Patients with acute coronary syndrome (ACS) comprise a heterogeneous group. Despite clear guidelines, the management of ACS in clinical practice is variable. We aimed to evaluate clinical characteristics and myocardial revascularization patterns of patients presenting with ACS from a large French nationwide registry. The National Observational Study of Diagnostic and Interventional Cardiac Catheterization is a multicenter registry including all interventional cardiology procedures performed since 2004. Patient demographics and co-morbidities, invasive parameters, treatment options, and procedural techniques were prospectively collected. The present study is focused on data collected between 2004 and 2008. Patients were recruited in 99 hospitals (55% in private clinics, 45% in public institutions). Over a 5-year period, 64,932 patients with ACS were included (mean age 65.7 ± 13.3; 73% men, 31% ST-elevation myocardial infarction [STEMI]). Patients presenting with unstable angina pectoris and non-ST-elevation myocardial infarction weresimilar with regards to clinical presentation and coronary artery disease (CAD) extension. Overall, these patients were older, had a higher cardiovascular risk profile, and had more severe CAD compared with STEMI patients. In-hospital mortality during the first 24 hours was higher in STEMI patients. Patient’s characteristics and CAD were highly dependent on the type of ACS. Patients with unstable angina/non-STEMI were older and had a more severe CAD. In-hospital complications were higher in STEMI patients.
Acute coronary syndrome (ACS) represents a heterogeneous spectrum of conditions, and its management is well defined and summarized in reviews and guidelines. However, in clinical practice, there is a considerable heterogeneity in patient management. Therefore, large-scale observational data sets are important to assess information obtained via randomized clinical trials. The aim of this study was to evaluate the clinical characteristics and management of patients admitted for ACS from the French National Observational Study of Diagnostic and Interventional Cardiac Catheterization (ONACI).
Methods
We selected patients presenting with ACS from the ONACI registry, the methodology of which has been previously described. Briefly ONACI was set up in 2004 and is a national, prospective multicenter registry including most of the interventional cardiology procedures performed in France.
Consecutive patients aged >18 years who underwent coronary angiography (CAG) and/or percutaneous coronary intervention (PCI) were included in this registry. The present study focuses on data gathered over a period of 5 years (from 2004 to 2008). Participation in this registry was on a voluntary basis and did not affect the therapeutic approach of cardiologists in any way.
Our population was divided into 2 groups; the first included patients who underwent CAG (±PCI) and was analyzed to evaluate clinical characteristics and angiographic features. The second group, including patients who underwent PCI (±CAG), was used to assess procedural characteristics. PCI success was defined as ≥20% decrease in diameter stenosis to a postprocedure value <50%, with Thrombolysis In Myocardial Infarction Trial flow grade 3.
Participation in the study was voluntary and included university, general and regional hospitals, and private clinics. In each center, a physician was in charge of the registry and provided a full list of all patients admitted to the unit.
Data collection has been previously described. Data were entered in local electronic databases at each center by the physicians who performed the procedures, and data files were sent every 6 months to the French Society of Cardiology, where they were merged into a common database. The following data were prospectively collected and electronically stored for each patient: demographic characteristics (age, gender, and body mass index), cardiovascular risk factors (arterial hypertension, body mass index ≥30, diabetes, current smoking, hyperlipidemia), and medical cardiovascular history (past history of acute myocardial infarction, PCI, coronary artery bypass grafting, peripheral artery disease, chronic kidney disease). Chronic kidney disease was defined as creatinine clearance <30 ml/min or serum creatinine value >15 mg/L. Left ventricular ejection fraction, assessed at admission or at any time during the hospital stay, was recorded. Procedural informations about PCI, such as disposable equipment and stents used, vessels treated by angioplasty (e.g., number of lesions treated and of stents implanted) were collected as previously described. Finally, in-hospital complications (death, stroke, myocardial infarction, and renal failure) occurring within 24 hours after of the procedures were recorded. Data were then checked for coherence and completeness by a cardiologist and a statistician (EP and MCP); individual records with excessive missing data were excluded from the current analysis.
The study was conducted in compliance with Good Clinical Practice, French Law, and the French data protection law. The protocol was reviewed by the Committee for the Protection of Human Subjects in Biomedical Research of Saint-Antoine University Hospital. The data file of the ONACI registry was declared to and authorized by the French data protection committee (Commission Nationale Informatique et Liberté).
Statistical analysis was performed using SPSS 18.0 software (SPSS Inc., Chicago, IL, USA). For quantitative variables, means, SDs, and minimum and maximum values were calculated. In addition, medians with the interquartile range were calculated for some of the variables. Discrete variables are presented as percentages. Comparisons were made with chi-square or Fisher’s exact tests for discrete variables and by unpaired t tests, Wilcoxon signed-rank tests, or 1-way analysis of variance for continuous variables. For all analyses, a p value <0.05 was considered significant.
Results
Over a 5-year period, 64,932 patients presenting with ACS were included in the registry (ST-elevation myocardial infarction [STEMI] 31%, non-STEMI [NSTEMI] 29%, unstable angina pectoris [UAP] 40%).
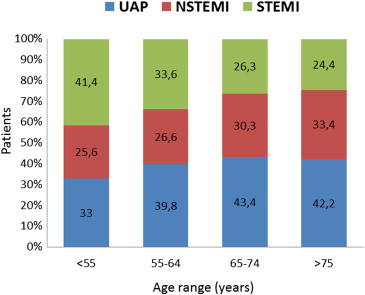
Baseline clinical characteristics of patients hospitalized for ACS are summarized in Table 1 . Overall, NSTEMI and UAP populations were similar. Compared with the STEMI group, they were older and had a higher cardiovascular risk profile with more diabetes, hypertension, and dyslipidemia. They also presented with more co-morbidities (peripheral artery disease, chronic kidney disease) and more past history of CAD (acute myocardial infarction, PCI, coronary artery bypass grafting) compared with STEMI patients. The rate of current smokers was higher in STEMI patients. Likewise, the clinical presentation of the patients varied with age; there was a significant increase with age of the ratio of UAP and NSTEMI and a decrease of STEMI ( Figure 1 ).
| Variable | UAP (n = 25,916) | NSTEMI (n = 19,058) | STEMI (n = 19,958) | ACS (n = 64,932) | p Value |
|---|---|---|---|---|---|
| Age (yrs) | 66.9 ± 12.5 | 67.0 ± 13.1 | 62.8 ± 13.9 | 65.7 ± 13.3 | <0.001 |
| Men | 18,461 (71) | 13,861 (73) | 15,306 (77) | 47,628 (73) | <0.001 |
| BMI | 27.1 ± 4.6 | 27.0 ± 4.7 | 26.6 ± 4.3 | 26.9 ± 4.5 | <0.001 |
| LVEF (%) | 61 ± 12 | 57 ± 13 | 53 ± 13 | 58 ± 13 | <0.001 |
| Family history of CAD ∗ | 6,024 (25) | 3,747 (21) | 3,436 (19) | 13,207 (20) | <0.001 |
| Previous AMI | 4,001 (16) | 2,682 (15) | 1,480 (8) | 8,163 (13) | <0.001 |
| Previous PCI | 7,311 (29) | 3,431 (19) | 1,962 (11) | 12,704 (20) | <0.001 |
| Previous coronary bypass | 2,073 (8) | 1,348 (7) | 421 (2) | 3,842 (6) | <0.001 |
| Peripheral vascular disease | 2,594 (11) | 1,917 (11) | 933 (5) | 5,444 (8) | <0.001 |
| Chronic kidney disease † | 1,539 (6) | 1,564 (9) | 523 (3) | 3,626 (6) | <0.001 |
| Smoker | 11,357 (45) | 7,840 (42) | 9,413 (49) | 28,610 (44) | <0.001 |
| Diabetes mellitus | 5,777 (23) | 4,393 (24) | 2,949 (16) | 13,119 (20) | <0.001 |
| Hypertension ‡ | 14,774 (58) | 10,179 (55) | 7,977 (42) | 32,930 (51) | <0.001 |
| Hyperlipidemia § | 15,259 (61) | 10,146 (55) | 7,934 (43) | 33,339 (51) | <0.001 |
∗ History of myocardial infarction at any age in first-degree relative.
† Creatinine clearance <30 ml/mm or creatinine >15 mg/L.
‡ Systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure <90 mm Hg (treated or not).
§ Included patients with previously documented diagnosis of hypercholesterolemia treated with diet or medication or a new diagnosis made during this hospitalization with elevated total cholesterol 190 mg/dl (or LDL-choesterol >130 mg/dl). Did not include elevated triglycerides.
The results of CAG are listed in Table 2 . The rate of CAG with normal coronary arteries or nonsignificant coronary lesions (<50% of diameter stenosis) was higher in NSTEMI and UAP patients. Patients admitted for STEMI more frequently had 1-vessel disease, whereas NSTEMI and UAP patients had more severe and diffuse coronary artery disease (i.e., a higher rate of patients with 2- or 3-vessel disease and more patients with left main coronary artery lesions).
| Coronary Narrowing | UAP (n = 25,916) | NSTEMI (n = 19,058) | STEMI (n = 19,958) | ACS (n = 64,932) | p Value |
|---|---|---|---|---|---|
| None ∗ | 4,180 (16) | 2,099 (11) | 739 (4) | 7,018 (11) | |
| No of coronary arteries narrowed | |||||
| 1 | 7,216 (30) | 4,274 (29) | 7,108 (41) | 21,098 (32.5) | <0.001 |
| 2 | 6,727 (28) | 4,397 (29) | 5,404 (31) | 19,028 (29) | |
| 3 | 6,396 (26) | 4,714 (31) | 4,176 (24) | 17,786 (27) | |
| Left main coronary artery | 1,748 (7) | 1,159 (6) | 722 (4) | 3,629 (6) |
Baseline procedural features are summarized in Table 3 , and the choice of treatment is shown in Figure 2 . Overall, PCI was performed in 70% of ACS (ranging from 89.4% to 62.3% as indicated). Figure 3 shows the treatment according to ACS and age classes. A trend toward less revascularization in STEMI and more in NSTEMI and UAP was noted with age. Radial access was mostly used in NSTEMI and UAP patients, whereas STEMI patients were predominantly investigated by femoral access. The numbers of lesions treated per procedure and per patient as well as the total number of stents used were lower for STEMI patients compared with NSTEMI and UAP patients. Drug-eluting stents were more often used in NSTEMI and UAP patients.
| Variable | UAP (n = 17,325) | NSTEMI (n = 13,887) | STEMI (n = 17,692) | ACS (n = 48,904) | p Value |
|---|---|---|---|---|---|
| Sheath size | |||||
| 5F | 3,147 (19) | 2,400 (17) | 1,486 (9) | 7,033 (15) | <0.001 |
| 6F | 13,448 (79) | 11,026 (81) | 15,836 (90) | 40,310 (84) | |
| 7F | 329 (2) | 255 (2) | 172 (1) | 756 (2) | |
| ≥8F | 38 (<1) | 38 (<1) | 50 (<1) | 126 (<1) | |
| Approach | |||||
| Femoral | 7,596 (44) | 7,309 (53) | 9,821 (56) | 24,726 (51) | <0.001 |
| Radial | 9,519 (55) | 6,423 (46) | 7,712 (43) | 23,654 (49) | |
| Brachial | 103 (<1) | 90 (<1) | 59 (<1) | 257 (<1) | |
| Number PCI per patient | |||||
| 1 | 10,517 (61) | 8,809 (64) | 13,084 (74) | 32,410 (68) | <0.001 |
| 2 | 4,505 (26) | 3,480 (25) | 3,182 (18) | 11,167 (24) | |
| 3 | 1,411 (8) | 1,039 (8) | 710 (4) | 3,160 (7) | |
| ≥4 | 351 (2) | 246 (2) | 133 (1) | 730 (2) | |
| Coronary artery intervention | |||||
| Left main | 564 (3) | 394 (3) | 257 (1.5) | 1,215 (2.5) | <0.001 |
| Left anterior descending | 8,175 (47) | 6,228 (45) | 7,672 (43) | 22,075 (45) | |
| Left circumflex | 5,343 (31) | 4,636 (33) | 3,193 (18) | 13,172 (27) | |
| Right | 5,776 (33) | 4,556 (33) | 7,118 (40) | 17,450 (36) | |
| Coronary bypass | 423 (2.5) | 366 (3) | 122 (1) | 911 (2) | |
| No. of PCI per procedure | 1.5 ± 2.1 | 1.4 ± 0.7 | 1.3 ± 1.0 | 1.3 ± 0.7 | 0.01 |
| No. of stents used | |||||
| 0 | 1,049 (6) | 866 (6) | 1,578 (9) | 3,493 (7) | |
| 1 | 9,975 (58) | 8,004 (58) | 10,758 (61) | 28,737 (59) | |
| 2 | 4,373 (25) | 3,464 (25) | 4,061 (23) | 11,898 (24) | <0.001 |
| 3 | 1,401 (8) | 1,164 (8) | 1,006 (6) | 3,571 (7) | |
| ≥4 | 514 (3) | 385 (3) | 284 (2) | 1,183 (3) | |
| Number of stents used per procedure | 1.5 ± 2.1 | 1.5 ± 0.9 | 1.3 ± 1.1 | 1.5 ± 0.8 | 0.004 |
| Drug-eluting stent | 6,058 (44) | 4,662 (38) | 2,501 (12) | 13,221 (28) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


