Atrial fibrillation (AF) and heart failure (HF) frequently coexist and are associated with an increased mortality. This study evaluated the prognosis of permanent and nonpermanent AF in patients with both AF and HF. All AF patients seen in our institution were identified and followed up. We included 1,906 patients suffering from AF and HF: 839 patients (44%) had preserved left ventricular ejection fraction (LVEF) and 1,067 patients (56%) had decreased LVEF; 1,056 patients (55%) had nonpermanent AF and 850 patients (45%) had permanent AF. During a median follow-up of 1.9 years (interquartile range 0.3 to 5.0), 377 patients died, 462 were readmitted for HF, and 200 had stroke or thromboembolic events. In patients with decreased LVEF, the rate of death was similar in patients with permanent or nonpermanent AF. In patients with preserved LVEF, permanent AF was associated with a higher risk of death and a higher risk of HF hospitalization. Stroke risk did not differ with permanent AF whatever the LVEF. NYHA functional class was an independent predictor of death (risk ratio [RR] = 1.33, 95% confidence interval [CI] 1.12 to 1.59, p = 0.001), as was permanent AF (RR = 1.79, 95%CI 1.32 to 2.42, p = 0.0002). Permanent AF (RR = 1.52, 95% CI 1.20 to 1.93, p = 0.0006) was also an independent predictor of readmission for HF. In conclusion, in patients with AF and HF, the risk of admission for HF and risk of death were higher when AF was permanent, particularly in patients with preserved LVEF. Stroke risk did not differ according to the pattern of AF, whatever the LVEF.
Heart failure (HF) and atrial fibrillation (AF) frequently coexist and are a significant health problem in an increasingly aging population. They are associated with an increased mortality and are responsible for many hospital admissions. AF increases the risk of thromboembolic complications (particularly stroke) and may lead to worsening of symptoms. Whether AF is an independent predictor of mortality is less certain, as is whether it can cause systolic HF (tachycardiomyopathy). In the EuroHeart Failure Survey II, 34% of patients hospitalized for acute HF had a preserved left ventricular ejection fraction (LVEF; ≥45%). Some information are available on the prognosis of AF in HF with reduced LVEF, but there are only few data regarding AF in HF with preserved LVEF. In addition, mortality may be different with different types of AF in the general population and in HF population. Permanent AF seems to be associated with higher mortality than paroxysmal AF. The aim of this study was to evaluate the prognosis of permanent and nonpermanent AF in patients with AF and HF with or without preserved LVEF, in a large cohort of patients with AF.
Methods
Patients hospitalized in the Cardiology Department in our institution (academic hospital, tertiary referral center) with diagnosis of both AF and HF at baseline between January 2000 and December 2010 were retrospectively identified and followed up until December 2010. AF was designated at baseline as nonpermanent if patients had paroxysmal AF or persistent AF. AF was designated as paroxysmal if the arrhythmia terminated spontaneously within 7 days and persistent when the arrhythmia was sustained beyond 7 days, or required termination by cardioversion. Permanent AF was defined at baseline as longstanding AF in which cardioversion has failed or has not been attempted.
The patients were identified by a search in the hospital discharge records, which include information on type of AF, primary diagnoses and coexisting conditions (based on the International Classification of Diseases, of the Word Health Organization), performed procedures, and medication at discharge. The study cohort was represented by all patients consecutively discharged with a primary or secondary diagnosis of AF and HF. Clinical evaluation included determination of the New York Heart Association (NYHA) functional class of HF and European Heart Rhythm Association (EHRA) score of AF-related symptoms. For each patient, we calculated the congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, previous stroke, vascular disease, age 65 to 74 years, and sex category (CHA 2 DS 2 -VASc) risk scores for thromboembolic events and the hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly, drugs or alcohol concomitantly (HAS-BLED) bleeding risk score. We retrieved for each patient the LVEF measured in the 6 previous months with either echocardiography or angioscintigraphy. A minimum ejection fraction of 50%, estimated by echocardiography or angiography, was used to define preserved LVEF. When available, the plasma brain natriuretic peptide (BNP) concentrations were measured with an immunoassay kit provided by Alere Triage (San Diego, California) on Access 2 (Beckman Coulter, Brea, California) automate.
Information on hospital death was obtained on hospital records of our public institution, which includes four hospitals on four different sites and covers all specialties in medicine and surgery. The Center Hospitalier Regional et Universitaire de Tours serves approximately 400,000 inhabitants and is the only public institution in an area of around 4,000 km². Hospital admission for worsening HF, stroke, and thromboembolic events during follow-up was identified by searching in the hospital records, and first date of event was considered in case of multiple hospitalizations.
The characteristics of the patients are reported as percentages and mean ± SD. Comparisons between groups were made using chi-square tests for comparing categorical variables and the Student t or nonparametric Kruskal Wallis test where appropriate for continuous variables. To identify independent characteristics associated with death during follow-up, a Cox regression model was used. Potential confounders were analyzed in univariate analysis and were entered into the model in the multivariate analysis for adjustment. The results are expressed as odds ratios and 95% confidence intervals (CIs). A p value <0.05 was considered statistically significant. Statview 5.0 (Abacus Concepts, Berkeley, California) was used for statistical analysis.
Results
In a cohort of 1,906 patients with AF and HF at baseline, 839 patients had LVEF ≥50% (486 patients with nonpermanent AF and 353 patients with permanent AF) and 1,067 patients had LVEF <50% (570 patients with nonpermanent AF and 497 patients with permanent AF). Baseline characteristics of the entire cohort and the two subgroups of patients are listed in Table 1 . Patients with LVEF ≥50% were more frequently women and hypertensive and less likely to have coronary artery disease and to receive conventional HF therapies. Patients with nonpermanent AF were younger, more likely to be women, hypertensive, more frequently had dyslipidemia, and less likely to have mitral regurgitation. NYHA HF functional class, LVEF, and BNP concentration were not significantly different between patients with nonpermanent AF and permanent AF. The CHA 2 DS 2 -VASc score and HAS-BLED score were also similar in the two groups, but patients with permanent AF were more often treated with anticoagulation and HF therapy than those with nonpermanent AF. Patients with permanent AF were more frequently treated with digoxin and less frequently treated with amiodarone.
| Variable | All Patients, n = 1,906 | Nonpermanent AF, n = 1,056 | Permanent AF, n = 850 | p Value |
|---|---|---|---|---|
| Age (yrs) | 72.8 ± 12.7 | 72.0 ± 12.7 | 73.9 ± 11.3 | 0.0006 |
| Women | 718 (38) | 425 (40) | 293 (35) | 0.01 |
| NYHA HF functional class | 2.2 ± 0.8 | 2.1 ± 0.9 | 2.2 ± 0.9 | 0.06 |
| AF-related symptoms EHRA score | 2.3 ± 0.8 | 2.2 ± 0.8 | 2.3 ± 0.8 | 0.21 |
| LVEF | 47.2 ± 15.9 | 47.2 ± 16.2 | 46.9 ± 15.6 | 0.63 |
| BNP (n = 1,077) | 429 (217–896) | 444 (215–927) | 414 (219–875) | 0.34 |
| Co-morbidities | ||||
| Hypertension | 942 (49) | 558 (53) | 384 (45) | 0.0009 |
| Smoking | 339 (18) | 202 (19) | 137 (16) | 0.09 |
| Peripheral arterial disease | 834 (44) | 468 (44) | 366 (43) | 0.58 |
| Renal insufficiency | 344 (18) | 201 (19) | 143 (17) | 0.21 |
| Dyslipidemia | 483 (53) | 303 (29) | 180 (21) | 0.0002 |
| Diabetes mellitus | 436 (23) | 239 (23) | 197 (23) | 0.78 |
| Thyroid disease | 235 (12) | 127 (12) | 108 (13) | 0.65 |
| Alcohol abuse | 133 (7) | 72 (7) | 61 (7) | 0.76 |
| Valvular surgery | 226 (12) | 103 (8) | 123 (14) | 0.002 |
| Valvular disease | 745 (39) | 296 (28) | 277 (33) | 0.03 |
| Previous ischemic stroke | 139 (7) | 83 (8) | 56 (7) | 0.29 |
| Mitral stenosis | 80 (4) | 30 (3) | 50 (6) | 0.001 |
| Coronary artery disease | 759 (40) | 430 (41) | 329 (39) | 0.37 |
| Pacemaker or ICD | 470 (25) | 244 (23) | 226 (27) | 0.08 |
| Cardiac resynchronization therapy | 141 (7) | 70 (7) | 71 (8) | 0.15 |
| Antithrombotic agent | ||||
| Vitamin K antagonist | 1,138 (64) | 583 (59) | 555 (70) | <0.0001 |
| Antiplatelet agent | 598 (34) | 362 (38) | 236 (30) | 0.002 |
| Other therapy | ||||
| Angiotensin-converting enzyme inhibitor | 861 (55) | 462 (52) | 399 (58) | 0.04 |
| β blocker | 817 (53) | 465 (53) | 352 (51) | 0.47 |
| Digoxin | 539 (34) | 230 (26) | 309 (45) | <0.0001 |
| Diuretic | 1,002 (65) | 509 (59) | 493 (73) | <0.0001 |
| Rhythm control strategy | 811 (50) | 551 (60) | 0 (0) | <0.0001 |
| Amiodarone | 739 (46) | 500 (55) | 239 (34) | <0.0001 |
| Calcium channel blocker | 137 (18) | 81 (19) | 56 (17) | 0.39 |
| Score | ||||
| CHA 2 DS 2 -VASc | 3.8 ± 1.6 | 4.0 ± 1.6 | 3.9 ± 1.6 | 0.44 |
| HAS-BLED score | 1.9 ± 1.1 | 1.9 ± 1.3 | 1.9 ± 1.3 | 0.16 |
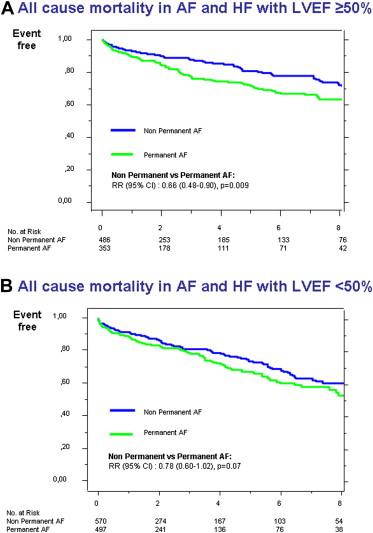
During a median follow-up of 1.9 years (interquartile range 0.3 to 5.0), 377 patients (20%) died, and the yearly rate of death was 7%. Permanent AF was associated with a higher risk of death. The risk of death differed significantly with permanent AF in subgroup of patients with LVEF ≥50% but not in the subgroup of patients with LVEF <50%. The rate of death in patients with LVEF ≥50% was lower in patients with nonpermanent AF than in patients with permanent AF, with a relative risk of 0.66 ( Figure 1 ). Factors associated with an increased risk of death in univariate and multivariate analyses are listed in Table 2 . In multivariate analysis, older age, higher NYHA functional class, permanent AF, and lack of therapy with warfarin and angiotensin-converting enzyme inhibitors were significantly associated with a worse prognosis.
| Death | Univariate, RR (95% CI) | Analysis, p | Multivariate, RR (95% CI) | Analysis, p |
|---|---|---|---|---|
| Age (yrs) | 1.05 (1.04–1.07) | <0.0001 | 1.04 (1.01–1.08) | 0.006 |
| Women | 1.08 (0.88–1.33) | 0.48 | 0.72 (0.42–1.26) | 0.25 |
| NYHA functional class | 1.38 (1.19–1.59) | <0.0001 | 1.33 (1.12–1.59) | 0.001 |
| LVEF <50% | 1.28 (1.04–1.57) | 0.02 | 1.30 (0.95–1.78) | 0.10 |
| Permanent AF | 1.40 (1.14–1.71) | 0.001 | 1.79 (1.32–2.42) | 0.0002 |
| Hypertension | 0.87 (0.71–1.07) | 0.18 | 0.65 (0.36–1.18) | 0.16 |
| Smoking | 1.10 (0.86–1.40) | 0.44 | 1.02 (0.70–1.42) | 0.99 |
| Pulmonary disease | 1.17 (0.92–1.49) | 0.19 | 1.31 (0.88–1.95) | 0.19 |
| Peripheral arterial disease | 1.32 (1.08–1.62) | 0.007 | 1.19 (0.51–2.79) | 0.68 |
| Renal insufficiency | 1.78 (1.42–2.23) | <0.0001 | 1.44 (0.85–2.45) | 0.18 |
| Dyslipidemia | 0.72 (0.57–0.91) | 0.007 | 0.93 (0.64–1.35) | 0.71 |
| Diabetes mellitus | 0.92 (0.72–1.17) | 0.49 | 0.86 (0.49–1.51) | 0.60 |
| Thyroid disease | 0.77 (0.52–1.14) | 0.20 | 1.04 (0.67–1.61) | 0.85 |
| Alcohol abuse | 0.78 (0.53–1.17) | 0.23 | 0.81 (0.39–1.69) | 0.57 |
| Valvular disease | 0.97 (0.78–1.21) | 0.81 | 0.68 (0.43–1.08) | 0.10 |
| Previous ischemic stroke | 1.18 (0.84–1.68) | 0.34 | 0.62 (0.23–1.68) | 0.34 |
| Coronary artery disease | 1.23 (1.00–1.50) | 0.05 | 0.78 (0.38–1.61) | 0.50 |
| Pacemaker or ICD | 0.78 (0.62–0.98) | 0.03 | 0.86 (0.62–1.20) | 0.38 |
| Previous bleeding | 1.88 (1.34–2.65) | 0.0003 | 1.48 (0.77–2.84) | 0.24 |
| Labile INR | 0.86 (0.52–1.43) | 0.57 | 0.82 (0.36–1.89) | 0.64 |
| Antiplatelet agent | 1.35 (1.08–1.68) | 0.007 | 0.84 (0.54–1.30) | 0.44 |
| Vitamin K antagonist | 0.56 (0.45–0.69) | <0.0001 | 0.63 (0.45–0.88) | 0.008 |
| Angiotensin-converting enzyme inhibitor; | 0.98 (0.79–1.23) | 0.89 | 0.68 (0.49–0.93) | 0.02 |
| β blocker | 0.71 (0.56–0.89) | 0.003 | 0.74 (0.54–1.02) | 0.07 |
| Digoxin | 0.88 (0.70–1.11) | 0.29 | 0.83 (0.60–1.15) | 0.26 |
| Diuretic | 1.30 (1.02–1.66) | 0.03 | 1.27 (0.90–1.80) | 0.18 |
During follow-up, 200 patients had stroke or thromboembolic (TE). Factors associated with an increased risk of stroke/TE in univariate and multivariate analyses are listed in Table 3 . Permanent AF was not significantly associated with a higher risk of stroke or TE, neither in patients with LVEF <50% nor in patients with LVEF ≥50% ( Figure 2 ).
| Stroke/Thromboembolic Events | Univariate, RR (95% CI) | Analysis, p | Multivariate, RR (95% CI) | Analysis, p |
|---|---|---|---|---|
| Age (yrs) | 1.03 (1.02–1.05) | <0.0001 | 1.01 (0.97–1.05) | 0.55 |
| Women | 1.41 (1.07–1.86) | 0.02 | 0.77 (0.37–1.59) | 0.48 |
| NYHA functional class | 0.93 (0.77–1.13) | 0.49 | 0.94 (0.75–1.19) | 0.62 |
| LVEF <50% | 1.02 (0.74–1.40) | 0.92 | 1.27 (0.82–1.97) | 0.29 |
| Permanent AF | 1.02 (0.77–1.34) | 0.91 | 1.17 (0.77–1.78) | 0.47 |
| Hypertension | 1.19 (0.90–1.58) | 0.21 | 1.24 (0.56–2.75) | 0.59 |
| Smoking | 0.92 (0.64–1.30) | 0.63 | 0.94 (0.56–1.59) | 0.83 |
| Pulmonary disease | 1.03 (0.73–1.45) | 0.88 | 0.68 (0.37–1.26) | 0.22 |
| Peripheral arterial disease | 1.30 (0.98–1.72) | 0.06 | 2.27 (0.88–5.88) | 0.09 |
| Renal insufficiency | 1.44 (1.03–2.00) | 0.03 | 2.24 (1.07–4.69) | 0.03 |
| Dyslipidemia | 0.80 (0.58–1.10) | 0.18 | 1.06 (0.65–1.72) | 0.82 |
| Diabetes mellitus | 1.12 (0.81–1.55) | 0.48 | 0.73 (0.35–1.52) | 0.40 |
| Thyroid disease | 0.99 (0.61–1.60) | 0.96 | 1.11 (0.65–1.89) | 0.70 |
| Alcohol abuse | 0.76 (0.43–1.33) | 0.33 | 2.22 (0.86–5.75) | 0.10 |
| Valvular disease | 0.96 (0.71–1.29) | 0.77 | 0.52 (0.26–1.04) | 0.06 |
| Previous ischemic stroke | 4.15 (2.98–5.75) | <0.0001 | 3.06 (0.96–9.80) | 0.06 |
| Coronary artery disease | 1.07 (0.81–1.42) | 0.64 | 0.37 (0.17–0.81) | 0.01 |
| Pacemaker or ICD | 0.87 (0.64–1.18) | 0.38 | 0.87 (0.55–1.36) | 0.53 |
| Previous bleeding | 2.16 (1.38–3.37) | 0.0007 | 3.07 (1.33–7.09) | 0.009 |
| Labile INR | 0.78 (0.43–1.39) | 0.39 | 3.80 (1.54–9.35) | 0.003 |
| Antiplatelet agent | 1.75 (1.31–2.35) | 0.0002 | 1.92 (1.06–3.47) | 0.03 |
| Vitamin K antagonist | 0.80 (0.59–1.07) | 0.13 | 1.22 (0.73–2.04) | 0.44 |
| Angiotensin-converting enzyme inhibitor | 1.18 (0.87–1.62) | 0.29 | 0.97 (0.63–1.49) | 0.89 |
| β blocker | 1.05 (0.77–1.43) | 0.77 | 1.00 (0.64–1.56) | 0.99 |
| Digoxin | 0.88 (0.64–1.22) | 0.44 | 0.72 (0.46–1.12) | 0.14 |
| Diuretic | 1.22 (0.88–1.69) | 0.24 | 1.00 (0.63–1.58) | 0.99 |
During follow-up, 462 patients were readmitted for HF. Permanent AF was associated with a higher risk of readmission for HF. The rate of hospital readmission for worsening HF in patients with LVEF ≥50% was lower in patients with nonpermanent AF than in patients with permanent AF ( Figure 3 ) Permanent AF, pulmonary disease, valvular disease, use of βblocker, and diuretic were independently associated with a higher risk of readmission for HF ( Table 4 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


