FIGURE 28.1. Report of a vein mapping.
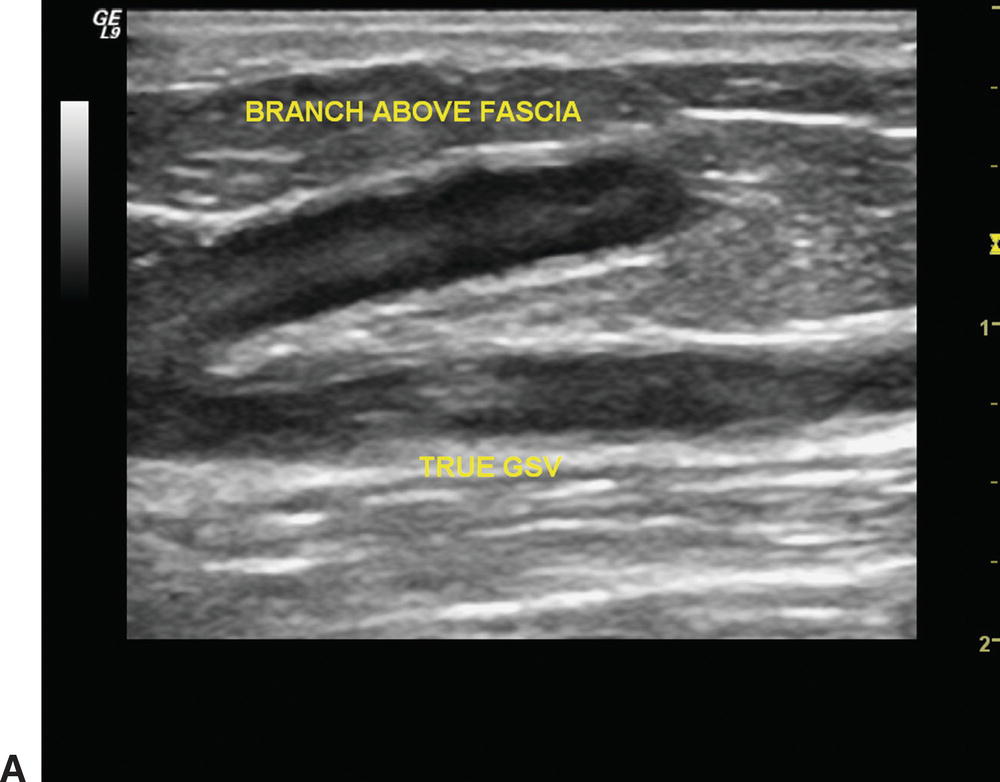
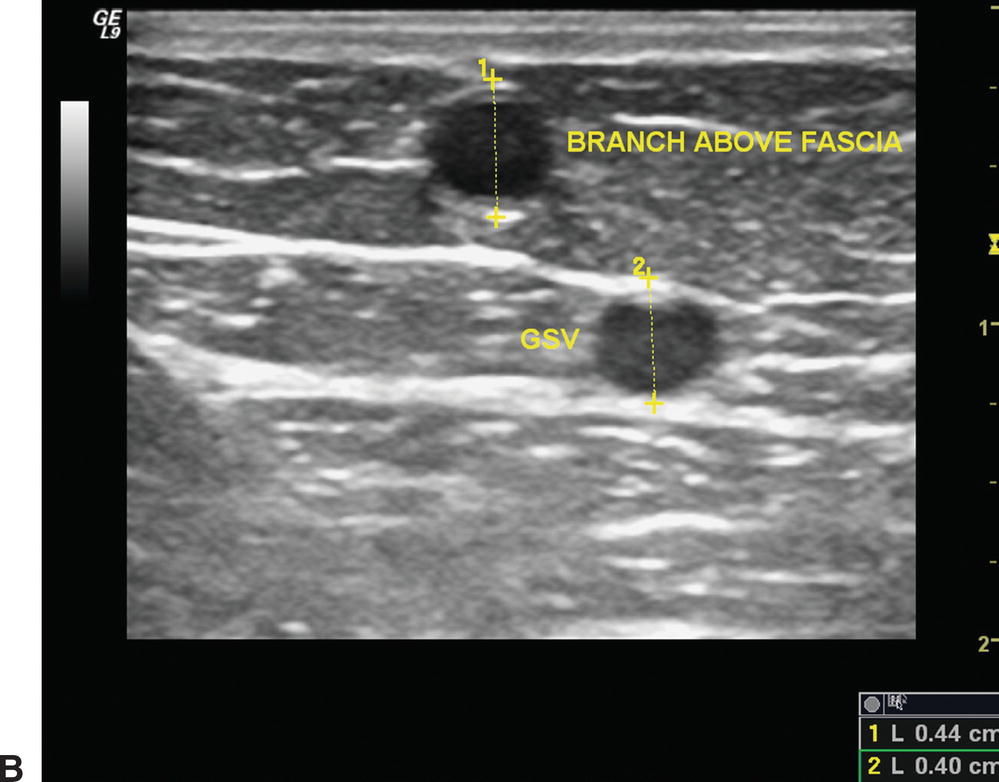
FIGURE 28.2. Images of a “duplicate” saphenous vein system with branches above and below the fascia in longitudinal (A) and cross-sectional (B) views.
Patency of the vein is determined by documenting spontaneous flow or flow with augmentation. Prior to recording of diameters, a sweep is made and compression of the vein is carried out over its entire length with the probe in transverse view to look for any wall thickening or intraluminal defects such as chronic phlebitis (Fig. 28.3). Scanning is then carried out from the SFJ, and cross-sectional measurements are documented incrementally at the SFJ, proximal, medial, and distal thigh, knee, and proximal, mid, and distal calf. Varicosities and incompetent segments are noted.
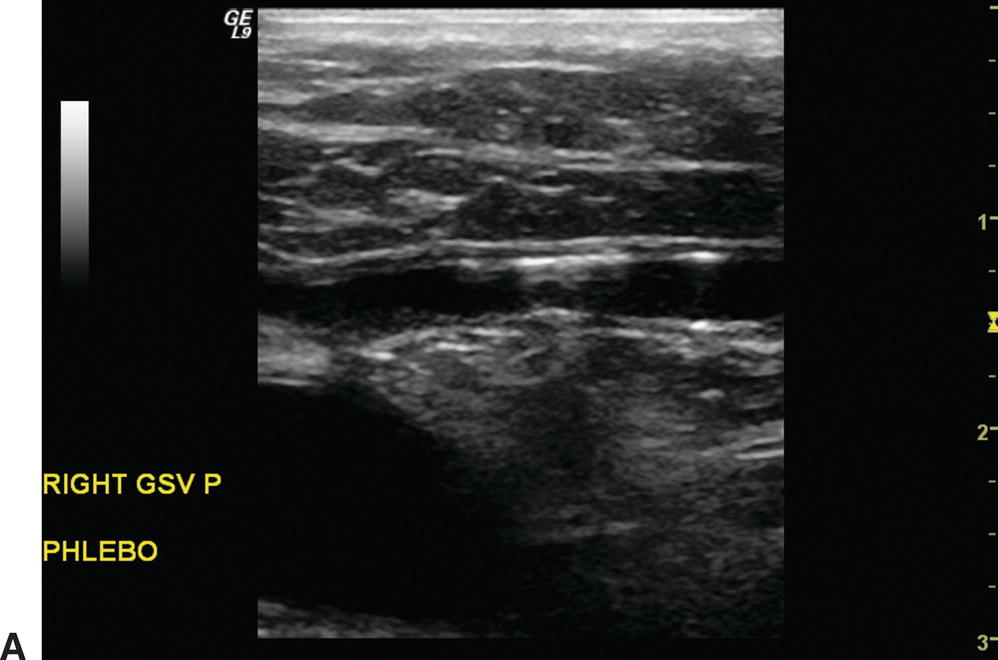
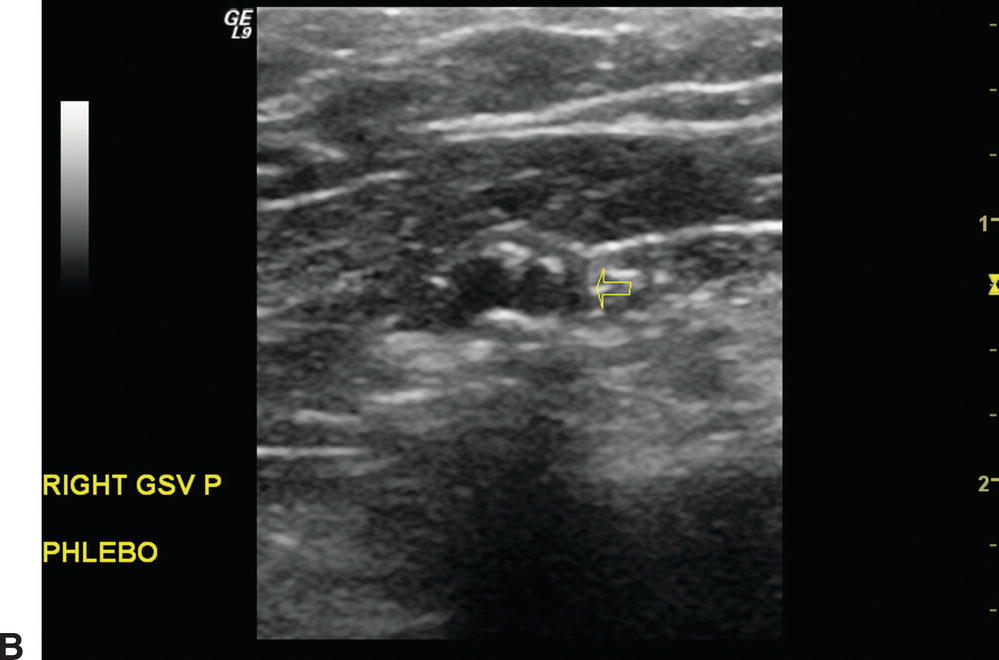
FIGURE 28.3. Images of phlebosclerosis in a vein in longitudinal (A) and cross-sectional (B) views.
Documentation of vein diameter is performed from proximal to distal. The vein should be imaged in both cross-sectional and longitudinal views. Figure 28.4 shows a cephalic vein with an adequate diameter for bypass, and Figure 28.5 shows a cephalic vein with diameters too small to be used as conduit. Care must be taken to avoid compressing the vein with the probe and making the diameter falsely small. If the vein appears to be in spasm (with bright, thick walls), warming the limb with heated towels, increasing the degree of reverse Trendelenburg, or using a tourniquet may be helpful. If these measures do not change the appearance of the vein, it is likely that the vein is sclerotic rather than in spasm. If the vein diameter is inadequate or borderline, the surgeon should be notified during the examination. Any abnormalities such as intraluminal defects, varicose segments, or sclerosis should also be communicated to the surgeon.
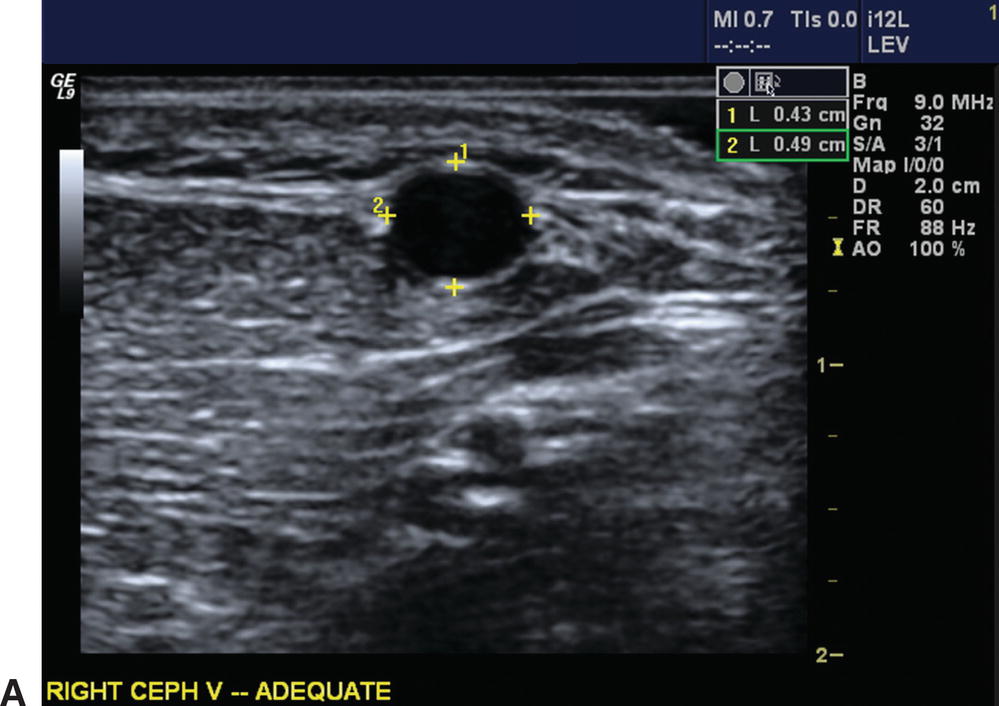
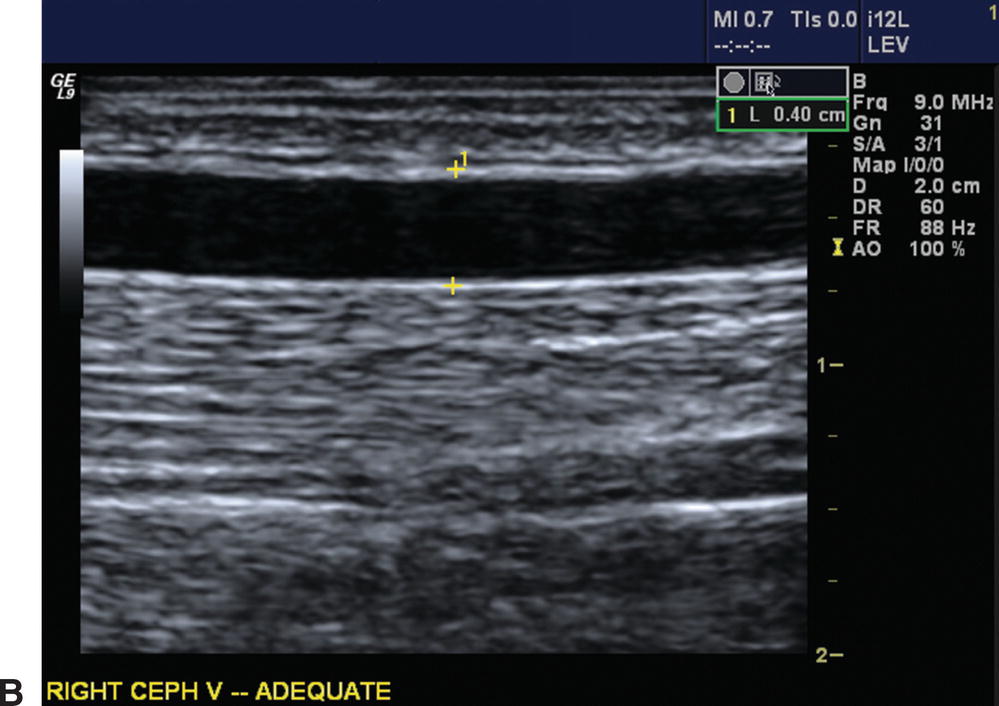
FIGURE 28.4. Images of a cephalic vein in longitudinal (A) and cross-sectional (B) views. Diameter measurements are indicated and are adequate for use as a bypass conduit.
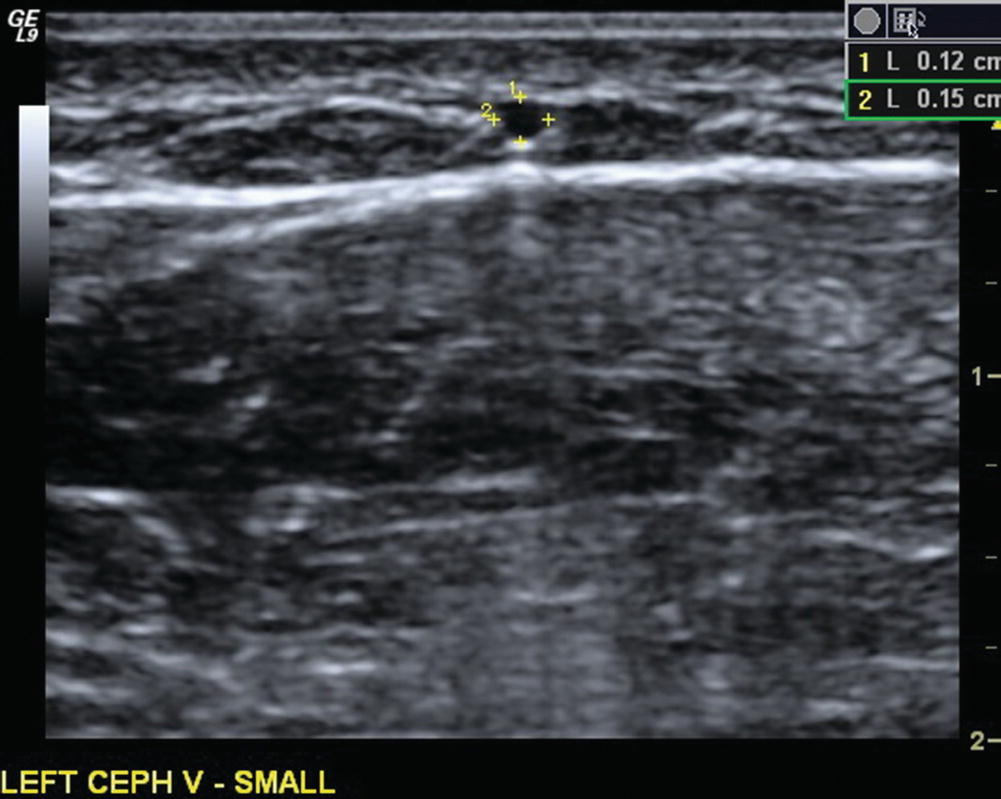
FIGURE 28.5. Cephalic vein in cross section with diameters of 0.12 cm and 0.15 cm, too small to use as a bypass conduit.
Marking the course of the vein on the skin while scanning can be problematic, as pens typically will not mark through ultrasound gel. In our vascular laboratory, we make dashed lines along the course of the vein through the gel with a colored pencil. It is important to hold the transducer at a right angle to the patient’s skin while marking in order to place the mark directly over the vein. The locations of all branches and perforator veins are also marked (branches drawn on and perforators denoted by the letter “P”). The leg is then wiped clean of gel, and the dashed lines are connected with an indelible marker. Following this second stage of marking, the transducer is placed perpendicularly over the mark to ensure that it is directly over the vein. This spot check is performed over the length of the marked vein. This double check is important, as the surgeon relies intraoperatively on precise marking of the course and location of the vein and branch points. If the vein is marked “off center,” the incision may be misplaced, causing a skin flap. Figures 28.6 and 28.7 show vein mapping of both a GSV and of arm veins. An alternative method of marking is to use the tip of a straw to gently make indentations in the skin over the vein and then use a pen to connect the indentations.

FIGURE 28.6. Great saphenous vein map with branches and perforators (P) indicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


