Procedures to Treat Arrhythmias in the Cardiac Care Unit
Eric M. Bader
Edgar Argulian
Eyal Herzog
Emad F. Aziz
Cardiac arrhythmias are among the most common conditions encountered in the cardiac care unit (CCU). The confluence of technology, personnel, and expertise that the CCU provides makes it the ideal location to address these challenging states. Essential to the care of the critically ill cardiac patient is the constant monitoring of the patient’s rhythm and vital signs, including blood pressure, respiration, and oxygenation. Symptomatic cardiac arrhythmias can be divided into bradycardias, where the native heart rate is insufficient to maintain an adequate cardiac output, and tachycardias, where the heart rate is accelerated or disorganized to the degree that the heart no longer functions as an effective pump. Either of these conditions can manifest clinically as heart failure, chest pain, dyspnea, dizziness or altered state of consciousness, hypotension, and pulmonary or peripheral edema.
The bradyarrhythmias include sinus bradycardia when, due to extrinsic or intrinsic reasons, the sinus node is chronotropically impaired. In other instances, the sinus node is intact, but there is a clinically significant interruption in the intracardiac conduction pathways. These include high-grade second-degree heart block (Mobitz type II) as well as third-degree (complete) heart block. Lower grade heart blocks, such as second-degree Mobitz type I (Wenckebach) and bundle branch blocks typically do not require acute intervention. Tachyarrhythmias can be divided into supraventricular and ventricular tachycardias (SVTs and VTs). SVTs are described in Chapter 16 and include atrial tachycardia, atrial fibrillation, and atrial flutter. VTs range from premature ventricular complexes, which typically do not require intervention, to ventricular fibrillation (VF), which is a medical emergency.
Many of the procedures to treat arrhythmias in the CCU require sedation that ensures patient comfort and can impact the success of the procedure. The desired degree of sedation, known as procedural or conscious sedation, should be provided by a health care practitioner who is certified in conscious sedation. Choice of medication should include careful consideration of the medication’s side effects, time of onset, and half-life.
MANAGEMENT OF BRADYCARDIA WITH TEMPORARY PACING
Bradycardia in the critically ill patient becomes clinically significant when the cardiac output, as determined by the heart rate and the stroke volume, falls below that required to meet the body’s metabolic demand. Once this occurs, temporary pacing may be required to increase the heart rate and correspondingly the patient’s cardiac output. Temporary pacing is considered a temporizing measure until the patient recovers from the acute insult or is able to have a permanent pacemaker implanted. Temporary pacing can be carried out through a transcutaneous pacing or by means of temporary pacing wires.
TRANSCUTANEOUS PACING
Transcutaneous pacing1 utilizes large cutaneous pads that pace the heart in a noninvasive manner. These pads are composed of an adhesive backing and a metallic plate, which is faced with a saline-based conductive gel. This method of pacing has the advantage of its ease of application and availability as a backup.
The noninvasive nature of this modality reduces the risk of complications associated with the more invasive pacing methods.2 This is achieved, however, at the expense of patient comfort and a lower rate of capture. When properly applied, capture rates of up to 90% can be expected in the range of output typically provided by today’s external defibrillator/pacing units. This electrical current, however, can also lead to painful stimulation of chest wall skeletal muscle requiring significant levels of analgesia and sedation for prolonged pacing durations.
Preprocedure preparation: The following are required:
External defibrillator/pacer unit
Pacer pads
Adequate sedation and analgesia.
Procedure: The pads should be placed according to the individual manufacturer’s instructions. Successful capture of external pacing impulses is dependent on proper placement of the pacing pads.3 The choice of electrical output, typically between 10 and 200 mA, depends on the energy required for myocardial electrical capture. Unlike transvenous pacing, the EKG is not helpful in determining capture in transcutaneously paced patients, as the artifact from the long-duration pacing impulse can obscure the EKG. Instead, capture is determined by manual palpation of the pulse and other hemodynamic measurement.
Postprocedure: Continuous monitoring is essential to confirm continued capture, as well as to assess the patient’s respiratory rate, level of sedation, and pain. At this time, serious consideration should be given to the next step in the treatment plan, including temporary and permanent transvenous pacing.
TEMPORARY TRANSVENOUS PACING
Transvenous pacing is an effective method for augmenting heart rate.4,5 This method of pacing is more reliable than transcutaneous pacing but is not immune from problems like catheter migration, bleeding, infection, and perforation of the right ventricular (RV) free wall, which can lead to hemopericardium and tamponade.6
Table 21.1 outlines the class I indications for transvenous pacing.7
TABLE 21.1 Class I Indications for the Placement of Emergent Transvenous Pacemaker | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Preprocedure preparation: The following are required:
12-lead EKG machine
Portable ultrasound
Introducer sheath and central line kit (Figure 21.1)
Sedation: As the level of discomfort experienced during this procedure is not comparable with transcutaneous pacing, sedation is rarely required. It may, however, be helpful at times to administer low doses of anxiolytics to ensure patient comfort.
Pacing wire kit
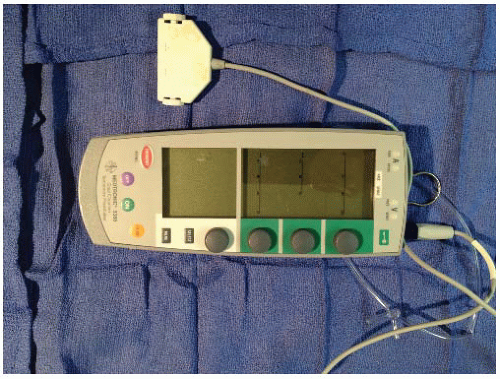
Generator box (Figure 21.2)
Choice of access site: The right internal jugular (IJ) vein when accessed under direct ultrasound visualization is the preferred method of access. This location allows for the greatest combination of safety and long-term stability of the access point, with acceptably low rates of infection and catheter dislodgement. In addition, the use of the right IJ leaves the left subclavian vein available for the placement of a permanent pacing device should that be needed. The right IJ is followed in order of preference by the left subclavian vein, which is a relatively stable location but carries a higher rate of complications like pneumothorax. The right femoral vein is considered the safest access site. It is easily controlled in the event of a problem with the introducer sheath, but it carries the disadvantage of the highest rate of site infection and catheter dislodgment. It is advised to obtain an access in advance as temporary pacing may be required emergently. It is prudent in patients in whom you suspect that an emergency condition may require pacing support to place the introducer sheath in advance. Care should be exercised to ensure that the hub of the sheath remains sterile.
Procedure: Once the access site is chosen, the patient is prepped in a sterile fashion. A large drape should be used to provide an adequate sterile field.
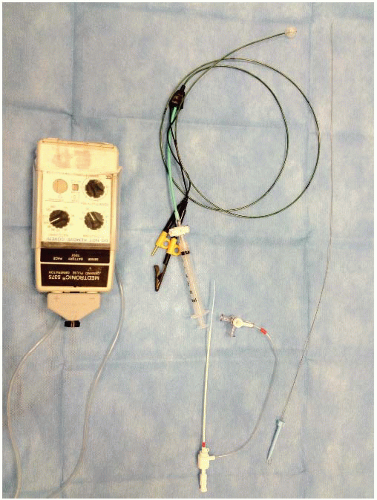 Figure 21.1. Four French introducer and transvenous pacing wire kit. (Note distal balloon inflated with provided syringe.) |
1. IJ venous cannulation8 is guided by three anatomic landmarks: the two heads of the sternocleidomastoid muscle (SCM), the upper margin of the clavicle, and the midclavicular notch. After infiltrating the area with a small gauge needle, the IJ artery is palpated as it runs between the heads of the SCM. The artery is retracted medially, and if a sterile “site-finder” is available, the vein is accessed with an 18G needle at a 30° angle with the needle pointed toward the ipsilateral nipple. If no ultrasound
guidance is available, venous access is first achieved with a small finder needle and then repeated with a larger needle through which a J-tipped guidewire is advanced. The guidewire should then be advanced to about 20 cm with careful attention given to the cardiac monitor for ventricular ectopy. Should ventricular ectopic beats occur, the guidewire should be promptly withdrawn until the ectopy ceases. The dilator and sheath are then advanced over the wire. After placement of the sheath, the dilator and the guidewire are removed, blood is drawn out of the side port, and the sheath is flushed and sutured in place.
guidance is available, venous access is first achieved with a small finder needle and then repeated with a larger needle through which a J-tipped guidewire is advanced. The guidewire should then be advanced to about 20 cm with careful attention given to the cardiac monitor for ventricular ectopy. Should ventricular ectopic beats occur, the guidewire should be promptly withdrawn until the ectopy ceases. The dilator and sheath are then advanced over the wire. After placement of the sheath, the dilator and the guidewire are removed, blood is drawn out of the side port, and the sheath is flushed and sutured in place.
2. Subclavian access9




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree