25 Prevention and Management of Procedural Complications
 Choice of Physician
Choice of Physician
A primary issue regarding morbidity associated with CIED implantation is which medical professional should implant and follow up in these patients. As the indications for CIEDs have broadened, and an increasing number of patients are considered for implantation, physicians of various specialties are being called on to implant the devices and manage the postimplantation care of these patients. Curtis et al.,1 using data from the National Cardiovascular Device ICD Registry, found that the rates of overall complications and major complications were lowest among procedures carried out by electrophysiologist (EP) physicians (3.5% and 1.3%, respectively) and highest among those performed by thoracic surgeons (5.8% and 2.5%). Importantly, EP physicians had the lowest rates of major complications, including cardiac arrest, lead dislodgment, and pneumothorax. In this study, the choice of device was also influenced by the specialty of the physician performing the procedure. Non–EP physicians failed to recommend implantation of an indicated cardiac resynchronization implantable cardioverter-defibrillator (ICD) device (CRT-D).1 In a different study, Al-Khatib et al.2 also identified implantation by non–EP physicians as being associated with an increased incidence of complications.2
 Implantation-Related Complications
Implantation-Related Complications
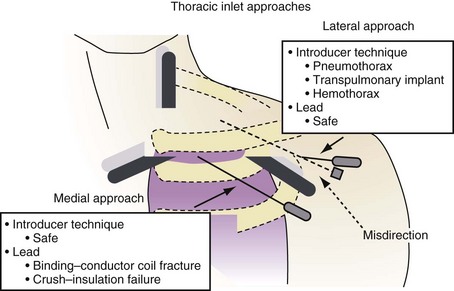
Depending on the physical characteristics of the lead, in terms of both materials and construction, certain approaches to subclavian vein access have been associated with subclavian crush, where the lead is compressed in the space between the clavicle and the first rib. This entrapment of the lead in the subclavius muscle, in the periosteum of the clavicle, or just through the very narrow space that occurs with medial subclavian vein puncture is completely dependent on the proceduralist’s approach to accessing the central circulation. In addition, management of suture tie-down sleeves with overly tight ligatures can damage the outer insulation, inner insulation, or conductor coils, particularly in coaxial leads with a polyurethane inner insulation.3,4
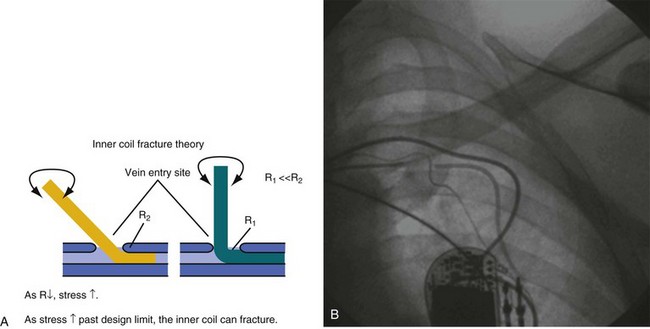
In response to the concerns about medial access of the subclavian system, physicians began to use more lateral access techniques. Unfortunately, extreme lateral access places different stresses on the lead body. Recently popularized implantation techniques within the last 10 years employ access to the subclavian venous system at the point where the axillary vein crosses the first rib, immediately lateral to the clavicle. However, if a more lateral approach into the axillary vein over the second or third rib stresses the leads by a different mechanism. The extreme angle of the lead on entry to the axillary vein at this lateral but also more posterior position, as well as the resultant acute anterior bend following the trajectory of the vein, exacerbated by the suture tie-down sleeve fixing the lead to the muscle, places a torque and compression fatigue stress on the lead conductors. This is most often observed with leads constructed with a thin body, coaxial construction, and active-fixation inner coils (Figs. 25-1 and 25-2).
The more medial axillary vein puncture, over the first anterior rib, avoids both subclavian crush and second-rib fatigue fractures.5 The axillary vein can be accessed under fluoroscopy over the first rib and the area probed posterolaterally until the vein is punctured. Alternatively, venography or ultrasound can be used to guide lead implantation6 (see Chapter 21).
At implantation, the lead must be treated gently, and any mechanical stress should be avoided. Even overuse of the helical screw mechanism can place additional stress on the conductor. It is usually difficult to nail down the precise trauma that later causes a lead failure, but the time of implantation is a relatively dangerous time for a lead and is often a contributor to the ultimate failure. Prolapsing of the lead on itself should not be performed unless absolutely necessary. Again, although difficult to prove, this practice has been implicated in early lead failure, particularly with lower-profile ICD leads.7–12
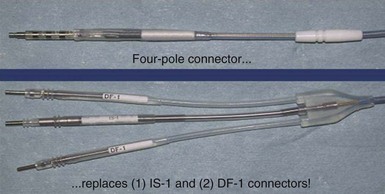
In addition to placing the lead in the heart and affixing the suture sleeve, making the connections to the CIED is another potential problem. Utmost vigilance should be exercised when the leads are connected to the device, to avoid the need for surgical revision, reentering the pocket and increasing the risk of infection. In the Replace trial, five patients needed revision because of generator-lead interface problem, such as loose set screw or misconnected leads.13 With the introduction of the DF-4 ICD leads, in which the two DF-1 and one IS-1 connectors are replaced with a single connector, the incidence of connection error should be significantly reduced.14 Currently, an SJ-4 lead is available and is in clinical use (Fig. 25-3).
 Procedural Complications
Procedural Complications
Lead Dislodgment
Lead dislodgment is the most common complication associated with CIEDs (1.6%-4.4% of cases), with atrial lead dislodgment accounting for most cases. In the MOST trial of more than 2000 patients, Ellenbogen et al.15 found atrial dislodgment in 1.7% of patients in the first 30 postimplant days.15 To prevent dislodgment, it is important to have an adequate intrinsic signal and to ensure contact to the myocardial wall. This is partly assessed by viewing a modest current of injury in the unfiltered electrogram, in addition to the appearance on fluoroscopy. This has the appearance of a QRS complex with ST-segment elevation before fixation of the active helix into the myocardium. Appropriate slack on the lead is also important, to allow for settling of the device when the patient is upright. There may be micro- or macro-dislodgment. Micro-dislodgment has been defined as when there is loss of capture and sensing without radiographic evidence of dislodgment. Macro-dislodgment can be detected by radiography. Lead dislodgment requires reopening the pocket and repositioning of the dislodged lead to ascertain satisfactory function. However, it is best to reaccess the vein, remove the dislodged lead, and ensure that there is no clot or tissue or damage to the lead before reinsertion.
Pneumothorax
Inadvertent entrance into the pleural space, especially with the introducer access technique, can lead to pneumothorax (0.7%-2% of cases).1,2 This is related to the experience of the implanter and also the level of difficulty obtaining access. This complication can be mitigated by using an extrathoracic approach with the introducer technique, accessing the axillary vein over the first rib, which acts as a barrier against entering the lung. Pneumothorax should not occur when using the cephalic vein cutdown technique. Most patients with pneumothorax are asymptomatic and are diagnosed on the postimplant chest radiograph. In patients with a sizable pneumothorax, cardiothoracic surgery should be consulted for possible chest tube insertion, in addition to administering high-flow oxygen. Tension pneumothorax should be recognized as a potential cause of sudden hemodynamic compromise during device implantation. Tension pneumothorax should be treated immediately with a chest tube.
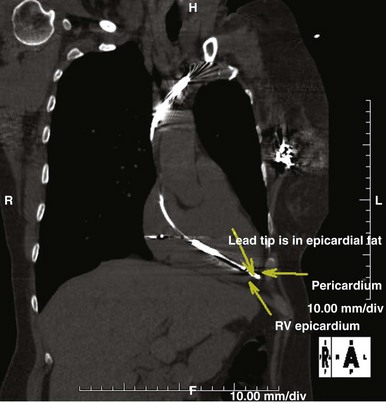
Perforation
Perforation of the great vessels is very rare during implantation and is more common with lead extraction. Ventricular perforation is rare and reported to occur in 0.3% to 1% of CIED cases7,11,16,17 (Fig. 25-4). Most are self-limited with no sequelae. Acute tamponade is extremely rare but should be quickly recognized as a cause of hemodynamic compromise and easily diagnosed by bedside echocardiography or with fluoroscopy; the enlarged cardiac silhouette is associated with minimal contraction. Immediate pericardiocentesis should be performed and surgical intervention sought if bleeding does not stop.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree