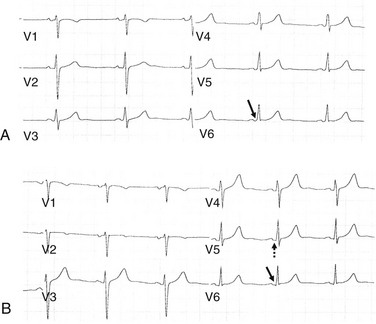
76 If the AP is capable of anterograde conduction, the baseline ECG demonstrates a short PR interval and a slurred upstroke of the QRS complex referred to as a delta wave, hallmarks of ventricular preexcitation. The AP thus is considered to be manifest (Figure 76-1). In approximately 50% of patients with AVRT, the accessory pathway is capable of only retrograde conduction. The ECG during sinus rhythm in these patients shows a normal QRS complex, and therefore the accessory connection is considered to be concealed. Patients with evidence of preexcitation on the resting ECG and symptomatic tachycardia are said to have the Wolff-Parkinson-White (WPW) syndrome. An asymptomatic patient who incidentally is found to have preexcitation on the ECG is said to have a WPW “pattern.” Figure 76-1 Ventricular Preexcitation The presentation of patients with AVRT is clinically indistinguishable from that of patients with other mechanisms of PSVT. Symptoms commonly include rapid palpitations, chest discomfort, dizziness/light-headedness, dyspnea, weakness, neck pulsations, and presyncope. Syncope is an uncommon symptom of AVRT. Occasionally, patients with AVRT develop atrial fibrillation (AF), which may lead to hemodynamic deterioration as the result of rapid anterograde conduction over the accessory pathway (Figure 76-2). This may cause syncope, cardiac arrest, or sudden death. Figure 76-2 Preexcited Atrial Fibrillation (AF) Supraventricular tachycardia in association with ventricular preexcitation is considered a class I indication for electrophysiological evaluation and catheter ablation.1 Catheter ablation is highly effective in eliminating AP conduction, thereby eliminating symptoms caused by SVT and the small risk of sudden death associated with the WPW syndrome. Patients with WPW syndrome in whom ablation would be likely to result in high-grade AV block should be treated with a combination of rhythm- and rate-controlling medications. One study found that after a first episode of tachycardia in patients with WPW syndrome, a large proportion of patients remained asymptomatic over the next several years.2 The risk of adverse events during follow-up was very low. Investigators identified high-risk features including a short AP effective refractory period, inducible AVRT triggering preexcited AF, and the presence of multiple accessory pathways. The low event rate after a first episode of AVRT suggests that long-term pharmacologic treatment may not be needed until the tachycardia becomes recurrent. Most asymptomatic patients in whom the ECG incidentally shows evidence of preexcitation do not require an electrophysiological evaluation because their risk of sudden death is very low.1,3 However, data suggest that catheter ablation in this group reduces the risk of arrhythmic events.4 The decision to perform catheter ablation in asymptomatic patients with “high-risk” occupations, for example, pilots and bus drivers, should be individualized. In patients referred for an electrophysiological evaluation for PSVT, the ECG during sinus rhythm and during tachycardia may be helpful in identifying the mechanism of the tachycardia. Evidence of preexcitation during sinus rhythm in a patient with a history of tachycardia makes AVRT very likely. The degree of preexcitation may be subtle, especially in patients with a left free wall or with slowly conducting APs. In the former, it is helpful to analyze the QRS morphology in the lateral precordial leads. In patients with subtle preexcitation due to a left free-wall AP, a “septal” Q wave is not inscribed in the lateral precordial leads (Figure 76-3). The left-sided location of the pathway allows ventricular activation to proceed over the AV node more than would be possible with right-sided pathways. Right-sided APs are associated with a greater degree of preexcitation. In patients with an equivocal ECG, administration of adenosine is helpful in unmasking preexcitation. Figure 76-3 A, An example of subtle preexcitation. Slight slurring of the QRS complex upstroke (arrow) and a short PR interval are consistent with ventricular preexcitation. Also note that the QRS complex in the lateral precordial leads lacks a “septal” Q wave. B, A post-ablation ECG obtained from the same patient as in Figure 76-3, A. After elimination of the left lateral AP, the delta wave is no longer present, and the PR interval is longer (dashed arrow). Also, a small Q wave in lead V6 (solid arrow) reflects normal septal activation.
Preexcitation, Atrioventricular Reentry, and Variants
Definitions
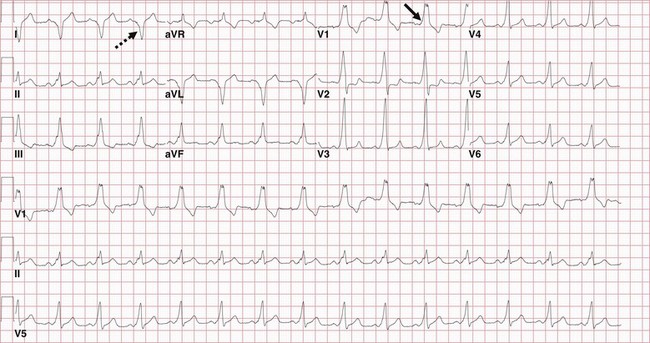
The electrocardiogram (ECG) shows sinus rhythm, a short PR interval, and slurred upstroke of the QRS (delta waves, arrow). The positive delta waves in lead V1 and the negative delta waves in lead I (dashed arrow) point to an insertion along the free-wall aspect of the mitral annulus. In addition, the positive delta waves in the inferior leads are consistent with a lateral or anterolateral accessory pathway (AP). Paper speed = 25 mm/s. (See next.)
Presentation and Evaluation
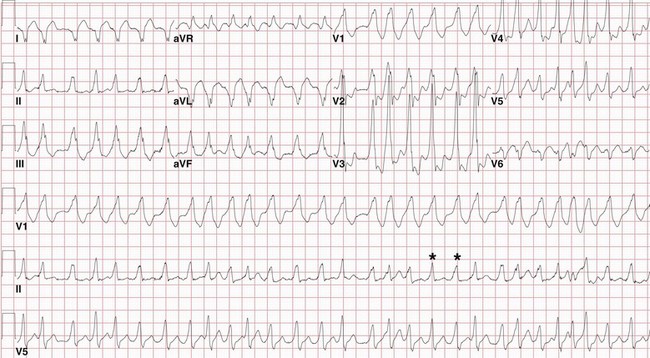
This ECG was recorded from the same patient as in Figure 76-1. He presented to the hospital with palpitations and near-syncope. Note the wide-complex QRS morphology, which is very similar to that during sinus rhythm (Figure 76-1). The QRS morphology is not uniform (asterisks), reflecting a varying degree of fusion of ventricular activation over the AP and the specialized conduction system. The ventricular rate is irregular and at times is as short as 200 ms. The AP was successfully ablated at the lateral mitral annulus. Paper speed = 25 mm/s.
Management
ECG Characterization
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
