The risk factors for aortic and mitral valve diseases that require surgical repair such as congenital bicuspid aortic valve (BAV) and mitral valve prolapse include acquired clinical factors and genetic influences. Whether race affects the prevalence of certain valvular diseases has not been sufficiently investigated. Through the Cleveland Clinic’s Cardiovascular Information Registry, we evaluated the data from 40,419 patients who had undergone aortic valve surgery, mitral valve surgery, and/or coronary artery bypass grafting from 1993 to 2007. Of these patients, 38,366 were white and 2,053 were black. The prospective evaluation of valvular disease was coded, identifying the etiology and morphology by echocardiographic, surgical, and pathologic inspection. At baseline, compared to white patients, the black patients were younger, more often women, had a greater body mass index, and a greater prevalence of hypertension, diabetes, tobacco use, and renal disease. The prevalence of congenital BAV and mitral valve prolapse was considerably lower in blacks than in whites (9% vs 25%, p <0.001, and 27% vs 52%, p <0.001, respectively), as was the presence of calcific aortic stenosis (14% vs 28%; p <0.001), pathologically determined aortic valve calcium (50% vs 67%; p <0.001), and mitral valve chordal rupture (13% vs 31%; p <0.001). In conclusion, in the present large surgical series, the valve etiologies and morphology differed among blacks and whites. Despite an adverse cardiovascular risk profile, blacks had a significantly lower prevalence of valvular calcium and degeneration than did the whites and a lower prevalence of congenital BAV and mitral valve prolapse. Our findings offer insight into the influence of race on the development of mitral valve disease and congenital BAV.
The influence of race on specific valvular heart diseases has been understudied. From an autopsy series and echocardiographic database reviews, it has been suggested that blacks have a lower prevalence of bicuspid aortic valve (BAV). Racial differences have been observed in the prevalence of aortic and mitral valve calcium, with blacks having a lower risk of extracoronary calcium. Whether the prevalence of mitral valve prolapse (MVP) differs by race has been studied previously but, more recently, has been limited to populations of South Asian, European, and Chinese descent. Using data from a large institutional surgical database, we sought to determine the association between white and black race and the prevalence of MVP and BAV among patients undergoing mitral valve surgery, aortic valve surgery, and/or coronary artery bypass grafting (CABG).
Methods
The study patients were identified using the Cardiovascular Information Registry of the Cleveland Clinic (Cleveland, Ohio), a single-center, prospective database containing baseline clinical and laboratory information for consecutive patients undergoing cardiac surgery. From January 1, 1993 to January 1, 2007, 43,496 patients underwent aortic valve surgery, mitral valve surgery, and/or CABG at the Cleveland Clinic (Cleveland, Ohio). Of these patients, 38,366 were white and 2,053 were black; these patients constituted the study population (2,559 patients of other races were excluded). Of the 40,419 study patients, 12,714 patients had undergone aortic valve surgery (12,182 whites, 532 blacks), 12,779 mitral valve surgery (12,164 whites, 615 blacks), and 14,926 isolated CABG. The baseline clinical, laboratory, and surgical data were prospectively collected in the registry. The baseline characteristics of all patients were obtained from the registry and included the following: age, gender, race (self-reported by the patient), body mass index, current therapy for diabetes mellitus, current therapy for and/or a history of hypertension, current tobacco use, a history of renal disease, a history of peripheral vascular disease, a history of myocardial infarction, and a history of chronic lung disease. The baseline laboratory data for patients were obtained from the registry and included the following: serum creatinine, total cholesterol, and high- and low-density lipoprotein cholesterol. The institutional review board at Cleveland Clinic (Cleveland, Ohio) approved the present study.
The indication for valve surgery was prospectively coded in the registry at surgery according to the hemodynamic, cine radiographic, and/or echocardiographic data, performed at either the Cleveland Clinic or an outside institution. The predominant valve lesion was coded in the registry as stenosis, regurgitation, or mixed. Morphologic evaluation of the valve structure and etiology was done from the echocardiographic data and, when available, direct gross inspection by the operating surgeon. Pathologic findings were from gross examination and histologic analysis of the explanted valvular specimens. For the aortic valve, degenerative disease was classified as an abnormal trileaflet valve (fibrosis, calcium, thickening, nonspecific degenerative changes) without rheumatic changes, infective endocarditis, an associated aneurysm, or congenital abnormalities, including a BAV. For the mitral valve, degenerative disease was classified as an abnormal valve without ischemic, congenital, rheumatic, or infective endocarditis changes. These valves typically had isolated myxomatous degeneration such as prolapse or chordal rupture.
Continuous data are expressed as the mean ± SD, with the median, 15th and 85th percentiles (comparable to 1 SD). Wilcoxon rank sum tests were used to analyze race differences for the continuous data. Categorical data are presented as frequencies and percentages, and race comparisons were done using the chi-square test (Fisher’s exact test, if appropriate). Statistical analyses were performed using SAS, version 9.1 (SAS Institute, Cary, North Carolina).
Results
On average, the black patients were younger, more likely to be women, and had a greater weight and body mass index than the white patients ( Table 1 ). The black patients had a greater prevalence of hypertension, diabetes mellitus, renal disease, tobacco use, and previous myocardial infarction. Compared to the white patients, the black patients had a greater serum creatinine, lower total cholesterol, and greater high-density lipoprotein levels. The black patients were more likely to undergo CABG during their index surgery.
| Variable | Whites (n = 38,366) | Blacks (n = 2,053) | p Value |
|---|---|---|---|
| Age (yrs) | 64 ± 13 | 61 ± 13 | <0.001 |
| Male gender | 69% | 55% | <0.001 |
| Weight (kg) | 82 ± 18 | 84 ± 19 | <0.001 |
| Body mass index (kg/m 2 ) | 28 ± 5 | 29 ± 6 | <0.001 |
| Hypertension | 66% | 85% | <0.001 |
| Diabetes mellitus | 21% | 31% | <0.001 |
| Renal disease | 5% | 13% | <0.001 |
| Tobacco use | 59% | 69% | <0.001 |
| Previous myocardial infarction | 41% | 49% | <0.001 |
| Chronic obstructive lung disease | 25% | 32% | <0.001 |
| Peripheral vascular disease | 37% | 37% | 0.92 |
| Serum creatinine (mg/dl) | 1.2 ± 0.8 | 1.6 ± 1.8 | <0.001 |
| Total cholesterol (mg/dl) | 190 ± 47 | 187 ± 51 | <0.001 |
| High-density lipoprotein cholesterol (mg/dl) | 46 ± 16 | 49 ± 17 | <0.001 |
| Low-density lipoprotein cholesterol (mg/dl) | 113 ± 41 | 113 ± 47 | 0.66 |
| Triglycerides (mg/dl) | 158 ± 125 | 126 ± 104 | <0.001 |
| Coronary artery bypass grafting during index surgery | 64% | 67% | 0.01 |
| Congenital bicuspid aortic valve | 25% | 9% | <0.001 |
| Mitral valve prolapse, any leaflet | 52% | 27% | <0.001 |
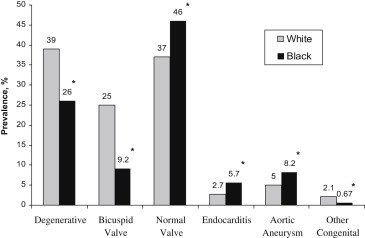
The black patients were less likely than the white patients to present with aortic valve disease of degenerative etiology, a congenital BAV, or other congenital abnormalities and were more likely to have an etiology of endocarditis and ascending aortic dilation or aneurysm or a normal aortic valve ( Figure 1 ). The pathologic findings from the explanted aortic valves revealed less cuspal calcium among the black patients and a greater prevalence of dilated aortic annulus, cusp vegetation, and cusp perforation ( Figure 2 ).