conferring a survival advantage in the medium term.
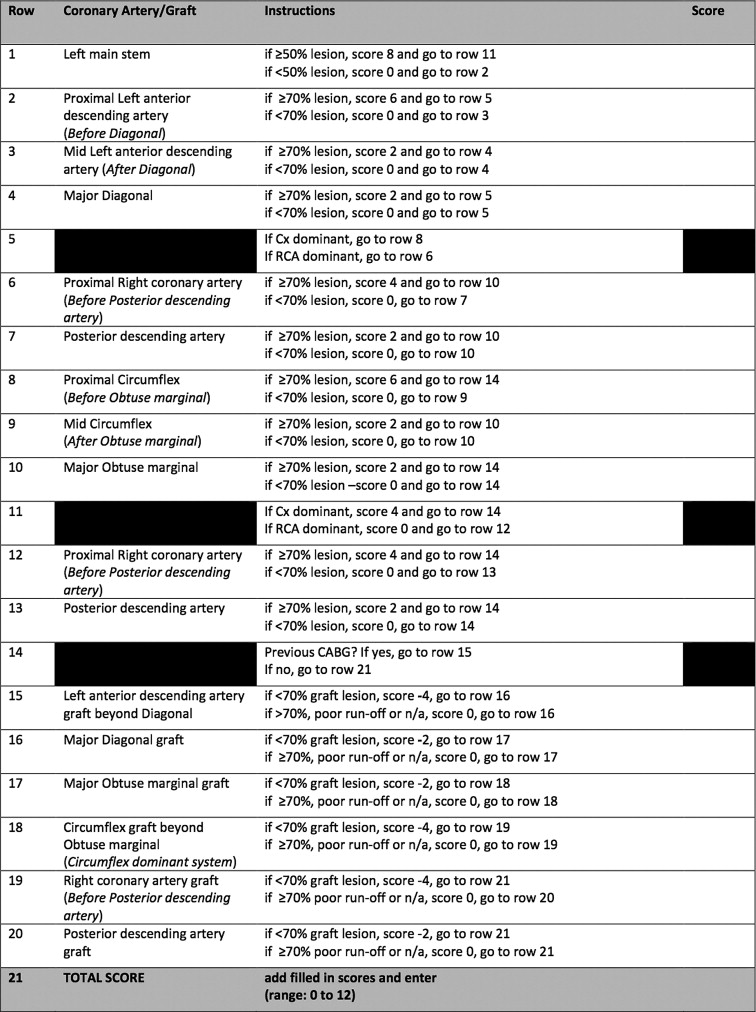
The recently described British Cardiovascular Intervention Society myocardial jeopardy score (BCIS-JS) is a modification of the Duke Jeopardy Score scoring system. The BCIS-JS accommodates classification of left main coronary artery disease and coronary bypass graft disease, maintaining the simplicity of the original Duke Jeopardy Score ( Figure 1 ). The purpose of the present study was to investigate the prognostic value of the BCIS-JS in determining all-cause mortality in a cohort of patients, with native coronary and graft disease, after percutaneous coronary intervention (PCI).
Methods
A total of 663 patients who underwent PCI at a single United Kingdom center (St. Thomas’ Hospital, London) from April 2007 to February 2009 were retrospectively included in the present study. The patients were eligible for inclusion if a minimum prespecified data set had been prospectively entered in the database at PCI, including categorization of left ventricular (LV) function on the basis of the echocardiographic or left ventricular angiographic findings. The patients were excluded if complete pre-PCI diagnostic angiograms were unavailable for review and classification. One of the unique strengths of the BCIS-JS is its ability to classify patients with previous coronary artery bypass grafting (CABG). To reflect this, we enrolled all patients with previous CABG, who underwent PCI during the sampling period, subject to the overall eligibility criteria (n = 221 CABG patients). To ensure applicability of the score to the wider population of patients undergoing PCI, we included consecutive patients who underwent PCI during this period and did not have a history of CABG, to achieve a ratio of 1 CABG patient to 2 non-CABG patients overall (n = 442 non-CABG patients; Table 1 ).
| Demographic/Procedural Variables | Total (n = 660) |
|---|---|
| Mean age (yrs) | 66.0 ± 10.7 |
| Men | 503 (76.2%) |
| Diabetes mellitus | 143 (21.6%) |
| Renal dysfunction ∗ | 33 (5.0%) |
| Cardiogenic shock † | 14 (2.1%) |
| Previous coronary artery bypass grafting | 218 (33.0%) |
| Left ventricular ejection fraction <50% | 206 (31.2%) |
| Coronary arteries treated (n) | |
| 1 | 565 (85.6%) |
| ≥2 | 96 (14.5%) |
| Urgency of percutaneous coronary intervention | |
| Elective | 290 (44.0%) |
| Urgent/emergency | 370 (56.0%) |
∗ Renal dysfunction defined as creatinine of >200 mmol/L at PCI.
† Cardiogenic shock defined as sustained hypotension (systolic blood pressure <90 mm Hg) for ≥30 minutes with evidence of tissue hypoperfusion despite adequate LV filling pressure.
Coronary angiography was performed according to standard techniques and included multiple projections of each artery to visualize stenosis severity. Experienced interventional cardiologists, who were unaware of the clinical and outcomes data, analyzed the diagnostic and procedural coronary angiograms. Stenosis severity was assessed visually, and the BCIS-JS recorded before and after PCI (BCIS-JS PRE and BCIS-JS POST , respectively). Calculation of the BCIS-JS has been previously described. In brief, it is designed to be calculated from visual assessment of the angiogram both for ease of use and to reflect clinical practice. The previously devised Duke Jeopardy Score ascribes 2 points each for 6 myocardial territories, those subtended by the left anterior descending artery, diagonal branch, circumflex artery, obtuse marginal branch, right coronary artery, and posterior descending branch arteries. Two points are allocated to each coronary lesion plus 2 additional points if the lesion affects 2 of the 6 downstream myocardial territories. The BCIS-JS is a modification of this scoring system and allows classification of left main coronary artery disease and CABG disease. Coronary or graft lesions with ≥70% diameter stenosis on visual estimation should be considered significant. Left main coronary lesions of ≥50% should be considered significant and given a score of 8 points. In cases in which a main vessel gives rise to multiple branches (diagonal branch, obtuse marginal branch, or posterior descending branch), only lesions in the branch supplying the largest territory (termed the “major branch” Figure 1 ) should be scored. For anatomic variations, equivalent myocardial territories should be assessed. For example, the ramus intermedius branch could be scored as a major diagonal branch or major obtuse marginal branch, if considered to supply a similar territory. When a right coronary artery is dominant, the proximal circumflex artery should be scored as a major obtuse marginal branch. For true anatomic co-dominance, the right coronary artery should be considered dominant for scoring. This takes into account the entire myocardial area at risk by a subsequent ischemic insult, with the score accounting for the territories supplied by the circumflex artery and left anterior descending artery. Native coronary arteries are scored and points are then deducted for patent grafts to these territories, where applicable. Coronary artery dominance is determined by whether the right coronary artery or circumflex artery supplies the posterior descending branch. Scores thus range from a minimum of 0 to a maximum of 12 ( Figure 1 ). We also calculated a novel revascularization index (RI), in which RI = (BCIS-JS PRE − BCIS-JS POST )/BCIS-JS PRE . Complete revascularization of the 6 territories thus results in an RI of 1, and an unchanged BCIS-JS after the procedure would result in an RI of 0 ( Figure 1 ).
The primary end point was all-cause mortality. Mortality data were obtained from the United Kingdom Office of National Statistics.
Statistical analysis was performed using SPSS, version 17 (SPSS, Chicago, Illinois). The RI was categorized numerically into tertiles, according to the extent of revascularization, the potential reduction in myocardial jeopardy, with 0 to 0.33 indicating no or minimal successful revascularization, 0.34 to 0.66 indicating intermediate revascularization, and 0.67 to 1.0 indicating near-complete or complete revascularization.
Dichotomous data are expressed as numbers and percentages and continuous data as mean ± SD. Categorical variables were analyzed using the chi-square test or (where stated) Fisher’s exact test, with continuous variables analyzed using analysis of variance. The correlation between baseline variables and all-cause mortality was assessed by univariate analysis; these included BCIS-JS PRE , BCIS-JS POST , RI, age, gender, diabetes, LV dysfunction (LV ejection fraction <50%), renal impairment, acuity of presentation, presence of cardiogenic shock, and previous CABG. All variables were strongly associated with mortality on univariate analysis (p <0.05) were incorporated into a multivariate Cox regression analysis. Each BCIS-JS category (BCIS-JS PRE , BCIS-JS POST , and RI) were assessed against each covariate in separate multivariate analyses; however, for clarity, they have been tabulated together ( Table 2 ).
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age | 1.04 (1.01–1.08) | 0.01 | 1.03 (1.00–1.07) | 0.072 |
| Male gender | 4.16 (1.29–13.47) | 0.02 | 2.77 (0.80–9.53) | 0.106 |
| Diabetes mellitus | 1.59 (0.80–3.13) | 0.184 | NA | NA |
| Left ventricular ejection fraction <50% | 3.76 (2.53–5.58) | 0.001 | 2.03 (1.25–3.30) | 0.004 |
| Renal dysfunction | 4.29 (1.86–9.93) | 0.001 | 3.57 (1.48–8.64) | 0.005 |
| Acute coronary syndrome | 2.31 (1.24–4.30) | 0.008 | 2.14 (0.65–7.37) | 0.225 |
| Cardiogenic shock | 14.56 (6.45–32.89) | 0.0001 | 2.74 (0.64–11.76) | 0.174 |
| Circulatory support | 10.01 (4.94–20.54) | 0.0001 | 2.36 (0.71–7.97) | 0.163 |
| Previous coronary artery bypass grafting | 3.35 (1.80–6.25) | 0.0001 | 1.78 (0.87–3.67) | 0.115 |
| Preprocedural British Cardiovascular Intervention Society myocardial jeopardy score | 2.96 (1.71–5.15) | 0.001 | 1.37 (0.65–2.93) | 0.407 |
| Postprocedural British Cardiovascular Intervention Society myocardial jeopardy score | 4.02 (2.41–6.68) | 0.001 | 0.87 (0.34–2.25) | 0.776 |
| BCIS-JS Revascularization Index | 4.13 (1.91–8.91) | 0.0001 | 1.99 (1.03–3.87) | 0.041 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


