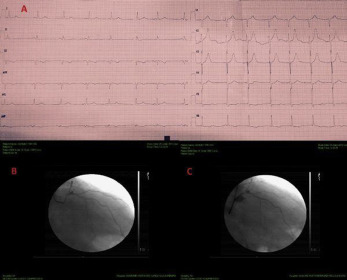
The clinical presentation of carbon monoxide (CO) intoxication includes dizziness, headache, and weakness, progressing in severe cases to confusion, loss of consciousness, and death. Carbon monoxide may cause hypoxia by preventing the delivery of oxygen to tissues because it binds to hemoglobin with a 250-fold greater affinity than oxygen to form carboxyhemoglobin. The central nervous and cardiovascular systems are most susceptible to hypoxia associated with carbon monoxide intoxication, and neurologic sequelae are among the most common problems that occur after exposure to carbon monoxide. Herein we report a case of acute non-ST elevation myocardial infarction and acute cerebrovascular ischemia in a same patient at the same time induced by acute CO intoxication. A 73 years old man admitted to our hospital emergency department with typical chest pain and right hemiparalysis. His carboxyhemoglobin level was 14.1%, hemoglobin concentration was 11.7 g/dL, and pH was 7.2. His peak troponin I level was 46.9 ng/mL. His magnetic resonance image of the brain showed that diffusion restriction in the left pre-central gyrus. There were minimal ST depressions in the leads of D3-aVF and V5-6 on his electrocardiogram. An 80% occlusion in left anterior descending artery (LAD) after first septal branch was shown in coronary angiography therefore we put a drug-eluting stent in LAD. We also planned antiaggregant and anticoagulant treatment with a specific neurologist. His all symptoms were fully regressed after the medical treatments. To the best of our knowledge, there are only a few reported cases of the combination acute myocardial infarction and cerebrovascular ischemia after CO intoxication.