The impact of left ventricular (LV) dyssynchrony on the long-term outcomes of patients with acute myocardial infarction (AMI) remains unknown. The purpose of the present study was to evaluate the prevalence of LV dyssynchrony after AMI and the potential relation with adverse events. A total of 976 consecutive patients admitted with AMI treated with primary percutaneous coronary intervention were evaluated. Two-dimensional echocardiography was performed <48 hours after admission. LV dyssynchrony was assessed with speckle-tracking imaging and calculated as the time difference between the earliest and latest activated segments. Patients were followed up for the occurrence of all-cause mortality (the primary end point) or the composite secondary end point (heart failure hospitalization and all-cause mortality). Within 48 hours of admission for the index infarction, mean LV dyssynchrony was 61 ±79 ms, and 14% of the patients demonstrated a ≥130-ms time difference, defined as significant LV dyssynchrony. During a mean follow-up period of 40 ±17 months, 82 patients (8%) reached the primary end point. In addition, 36 patients (4%) were hospitalized for heart failure. The presence of LV dyssynchrony was associated with an increased risk for all-cause mortality and hospitalization for heart failure during long-term follow-up (adjusted hazard ratio 1.06, 95% confidence interval 1.05 to 1.08, p <0.001, per 10-ms increase). Moreover, LV dyssynchrony provided incremental value over known clinical and echocardiographic risk factors for the prediction of adverse outcomes. In conclusion, LV dyssynchrony is a strong predictor of long-term mortality and hospitalization for heart failure in a population of patients admitted with ST-segment elevation AMI treated with primary percutaneous coronary intervention.
Left ventricular (LV) dyssynchrony has been extensively evaluated in patients with heart failure who undergo cardiac resynchronization therapy. The presence of LV dyssynchrony is significantly associated with increased morbidity and mortality in patients with heart failure. In contrast, reduction of LV dyssynchrony by cardiac resynchronization therapy has been shown to improve the quality of life, LV function, and survival of patients with heart failure.
In the past few years, the prevalence and clinical implications of LV dyssynchrony in other subgroups of patients have been evaluated. Several studies have investigated the predictive value of LV dyssynchrony for the development of LV remodeling after acute myocardial infarction (AMI). More recently, LV dyssynchrony was related to adverse events, including all-cause mortality and heart failure, in high-risk AMI patients with LV dysfunction.
Currently, most patients admitted with AMI are treated with primary percutaneous coronary intervention (PCI), and therefore, LV function is relatively preserved. A few studies have reported the prevalence of LV dyssynchrony in patients with AMI treated with primary PCI. However, the clinical relevance of LV dyssynchrony in patients with AMI treated with primary PCI remains unclear. Accordingly, the purposes of the present study were to assess the prevalence of LV dyssynchrony in a large population of patients with AMI treated with primary PCI and to assess the potential relation between LV dyssynchrony and long-term outcomes.
Methods
A total of 976 consecutive patients admitted with ST-segment elevation AMI treated with primary PCI were evaluated. Patients were selected from an ongoing registry that evaluates the effects of an all-phase integrated AMI care program (MISSION!) on short- and long-term outcomes. Diagnosis of ST-segment elevation AMI was based on typical electrocardiographic changes with clinical symptoms associated with elevation of cardiac biomarkers. All patients were treated according to the institutional AMI protocol (MISSION!), which includes 2-dimensional echocardiography performed <48 hours after admission. Clinical data were prospectively entered in the departmental cardiology information system (EPD-Vision; Leiden University Medical Center, Leiden, The Netherlands) and retrospectively analyzed. In addition, echocardiographic data were retrospectively analyzed, including the assessment of LV dyssynchrony with 2-dimensional speckle-tracking imaging.
Patients were followed prospectively for the occurrence of all-cause mortality and hospitalizations for heart failure. Among the various clinical and echocardiographic variables, the independent determinants of these end points were assessed. In particular, the prognostic value of LV dyssynchrony was evaluated.
All patients underwent imaging in the left lateral decubitus position using a commercially available system (Vivid 7 and e9; GE Vingmed Ultrasound AS, Horten, Norway). Images were obtained, with a simultaneous electrocardiographic signal, using a 3.5-MHz transducer in the parasternal and apical views. Standard M-mode and 2-dimensional images were acquired during breath hold and saved in cine loop format from 3 consecutive beats. Analysis of echocardiographic images was performed offline by 2 independent observers using dedicated software (EchoPAC version 108.1.5; GE Vingmed Ultrasound AS).
LV end-systolic and end-diastolic volumes were assessed, and the LV ejection fraction was calculated using the biplane Simpson’s method. Thereafter, the left ventricle was divided into 16 segments, and each segment was analyzed individually and scored on the basis of its motion and systolic thickening (1 = normokinesia, 2 = hypokinesia, 3 = akinesia, 4 = dyskinesia). Wall motion score index was calculated as the sum of the segment scores divided by the number of segments scored. The severity of mitral regurgitation was graded semiquantitatively from the jet area of color-flow Doppler data and by measuring the width of the vena contracta.
To assess LV diastolic function, pulsed-wave Doppler of mitral valve inflow was obtained by placing the Doppler sample volume between the tips of the mitral leaflets. The early (E) and late (A) peak diastolic velocities and E-wave deceleration time were measured. The E/E′ ratio was obtained by dividing E by E′, which was measured using color-coded tissue Doppler imaging at the septal side of the mitral annulus in the apical 4-chamber view.
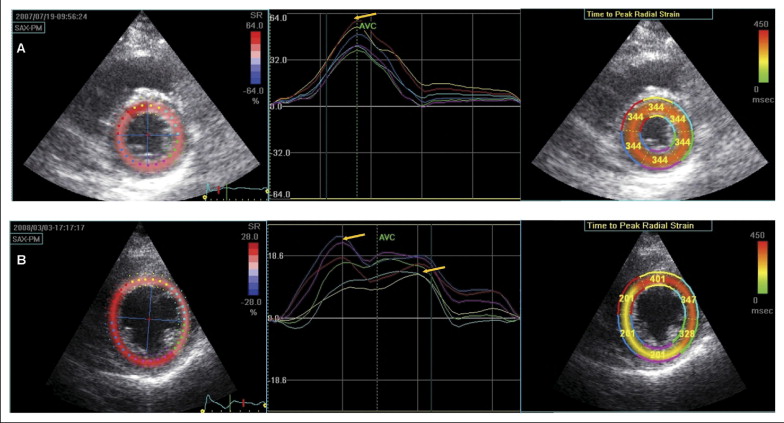
LV dyssynchrony was evaluated using speckle-tracking analysis ( Figure 1 ) . This software analyzes motion by tracking the frame-to-frame movement of natural acoustic markers on standard ultrasonic images in 2 dimensions. All images were recorded with a frame rate of ≥40 frames/s for reliable analysis. To obtain LV dyssynchrony, peak radial strain was assessed on the LV short-axis images at the level of the papillary muscles. The LV endocardial border was manually traced, and the automatically created region of interest was adjusted to the thickness of the myocardium. Thereafter, the traced endocardium was automatically divided into 6 standard segments (septal, anteroseptal, anterior, lateral, posterior, and inferior). Segments were discarded if tracking was of poor quality. Finally, the software automatically provided the time to peak systolic strain for all 6 segments, and LV dyssynchrony was calculated as the time difference between the earliest and latest activated segments. Inter- and intraobserver agreement for LV dyssynchrony assessment was 87%, as previously published.
Continuous data are presented as mean ± SD and categorical data as frequencies and percentages. Differences in characteristics between patient groups were evaluated using unpaired Student’s t tests and chi-square tests. Differences in dyssynchrony between the different groups of the LV ejection fraction were compared using 1-way analysis of variance. Post hoc comparisons were performed using Bonferroni adjustments for multiple comparisons.
All patients were followed prospectively, and the occurrence of adverse events was noted. Patients in whom >1-year follow-up data were lacking were considered lost to follow-up. Data on these patients were included until the last date of follow-up. All-cause mortality was defined as the primary end point. The secondary end point was defined as a composite of all-cause mortality and hospitalization for heart failure. Hospitalization for heart failure was defined as hospitalization for new-onset or worsening of heart failure. Event rates were plotted using Kaplan-Meier curves for primary and secondary end points, and the study population was divided into patients with and without LV dyssynchrony. Patients with LV dyssynchrony were defined as those with time differences ≥130 ms between the earliest and latest activated segments. The cut-off value of 130 ms was derived from previous studies, which have demonstrated that a time difference ≥130 ms is the optimal cut-off value for the prediction of LV remodeling in patients after AMI but also for the prediction of response after cardiac resynchronization therapy. The event rates between patients with and without LV dyssynchrony were compared using the log-rank test.
To assess the relation between LV dyssynchrony and the primary and secondary end points, multivariate Cox proportional-hazards analysis was performed. The selection of parameters for consideration for entry in the multivariate models was based on clinical judgment and univariate statistical significance. The multivariate models were corrected for age, Killip class ≥2, diabetes, QRS duration, the left anterior descending coronary artery as the culprit vessel, multivessel coronary disease, peak cardiac troponin T level, the LV ejection fraction, wall motion score index, and E/E′ ratio.
The incremental value of LV dyssynchrony for the prediction of the primary and secondary end points was evaluated by comparing the areas under the receiver-operating characteristic curves. For this purpose, 2 models were constructed. Model 1 consisted of traditional clinical and echocardiographic risk factors, including age, Killip class ≥2, diabetes, QRS duration, the left anterior descending coronary artery as the culprit vessel, peak cardiac troponin T level, the LV ejection fraction, and E/E′ ratio, and model 2 consisted of model 1 including LV dyssynchrony.
All statistical tests were 2 sided, and p values <0.05 were considered statistically significant. SPSS for Windows version 17 (SPSS, Inc., Chicago, Illinois) was used to perform the statistical analyses.
Results
Baseline clinical and echocardiographic characteristics of the patients are summarized in Tables 1 and 2 . The mean age of the population was 61 ± 12 years, and most patients were men (n = 747 [77%]). The left anterior descending coronary artery was the culprit vessel in 446 patients (46%), and mean peak creatine phosphokinase and peak cardiac troponin T levels were 2,374 ± 3,143 U/L and 6.4 ± 6.7 μg/L, respectively. Baseline echocardiography performed <48 hours after admission revealed relatively preserved LV ejection fractions (47 ± 9%) and moderate or severe mitral regurgitation in 65 patients (7%).
| Variable | LV Dyssynchrony (ms) | p Value | ||
|---|---|---|---|---|
| All Patients (n = 976) | ≥130 (n = 129) | <130 (n = 829) | ||
| Age (years) | 61 ± 12 | 63 ± 12 | 60 ± 12 | 0.01 |
| Men | 747 (77%) | 103 (80%) | 631 (76%) | 0.35 |
| Killip class ≥2 | 63 (7%) | 17 (14%) | 42 (5%) | <0.001 |
| Current smoking | 477 (49%) | 61 (48%) | 412 (50%) | 0.66 |
| Diabetes mellitus | 102 (11%) | 23 (18%) | 75 (9%) | 0.002 |
| Hypercholesterolemia ⁎ | 192 (20%) | 30 (23%) | 161 (19%) | 0.29 |
| Hypertension † | 310 (32%) | 46 (36%) | 254 (31%) | 0.23 |
| Previous myocardial infarction | 76 (8%) | 12 (9%) | 61 (7%) | 0.42 |
| QRS duration (ms) | 95 ± 16 | 99 ± 19 | 94 ± 15 | 0.005 |
| Infarct characteristics | ||||
| Left anterior descending coronary artery as culprit artery | 446 (46%) | 72 (56%) | 364 (44%) | 0.01 |
| Multivessel coronary disease | 477 (49%) | 79 (64%) | 385 (46%) | 0.002 |
| TIMI grade 2 or 3 flow | 954 (98%) | 124 (97%) | 814 (98%) | 0.22 |
| Peak creatine phosphokinase level (U/L) | 2,374 ± 3,143 | 2,985 ± 2,773 | 2,255 ± 3,153 | 0.007 |
| Peak cardiac troponin T level (μg/L) | 6.4 ± 6.7 | 9.0 ± 10.1 | 5.9 ± 5.5 | <0.001 |
| Medications at discharge | ||||
| Angiotensin-converting enzyme inhibitors/angiotensin receptor blockers | 925 (97%) | 114 (97%) | 798 (97%) | 0.83 |
| Antiplatelet agents | 952 (100%) | 117 (100%) | 822 (100%) | 0.69 |
| β blockers | 891 (94%) | 108 (92%) | 771 (94%) | 0.54 |
| Statins | 942 (99%) | 113 (97%) | 816 (99%) | 0.008 |
⁎ Total cholesterol ≥190 mg/dl or previous pharmacologic treatment.
† Blood pressure ≥140/90 mm Hg or previous pharmacologic treatment.
| Variable | LV Dyssynchrony (ms) | p Value | ||
|---|---|---|---|---|
| All Patients (n = 976) | ≥130 (n = 129) | <130 (n = 829) | ||
| LV systolic function | ||||
| End-systolic volume (ml) | 57 ± 23 | 64 ± 28 | 56 ± 21 | 0.002 |
| End-diastolic volume (ml) | 106 ± 35 | 111 ± 39 | 105 ± 34 | 0.09 |
| Ejection fraction (%) | 47 ± 9 | 43 ± 11 | 47 ± 9 | <0.001 |
| Wall motion score index | 1.5 ± 0.3 | 1.6 ± 0.4 | 1.5 ± 0.3 | 0.02 |
| Diastolic function | ||||
| E/A ratio | 1.0 ± 0.4 | 1.0 ± 0.4 | 1.0 ± 0.4 | 0.79 |
| Deceleration time (ms) | 212 ± 73 | 206 ± 83 | 213 ± 72 | 0.30 |
| E/E′ ratio | 14 ± 7 | 16 ± 11 | 13 ± 6 | 0.02 |
| Moderate or severe mitral regurgitation | 65 (7%) | 12 (9%) | 51 (6%) | 0.17 |
| LV dyssynchrony (ms) | 61 ± 79 | 224 ± 92 | 35 ± 33 | ⁎ |
Strain analysis was feasible in 98% of the segments. Mean LV dyssynchrony, as assessed with speckle-tracking analysis, was 61 ± 79 ms. As much as 14% of the patient population (n = 129) demonstrated ≥130-ms time differences between the earliest and latest activated segments and were defined as having significant LV dyssynchrony. Patients with LV dyssynchrony were significantly older (63 ± 12 vs 60 ± 12 years, p = 0.01) and more likely to present with Killip class ≥2 (14% vs 5%, p <0.001) and diabetes (18% vs 9%, p = 0.002) compared to those without LV dyssynchrony. In addition, patients with LV dyssynchrony were more likely to have the left anterior descending coronary artery as the culprit vessel (56% vs 44%, p = 0.01), multivessel coronary disease (64% vs 46%, p = 0.002), higher peak cardiac troponin T levels (9.0 ± 10.1 vs 5.9 ± 5.5 μg/L, p <0.001), and longer QRS duration (99 ± 19 vs 94 ± 15 ms, p = 0.005).
When comparing echocardiographic characteristics between patients with and without LV dyssynchrony, patients with LV dyssynchrony had lower LV ejection fractions (43 ± 11% vs 47% ± 9%, p <0.001) and higher wall motion score indexes (1.6 ± 0.4 vs 1.5 ± 0.3, p = 0.02). In addition, LV filling pressures estimated with the E/E′ ratio were higher (16 ± 11 vs 13 ± 6, p = 0.02). When dividing the population according to the LV ejection fraction (<40%, 40% to 50% and ≥50%), there were significant differences in the amount of LV dyssynchrony (analysis of variance p <0.001). These differences were more pronounced in the group of patients with LV ejection fractions <40% (86 ± 90 ms, post hoc Bonferroni test p <0.001), whereas no differences were observed between patients with LV ejection fractions of 40% to 50% and ≥50% (52 ± 76 vs 54 ± 72 ms).
During a mean follow-up period of 40 ± 17 months, 82 patients (8%) reached the primary end point, defined as all-cause mortality. In addition, 36 patients (4%) were hospitalized for heart failure. The Kaplan-Meier curves for patients with and without LV dyssynchrony who reached the primary and secondary end points are shown in Figure 2 . At 3-year follow-up, the cumulative survival was significantly lower in patients with LV dyssynchrony compared to those without (73% vs 96%, p <0.001). In addition, during 3 years of follow-up, the frequency of heart failure hospitalizations in the group of patients with LV dyssynchrony was significantly higher compared to patients without LV dyssynchrony (17% vs 2%, p <0.001). Finally, the event-free survival for the secondary end point at 3-year follow-up was significantly lower in patients with LV dyssynchrony (64% vs 95%, p <0.001).