Radiofrequency catheter ablation (RFCA) is a potential curative treatment for atrial fibrillation (AF) by eliminating the arrhythmia and inducing left atrial (LA) reverse remodeling. However, the effect on LA function, especially after repeated procedures, has scarcely been studied. The aim of this study was to evaluate the impact of RFCA on LA size and function in patients with AF after a first and a repeated procedure. RFCA was performed in 154 patients with symptomatic drug-refractory AF. LA volumes and function were assessed with real-time 3-dimensional echocardiography before and 6 months after the procedure. Recurrence of the arrhythmia was defined as any atrial tachyarrhythmia lasting >30 seconds, clinically documented or by 24-hour Holter recording, after the first 6 months after ablation. Of the 154 patients, 104 (67%) required only a first ablation, and 50 (33%) required redo RFCA. LA volume was reduced after first RFCA (from 60 ± 19 to 52 ±17 ml for 3-dimensional LA maximum volume, p <0.001, and from 38 ± 18 to 33 ± 15 ml for 3-dimensional LA minimum volume, p <0.000) without impairment of LA contractile function, measured as the active emptying percentage of total volume (39 ± 25% vs 43 ± 26%, p = NS). After repeated RFCA procedures, 3-dimensional LA maximum volume was reduced (from 57 ± 18 to 52 ± 18 ml, p = 0.04), also without further LA contractile function impairment (active emptying percentage of total volume) (36 ± 24% vs 36 ± 25% of total volume, p = NS). This effect was similar in paroxysmal and persistent AF. In conclusion, RFCA induces reductions in LA volumes without a deleterious impact on contractile function, even after repeated ablation.
Radiofrequency catheter ablation (RFCA) is a potentially curative and safe invasive treatment of drug-refractory atrial fibrillation (AF). Previous studies have described the effects of RFCA on left atrial (LA) size, with reductions of LA dimensions and volumes and without a significant decrease in LA function, mainly in those patients who maintain sinus rhythm (SR) (responders). Maintenance of LA function has clinical and therapeutic implications, because patients with impaired LA contractile function are at risk for AF recurrence and thromboembolism. Atrial systolic function could decrease after ablation procedures, depending of the size of the scar induced by the lines of radiofrequency application. However, the impact of repeated RFCA has not been extensively studied. Our aim was to evaluate, using real-time 3-dimensional (3D) echocardiography (RT3DE), the impact of repeated RFCA on LA volumes and function, analyzing whether this effect differs between the first and second procedures.
Methods
A total of 158 consecutive patients with symptomatic drug-refractory AF underwent RFCA and RT3DE before and 6 months after it. Of these, 107 patients (68%) underwent a single RFCA procedure, and 51 (32%) required a second procedure. Repeated procedures were indicated when patients persisted with symptomatic AF 3 months after a first ablation despite optimum pharmacologic treatment. AF was paroxysmal in 50% of the patients and persistent in the others (71% persistent and 29% long persistent [>1 year ]). All patients gave written informed consent before echocardiographic studies and RFCA. The ethics committee of our institution approved the study protocol.
Standard 2-dimensional and real-time 3-dimensional transthoracic echocardiography were performed 24 to 48 hours before RFCA. Transesophageal echocardiography was also performed on the same date to rule out thrombus in the left atrium. All images, obtained using a Philips iE33 ultrasound machine (Philips Medical Systems, Andover, Massachusetts), were digitally stored and transferred to a workstation for off-line analysis. In 2-dimensional echocardiographic examinations, LA diameters (anteroposterior diameter) and left ventricular dimensions were measured in the long parasternal axis, and the left ventricular ejection fraction (Simpson’s method) and the peak velocities of late left ventricular filling flow (A wave) and of the mitral annulus (A′ wave determined by Doppler tissue imaging) were also measured.
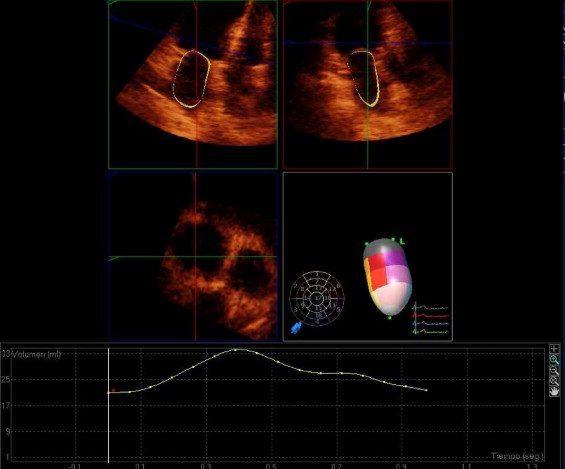
RT3DE was performed in the apical view using an x4 matrix-array transducer (Philips Medical Systems). Full-volume LA scans were acquired as previously described. Volume data were postprocessed using commercially available software (QLAB version 7.1; Philips Medical Systems). After defining the mitral annulus and the roof of the left atrium using 5 points at maximum 3D LA volume (V max-3D ) and minimum 3D LA volume (V min-3D ), in the frame just before the opening and at closure of the mitral valve, respectively, a semiautomatic algorithm of endocardial border detection provided time-volume curves ( Figure 1 ). Precontraction LA volume (Vp 3D ), defined at the P wave on the surface electrocardiogram, was also quantified. LA total emptying volume (V max-3D − V min-3D ), LA passive emptying volume (V max-3D − Vprep 3D ), and LA active emptying volume (Vprep 3D − V min-3D ) were calculated. LA contractile, conduit, and reservoir functions were analyzed using RT3DE. The following indexes were measured to assess contractile function: the LA ejection fraction, obtained as [(V max-3D − V min-3D )/V max-3D × 100]; LA active emptying fraction, calculated as [(Vp 3D − V min-3D )/Vp 3D × 100]; and LA active emptying percentage of total LA emptying, calculated as [(Vp 3D − V min-3D )/(V max-3D − V min-3D )] × 100. LA conduit function was calculated as [(V max-3D − Vp 3D )/V max-3D ] × 100. Finally, the LA expansion index, a surrogate of LA reservoir function, was calculated as (V max-3D − V min-3D )/V min-3D × 100. All measurements were taken as the average of 3 cardiac cycles if SR was present or 5 cycles if AF was present. LA active emptying fraction and LA active emptying percentage of total LA emptying applied only to patients in SR at both examinations. The reproducibility of measuring LA volumes with RT3DE has already been reported by our center. At 6-month follow-up, 2-dimensional Doppler echocardiography and RT3DE were repeated.
During RFCA, catheters were introduced percutaneously through the femoral vein; a transseptal puncture was performed. Heparin was administered to maintain an activated clotting time of 250 to 300 seconds. A 3D map was constructed using an electroanatomic mapping system (CARTO; Biosense Webster, Diamond Bar, California) to support the creation and validation of radiofrequency lesions. Continuous radiofrequency lesions surrounding each ipsilateral pulmonary vein were delivered as previously described. Ablation lines were also deployed in patients with persistent AF along the LA roof. Radiofrequency was delivered through an irrigated-tip thermocouple-equipped catheter, using a target temperature of 45°C at 40 W. The end point was a reduction of local electrogram to <0.15 mV and the establishment of a bidirectional conduction block between the left atrium and pulmonary veins.
Patients were followed at 1, 3, and 6 months to evaluate recurrence, with electrocardiographic monitoring and also 24-hour Holter monitoring to detect asymptomatic AF episodes. Patients were divided into 2 groups for analysis: responders and nonresponders. Recurrent atrial tachyarrhythmia was defined as any atrial tachyarrhythmia documented by electrocardiography or a 24-hour Holter recording lasting >30 seconds during this 6-month period.
Continuous baseline variables are expressed as mean ± SD, depending on normality as assessed using the Shapiro-Wilks test. Categorical variables are expressed as total numbers and were compared between groups using chi-square or Fisher’s exact tests. Continuous variables were tested using unpaired Student’s t tests or Mann-Whitney U tests, according to normality, and paired data using paired Student’s t tests or Wilcoxon’s analysis. Analyses were performed using SPSS version 16.0 (SPSS, Inc., Chicago, Illinois).
Results
In 4 patients, the quality of RT3DE was insufficient to ensure adequate border detection, and these patients were not included in the analysis. Among the remaining 154 patients, 104 (67%) underwent a single RFCA procedure, and 50 (33%) underwent a second procedure.
Table 1 lists the baseline clinical characteristics before the single and the repeated RFCA procedures. There were no significant differences between the groups, including LA size and function. At 6-month follow-up, RFCA was effective in 56 of 104 (54%) patients after a single RFCA procedure and in 20 of 50 (40%) after a redo procedure.
| First RFCA | Repeated RFCA | |
|---|---|---|
| Variable | (n = 104) | (n = 50) |
| Age (years) | 53 ± 11 | 53 ± 10 |
| Men | 81 (71%) | 39 (78%) |
| Hypertension | 45 (43%) | 24 (48%) |
| Paroxysmal AF | 54 (52%) | 23 (46%) |
| Persistent AF | 33 (32%) | 22 (44%) |
| Long persistent AF | 17 (16%) | 5 (10%) |
| Preprocedural SR | 53 (51%) | 26 (52%) |
| Antiarrhythmic drugs | 1.5 ± 1 | 1.7 ± 1 |
| AF duration (months) | 52 ± 34 | 71 ± 54 |
| LV hypertrophy | 24 (23%) | 11 (22%) |
| Mild MR | 46 (44%) | 25 (50%) |
| Mild AR | 16 (15%) | 7 (14%) |
| LV ejection fraction <50% | 11 (12%) | 7 (14%) |
| LV ejection fraction (%) | 59 ± 9 | 59 ± 10 |
| LV end-diastolic diameter (mm) | 52 ± 5 | 53 ± 5 |
| LV end-systolic diameter (mm) | 34 ± 6 | 34 ± 7 |
Baseline and follow-up LA dimensions and function are listed in Table 2 . Overall, a first RFCA procedure induced a significant decrease from baseline for LA V max-3D , with mean reductions of 11.4% (p <0.0001) and 6% for LA V min-3D (p <0.0001). This reduction after repeated RFCA was also significant for LA V max-3D , with a mean reduction of 5.6% (p <0.04), but not for LA V min-3D (p <0.06). There were no significant changes in LA systolic and diastolic function parameters after either a first or a repeated RFCA procedure. Slightly decreased LA conduit function and peak A-wave velocity were observed after a first ablation procedure.
| Variable | First RFCA (n = 104) | Repeated RFCA (n = 50) | ||
|---|---|---|---|---|
| Before RFCA | After RFCA | Before RFCA | After RFCA | |
| LA size | ||||
| Anteroposterior diameter (mm) | 43 ± 6 | 42 ± 6 | 43 ± 6 | 42 ± 6 |
| V max-3D (ml) | 60 ± 19 | 52 ± 17* | 57 ± 18 | 52 ± 18* |
| V min-3D (ml) | 38 ± 18 | 33 ± 15* | 37 ± 17 | 35 ± 15 |
| LA active emptying fraction (ml) | 10 ± 8 | 9 ± 8 | 8 ± 6 | 6 ± 4 |
| LA function | ||||
| LA contractile function | ||||
| LA ejection fraction (%) | 37 ± 18 | 36 ± 17 | 35 ± 17 | 34 ± 15 |
| LA active emptying fraction (%) | 25 ± 14 | 24 ± 16 | 23 ± 18 | 18 ± 15 |
| LA active emptying percentage of total LA emptying (%) | 39 ± 25 | 43 ± 26 | 36 ± 24 | 36 ± 25 |
| LA conduit function (%) | 30 ± 15 | 24 ± 13* | 28 ± 13 | 25 ± 13 |
| LA expansion index | 73 ± 65 | 67 ± 44 | 67 ± 59 | 60 ± 39 |
| Peak A-wave velocity (cm/s) | 63 ± 22 | 57 ± 18* | 49 ± 16 | 47 ± 15 |
| A-wave velocity-time integral | 7.7 ± 3.4 | 7.8 ± 3.5 | 6.2 ± 2 | 6.6 ± 2 |
Figure 2 shows the effect of RFCA on LA size and function according to patient response. At baseline, patients in the single-ablation group with arrhythmia recurrence after RFCA (nonresponders, n = 49 [47%]) had significantly larger LA volumes compared to responders (n = 55 [53%]). However, there were no significant differences in baseline LA size (before the repeated RFCA) in patients who underwent repeated RFCA, whether they were responders (n = 20 [40%]) or not (n = 30 [60%]).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


