Prehospital electrocardiographic (ECG) diagnosis has improved triage and outcome in patients with acute ST-elevation myocardial infarction. However, many patients with acute myocardial infarction (AMI) present with equivocal ECG patterns making prehospital ECG diagnosis difficult. We aimed to investigate the feasibility and ability of prehospital troponin T (TnT) testing to improve diagnosis in patients with chest pain transported by ambulance. From June 2008 through September 2009, patients from the central Denmark region with suspected AMI and transported by ambulance were eligible for prehospital TnT testing with a qualitative point-of-care test (cutpoint 0.10 ng/ml). Quantitative TnT was measured at hospital arrival and after 8 and 24 hours (cutpoint 0.03 ng/ml). A prehospital electrocardiogram was recorded in all patients. Prehospital TnT testing was attempted in 958 patients with a 97% success rate. In 258 patients, in-hospital TnT values were increased (≥0.03 ng/ml) during admission. The prehospital test identified 26% and the first in-hospital test detected 81% of patients with increased TnT measurements during admission. A diagnosis of AMI was established in 208 of 258 patients with increased TnT. The prehospital test identified 30% of these patients, whereas the first in-hospital test detected 79%. Median times from symptom onset to blood sampling were 83 minutes (46 to 167) for the prehospital sample and 165 minutes (110 to 276) for the admission sample. In conclusion, prehospital TnT testing is feasible with a high success rate. This study indicates that prehospital implementation of quantitative tests, with lower detection limits, could identify most patients with AMI irrespective of ECG changes.
Prehospital electrocardiographic (ECG) diagnosis has improved triage and outcome in patients with acute ST-elevation myocardial infarction (STEMI). However, many patients with acute MI (AMI) present with equivocal ECG patterns making prehospital ECG diagnosis difficult. Point-of-care biomarker testing could improve prehospital diagnosis and triage in patients with AMI. Previous studies on prehospital biomarker testing for diagnosing AMI have been discouraging. However, the test kits used have been insensitive and the studies were performed under various settings. Most importantly, the benefit from the combined use of prehospital biomarkers and ECG diagnosis in prehospital triage and referral of patients with suspected acute coronary syndrome is unknown and the feasibility of prehospital biomarker testing by paramedics, unfamiliar with this procedure, has not been tested. The purpose of the present study was to test the feasibility and diagnostic value of prehospital troponin T (TnT) testing in patients with suspected AMI using a qualitative point-of-care kit when performed by paramedics.
Methods
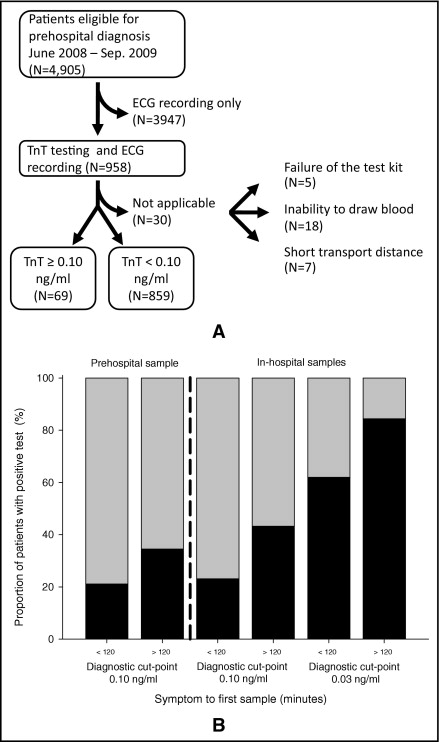
The study was conducted in the central Denmark region from June 18, 2008 through September 17, 2009. In total 4,905 patients with suspected acute coronary syndrome were transported by the emergency medical services in this period. An electrocardiogram was recorded in all patients and transmitted wirelessly to an on-call cardiologist for immediate interpretation at Aarhus University Hospital (Skejby, Denmark) as part of routine prehospital patient care. Electrocardiograms were digitally recorded in the ambulance and stored in an in-hospital database.
Patients transported in an ambulance with a paramedic trained in the procedure were eligible for prehospital TnT testing. Initially 11 paramedic supervisors were trained in the blood testing technique by laboratory technicians. These supervisors rotated among the 70 ambulances servicing the study region and gradually trained additional paramedics in the technique. Prehospital TnT testing was attempted in 958 patients. The remaining patients were transported in ambulances without equipment or staff for TnT measurement.
As part of routine practice a peripheral, intravenous access was established in all patients transported by emergency medical services. From the intravenous cannula blood 1 ml was drawn using a special blood collection tube with manually induced vacuum (Sarstedt Lithium-Heparin Coated S-Monovette, Sarstedt AG and Co., Nümbrecht, Germany). A sample of heparinized whole blood 150 μl was then transferred to a qualitative TnT test kit (TROP T Sensitive, Roche Diagnostics, GmbH, Mannheim, Germany). The result was read after 15 minutes (or sooner when positive) and recorded by the paramedics and reported to the on-call cardiologist. The qualitative TnT test had a diagnostic cutpoint of 0.10 ng/ml. On hospital arrival TnT was measured quantitatively using the well-validated Roche Elecsys analyzer (Roche Diagnostics, GmbH). The cutpoint for the quantitative test was ≥0.03 ng/ml. A TnT control lysate (Roche Diagnostics, GmbH) was used throughout the study period to spot-check the quality and validity of the tests.
The final diagnosis of AMI was based on the universal definition of MI with an increase and/or decrease pattern of TnT with ≥1 value above the 99th percentile together with symptoms of ischemia and/or ECG changes indicative of new ischemia. The diagnosis was adjudicated independently by 2 cardiologists (J.T.S. and C.S.) reviewing ECG, laboratory, angiographic, and imaging data in patients with increased in-hospital TnT values (≥0.03 ng/ml) and/or prehospital TnT values (≥0.10 ng/ml) together with admission and discharge papers. For discordance between the 2 adjudicators, a third cardiologist reviewed the data to reach consensus.
The on-call cardiologist recorded baseline demographic and timing data on all patients in the acute phase using a Web-based registration form. ECG changes, preliminary diagnosis, and any possible implications for management (e.g., direct referral of patients with ST-segment elevation to a primary percutaneous coronary intervention center) were recorded. Additional timing and dispatch data were obtained from the emergency medical services provider (Falck Denmark A/S, Copenhagen, Denmark). Admission and discharge papers were acquired in hard or digital copy from the concerned hospitals. The study was approved by the Danish Data Protection Agency and the Danish National Board of Health.
Dichotomous data are presented as absolute numbers (percentages of valid cases). Continuous variables are presented as medians (25th to 75th percentiles). Fisher’s exact test, chi-square test, and Mann–Whitney test were used for comparison of categorical and continuous variables as appropriate. A statistically significant p value <0.05 (2-sided test) was chosen.
Results
In the full cohort of 4,905 patients, 1,240 patients (25%) had increased TnT levels at some point during admission. In addition, 954 patients (19%) had a typical increase and/or decrease pattern of their TnT values plus symptoms and ECG changes indicative of AMI. A final diagnosis of STEMI was assigned to 345 patients (7%), 491 patients (10%) were diagnosed with non-STEMI, and 118 patients (2%) received a diagnosis of bundle branch block MI (BBBMI). TnT increase from causes other than AMI was recognized in 286 patients (6%).
Baseline characteristics for patients with and without prehospital TnT measurement are listed in Table 1 . Patients with prehospital TnT testing less often had prehospital cardiac arrest (p = 0.03) and more often received aspirin (p = 0.01) and clopidogrel (p <0.001) in the ambulance. A final diagnosis of non-STEMI was more prevalent in this group.
| Variable | Prehospital TnT Test (n = 958) | No Prehospital TnT Test (n = 3,947) | p Value |
|---|---|---|---|
| Age (years) | 66 (55–78) | 67 (55–79) | 0.69 |
| Men | 565 (59%) | 2,380 (60%) | 0.45 |
| Systolic blood pressure (mm Hg) | 143 (128–161) | 143 (126–164) | 0.81 |
| Heart rate (beats/min) | 83 (70–97) | 83 (70–99) | 0.41 |
| Previous myocardial infarction | 226 (25%) | 980 (26%) | 0.27 |
| Previous percutaneous coronary intervention or coronary artery bypass grafting | 218 (24%) | 831 (23%) | 0.41 |
| Diabetes mellitus | 111 (12%) | 397 (11%) | 0.30 |
| Prehospital cardiac arrest ⁎ | 9 (1%) | 77 (2%) | 0.03 |
| Prehospital aspirin | 713 (76%) | 2,499 (65%) | <0.001 |
| Prehospital clopidogrel | 77 (8%) | 222 (6%) | 0.01 |
| Prehospital heparin | 64 (7%) | 213 (6%) | 0.14 |
| Patient referred directly for primary percutaneous coronary intervention | 78 (8%) | 293 (8%) | 0.51 |
| Positive troponin T during admission | 258 (27%) | 982 (25%) | 0.87 |
| Acute myocardial infarction during admission | 208 (22%) | 746 (19%) | 0.05 |
| Noncardiac/nonacute myocardial infarction troponin T increase | 50 (5%) | 236 (6%) | 0.37 |
| Final acute myocardial infarction diagnosis | |||
| ST-elevation myocardial infarction | 66 (7%) | 279 (7%) | 0.89 |
| Non–ST-elevation myocardial infarction | 119 (12%) | 372 (9%) | 0.009 |
| Bundle branch block myocardial infarction | 23 (2%) | 95 (2%) | 0.99 |
| Median peak troponin T level (μg/L) | 0.22 (0.06–1.4) | 0.32 (0.07–1.3) | 0.61 |
| Median creatinine level at admission (μmol/L) † | 80 (68–92) | 80 (67–96) | 0.99 |
| Median time spend on scene (minutes) | 23 (19–29) | 22 (17–27) | <0.001 |
⁎ Defined as attempted cardiopulmonary resuscitation and/or defibrillation in ambulance.
† Creatinine was available for 649 patients, 139 in the group with prehospital troponin T and 510 in the group without.
Prehospital TnT testing was attempted in 958 patients and was successful in 928 patients (97%). The main reasons for failed blood testing were related to the intravenous cannula and problems drawing blood in the collection tube ( Figure 1 ). Prehospital qualitative TnT test values were positive in 69 patients. This result was confirmed by in-hospital measurements in 65 of these patients.
Of patients with prehospital TnT testing 78 were triaged directly to the catheterization laboratory for primary percutaneous coronary intervention. In 9 of these patients (12%) the decision to redirect patients was based primarily on the positive TnT result because the ECG pattern was equivocal or BBB of uncertain origin was present.
Times from onset of symptoms to prehospital TnT sample were <2 hours in 65% of patients and <6 hours in 90% of patients.
Of the 958 patients with prehospital TnT testing 258 had TnT concentrations ≥0.03 ng/ml during admission. The prehospital qualitative TnT test identified 65 of these patients (25%). Sensitivity of the qualitative test to identify patients with a final diagnosis of AMI was 31%; ( Table 2 ).



