INDICATIONS/CONTRAINDICATIONS
Indications
Nonanatomic limited resection of lung parenchyma is one of the most commonly performed thoracic procedures, with the majority being done by video-assisted thoracic surgery (VATS) wedge resection using surgical stapling devices. An alternative method of precision excision of pulmonary lesions was described by Perelman and Cooper in the 1980s, using electrocautery to resect lesions while preserving as much lung parenchyma as possible. Since then, other devices such as the monopolar floating ball (which provides a continuous flow of electrically conductive saline to the interface between a metal electrode and tissue) and bipolar sealing forceps (using electrothermal, radiofrequency, and ultrasonic energy) have been developed.
Lasers are being used with increasing frequency to perform precision excision (Table 19.1). Lung parenchyma has a water content of 80%, low tissue density, low heat capacity, and high air content. This makes the lung tissue suitable for laser applications. The ideal laser requires coagulation capability in addition to cutting properties to achieve hemostasis and to seal air leaks. Laser sealing is achieved by progressive collapse and shrinking of alveoli producing a thick, multilayer, airtight membrane. In contrast to electrical or ultrasonic energy, which is immediately converted to heat by the resistance of the tissue, lasers are able to penetrate deeper lung tissue to achieve coagulation. Coagulation of tissue up to a margin of 4 to 5 mm may also eradicate grossly undetectable microscopic foci of malignancy.
CO2 lasers, Er:YAG (erbium-doped yttrium aluminum garnet) lasers, and holmium lasers were used in the past on lung tissue but have been shown to possess absorption-dominant characteristics resulting in tissue vaporization with insufficient coagulation, and therefore not suitable for use in lung resections. The 1,064-nm Nd:YAG (neodymium-doped yttrium aluminum garnet) laser shows low absorption and high scattering in tissue and is also not ideal. More recently the 1,318-nm Nd:YAG laser has shown promise with balanced cutting and coagulation capability (Fig. 19.1). This laser creates a strong lung tissue shrinkage layer providing reinforcement of the coagulation zone and additional sealing of potential air leaks (Fig. 19.2). Defocused irradiation of lung tissue with the 1,318-nm Nd:YAG laser has been shown to create a sealed surface capable of withstanding ventilation pressure of up to 25 cm H2O. Shrinkage and thickening of the tissue can also be beneficial in management of lungs with bullous disease. The defocused Nd:YAG laser beam when applied to emphysematous tissue causes thickening of the surrounding lung tissue, and this can form a more secure closure of the blebs than staplers alone. Applying the beam over small- to moderate-sized blebs can also result in collapse and obliteration without air leak or the need for further intervention.
TABLE 19.1 Use of Lasers in Thoracic Surgery
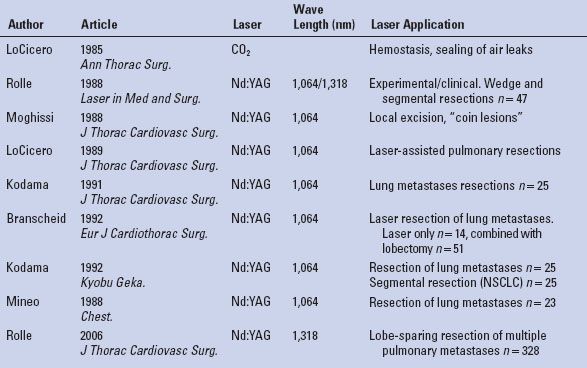
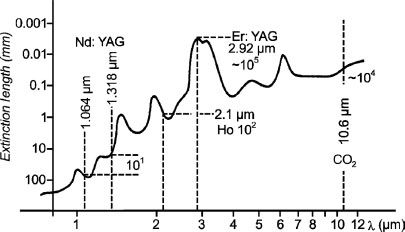
Figure 19.1 Absorption of various lasers in water.
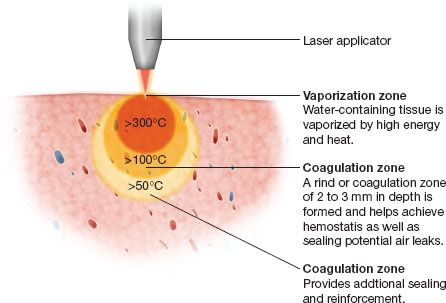
Figure 19.2 Effect of laser irradiation on lung tissue.
Precision excision techniques are used in situations where standard wedge excision is difficult, or maximal preservation of lung parenchyma is important. The raw lung surface is left charred with the defect sutured or left open. The latter is preferred to maintain as much functional lung parenchyma as possible, with minimal deformity or damage to the adjacent lung tissue.
Examples where this technique is especially useful include the following:
Resection of lesions in patients with limited pulmonary reserve.
Metastasectomy of multiple lung lesions.
Resection of deep-seated lesions where placement of staplers is precluded by the thickness of the lung tissue.
Lesions that traverse fissures.
Lesions located near a major bronchus or vessel, requiring a margin of tissue, without injury to these adjacent structures.
Contraindications
Clinical judgment should be exercised when evaluating patients for precision excision. With improvements in devices used for precision excision and demonstration that it can be performed safely with a low rate of complications, the indications for its use are being expanded. Contraindications to precision excision are relative but include the following.
Severe cardiopulmonary failure
Hemodynamic instability
Pleural adhesions or prior pleurodesis
Inability to tolerate single-lung ventilation (if using VATS)
Extrapulmonary metastasis
Coagulopathy
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Patients that are being considered for parenchyma-sparing cautery resections will often have marginal reserve, and a thorough assessment of their overall functional status is necessary. This includes a careful evaluation of cardiovascular risk, pulmonary function, exercise tolerance, and other factors such as nutritional status and the presence of other comorbidities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


