Chapter 33
Postoperative Management
Giuseppe Papia
Vascular surgery patients remain at high risk for the development of complications in the postoperative period because of the complexity of their surgical procedures and their preoperative comorbidities. This chapter addresses management issues in the postoperative period with an emphasis on issues in the intensive care unit (ICU) and specially monitored high-dependency step-down units.
Postoperative Triage
An important aspect of postoperative medical care involves identifying patients at highest risk for postoperative complications and triaging them to the appropriate care environment. The safest postoperative environment for patients undergoing vascular surgical procedures is determined by the preoperative medical comorbid conditions (see Chapters 28, 30, 31, 37, 39, 40, and 41), the inherent risks of the type of operation performed, and the ability to maintain intraoperative and postoperative homeostasis of the patient. Emergency operations, such as those for a ruptured abdominal aortic aneurysm (AAA), have increased risk for mortality.1
Admission to the Intensive Care Unit and High-Dependency Step-Down Unit
The need for invasive hemodynamic monitoring and observation remains the most common criterion for admission of selected patients to an ICU or step-down unit. The main distinction between these two environments in most institutions is the severity of critical illness and need for invasive positive pressure ventilation. These environments can provide patients the following: decreased myocardial oxygen demand through expeditious rewarming, effective fluid resuscitation, effective analgesia, meticulous control of hemodynamics, and careful monitoring and appropriate nursing care to aid in the early diagnosis and treatment of complications. In a cohort study of patients after elective aortic surgery, Lawlor et al2 demonstrated that care in an ICU decreased mortality in patients with preoperative severe coronary artery disease defined as an ejection fraction of less than 40%, congestive heart failure, or New York Heart Association class III or IV angina. Consideration of direct admission to the ICU should also be given to patients with significant chronic obstructive pulmonary disease (COPD, defined as forced expiratory volume in 1 second of less than 1 L) and those who are dialysis dependent or have a need for continuous renal replacement therapy. Hemodynamically unstable patients (systolic blood pressure <90 mm Hg or inotropic support at the end of the operation), intubated patients with ongoing need for ventilatory support, those with clinically significant perioperative cardiac ischemia, patients with pulmonary artery catheters, patients with spinal drains, patients with hypothermia (temperature <35° C), and those who required massive transfusion of blood products (>3 L) during the procedure should be admitted to the ICU.
Selective use of high-dependency step-down units and rationing of ICU resources can be safe and cost-effective with appropriate patient risk stratification.3,4 Each patient must be individualized according to preoperative comorbid diseases, perioperative hemodynamic stability, and surgical procedure performed. Patients undergoing less invasive vascular procedures associated with fewer fluid shifts and lower surgical morbidity can be safely managed in a step-down unit. This is the case with patients undergoing peripheral arterial bypass, elective repair of infrarenal AAAs, and carotid endarterectomy. Several scoring models predicting risk in vascular patients have been studied and validated as predictors of high-risk patients undergoing vascular surgery.5
Organizational Structure of the Intensive Care Unit
The organizational structure of the ICU, independent of a patient’s medical factors, has a direct impact on outcomes.6–11 In looking at outcomes after abdominal aortic surgery, Pronovost et al7,12 have shown a relationship between increased in-hospital mortality and the absence of a full-time ICU director, less than 50% of ICU attending physicians certified in critical care, no daily rounds by an ICU physician, and decreased ICU nurse-patient ratio in the evening (<1 : 2). In patients undergoing abdominal aortic surgery, intensivists not making routine ICU rounds is associated with an increase in hospital mortality (odds ratio [OR], 3.0; 95% confidence interval [CI], 1.9-4.9), cardiac arrest (OR, 2.9; 95% CI, 1.2-7.0), acute renal failure (OR, 2.2; 95% CI, 1.3-3.9), septicemia (OR, 1.8; 95% CI, 1.2-2.6), platelet transfusion (OR, 6.4; 95% CI, 3.2-12.4), and reintubation (OR, 2.0; 95% CI, 1.0-4.1). Dang et al6 also demonstrated that ICUs with decreased nurse staffing had increased rates of cardiac and respiratory complications after abdominal aortic surgery.
Hemodynamics and Pressure Monitoring
Monitoring is required to intervene in abnormal physiology with the goal of improving outcomes. However, even patients with normal hemodynamic parameters may have inadequate organ perfusion.13 Distributive hypoxia is a state that results from inadequate oxygen delivery to tissues, exacerbated by increased metabolic demands, with resultant multiorgan dysfunction.14 Indicators of organ perfusion to guide resuscitation15 include blood pressure, heart rate, central venous pressure (CVP), pulmonary capillary wedge pressure, cardiac output,16 urine output, blood lactate concentration, tissue carbon dioxide levels, base deficit, mixed venous oxygen levels, and mixed venous carbon dioxide levels.15,17 The key to interpreting and managing these indicators appropriately is to follow trends over time rather than individual measurements.
Central Venous Catheters and Central Venous Pressure
Central venous catheters are used primarily to infuse fluids, to administer vasoactive drugs, and to assess intravascular volume. The most common sites for placement of central venous catheters are the internal jugular veins, subclavian veins, and femoral veins. To measure CVP, internal jugular or subclavian central venous catheters must be positioned with the catheter tip in the distal segment of the superior vena cava. More distal placement in the right atrium is associated with potential risk for erosion, perforation, and cardiac tamponade. CVP measures right atrial pressure, providing an estimation of preload. This measurement, however, is inaccurate in patients with COPD or in those with valvular heart disease. Femoral lines are good for resuscitation but not for CVP measurements because of the effect of intra-abdominal pressure on measurements.
The transducer must be zeroed at the level of the midaxillary line, and normal values of CVP are between 6 and 12 mm Hg. In patients being managed with positive pressure ventilation, CVP should be measured at end-expiration, when pleural pressure in the chest is approximately zero.18 The addition of positive end-expiratory pressure (PEEP) in a ventilated patient is another important consideration in measuring pressure in the chest. In normal lungs and with low levels of PEEP (between 5 and 8 cm H2O), intrapleural pressure, which affects CVP, is only slightly affected.18 The effect on CVP of high levels of PEEP (>12 to 15 cm H2O) when the lungs are probably not compliant is unclear.19 High levels of PEEP prevent backflow of fluid outside the chest to the heart, thus decreasing venous return. If sudden changes in CVP occur, one should consider a cardiorespiratory cause, such as pneumothorax or cardiac tamponade. Further discussion of CVP monitoring can be found in Chapter 32.
Peripheral Arterial Lines
Peripheral arterial catheters are the “gold standard” for direct assessment of systolic blood pressure, and they allow direct vascular access for blood sampling. Complications include bleeding, hematoma, line-related infection, thrombosis, and, rarely, limb ischemia.20 These complications occur to varying degrees, depending on the cannulation site. The most common site for cannulation is the radial artery, followed by the femoral artery, axillary artery, brachial artery, and, less commonly, dorsalis pedis and ulnar arteries. The radial artery and the femoral artery have similar cannulation complication rates,21 and some prefer the femoral artery as the primary cannulation site because of ease of insertion. The most common complication of radial artery cannulation is temporary arterial occlusion, which occurs approximately 20% (1.5% to 35%) of the time, but the occlusion is temporary in most and rarely causes acute ischemia.20 In contrast to the radial artery, cannulation of the femoral artery is associated with a higher risk of bleeding (1.58% vs 0.53%) and pseudoaneurysm (0.3% vs 0.09%) but a lower risk of thromboembolism.20 Cannulation of the axillary artery has a complication rate similar to that at other sites, and it may be the only site available for arterial access in some patients. In the ICU, however, it is not commonly used because of lack of familiarity with the approach and the potential, albeit unproven, risk for carotid embolization.20 The level of the transducer relative to the pressure being measured will determine the measured value of the arterial pressure, thus making its position critical for obtaining an accurate measurement. The standard level is the midpoint of the right atrium, approximately 5 cm below the sternal angle in the midaxillary line. This is the area where the preload pressure of the heart is determined.22
The distance of the measuring catheter from the heart, the length and compliance of the tubing, and the presence of air bubbles affect systolic and diastolic measurements in the system. These variables affect systolic and diastolic pressure proportionately in opposite directions and have no net effect on the measurement of mean arterial pressure (MAP). For this reason, measurement of MAP is a more accurate reflection of mean aortic pressure. MAP is manually calculated with the formula MAP =  [(2 × diastolic blood pressure) + systolic blood pressure]. Electronic monitoring systems, however, measure MAP as the area under the pulse wave, often averaged over three or more cycles.
[(2 × diastolic blood pressure) + systolic blood pressure]. Electronic monitoring systems, however, measure MAP as the area under the pulse wave, often averaged over three or more cycles.
Pulmonary Artery Catheters
Pulmonary artery catheters provide central hemodynamic measurements, waveform tracings, and specific blood gas calculations such as mixed venous oxygen and carbon dioxide saturation (also see discussion of pulmonary artery catheter use in Chapter 32). Pulmonary artery catheters were initially used to assess and to treat patients with acute myocardial infarction (MI); however, the use of pulmonary artery catheters has declined significantly because several randomized trials have failed to demonstrate a reduction in mortality.23–25 Pulmonary artery catheters are typically inserted in the ICU in situations in which the clinician believes that measuring cardiac output, cardiac pressure, and mixed venous oxygen saturation will aid in guiding therapy and for direct assessment of the effect of and response to various treatments, such as fluids and vasopressors.26 Included in this category are patients in cardiogenic or refractory shock and patients in whom right ventricular dysfunction, such as right ventricular infarction, is suspected.18,27 Pulmonary artery catheters may induce arrhythmias, which are usually transient and not life-threatening.28 Left bundle branch block is a relative contraindication to the use of pulmonary artery catheterization because it can induce a temporary right bundle branch block and the potential for subsequent complete heart block.28 Other catheter-related complications include catheter knotting, pulmonary artery rupture, catheter fragmentation, and cardiac rupture secondary to forceful insertion. Long-term placement, more than 72 to 96 hours, can also lead to thrombosis and infection.
Echocardiography
Echocardiography is used to assess cardiac function by measuring ventricular contractility, chamber size, valve function, and flow.29,30 Global assessment of ventricular function with transthoracic echocardiography can be helpful in guiding hemodynamic management because one can easily differentiate between left and right ventricular dysfunction and adjust treatment appropriately.31 For instance, a patient with a poorly functioning left ventricle may benefit from an inotropic agent, whereas the presence of a hyperdynamic left ventricle and evidence of tissue hypoxia may indicate the need for fluid challenge and vasopressors.29 Echocardiography is helpful in the case of normotensive shock in a patient who has been adequately fluid resuscitated where it may be necessary to use afterload-reducing agents such as nitroglycerin.32 Calculation of ejection fraction, pulmonary artery pressure, and cardiac output is also possible, but specific expertise is required, and such measurements may not be reliable in ICU settings.31
Transesophageal Doppler ultrasound is a noninvasive modality for measuring cardiac output.33 Cardiac output is calculated by using the diameter of the descending aorta, the distribution of flow to the descending aorta, and the measured flow velocity of blood.15 The accuracy of the calculated cardiac output may be affected by the position of the ultrasound probe, which is inserted blindly in the esophagus. Poor positioning of the probe most commonly results in an underestimation of the cardiac output.15
Intra-Abdominal Pressure
Abdominal compartment syndrome is defined as clinically relevant organ dysfunction caused by intra-abdominal hypertension. Intra-abdominal pressure (IAP) is the steady-state pressure concealed within the abdominal cavity. For most critically ill patients, an IAP of 5 to 7 mm Hg is considered normal.34 Morbidly obese and pregnant individuals may have chronically elevated IAP without adverse consequences. Intra-abdominal hypertension is defined as IAP in excess of 12 to 20 mm Hg.35,36 Abdominal perfusion pressure is calculated as MAP minus IAP. Elevated IAP may reduce blood flow to the abdominal viscera. Abdominal compartment syndrome is diagnosed by the combination of intra-abdominal hypertension and evidence of organ malperfusion. Specifically, it is a constellation of symptoms consisting of new attributable organ dysfunction, such as cardiovascular (decreased cardiac output), respiratory (high peak airway pressure), and renal (oliguria) malperfusion, in the context of sustained IAP of 20 mm Hg or higher.35 Patients at increased risk for abdominal compartment syndrome are those who received large volumes of fluid for resuscitation (>10 L of crystalloid, >5 L of colloid) or transfusion of more than 10 units of packed red blood cells (PRBCs) during a 24-hour period.36
IAP is most commonly measured by the intravesicular technique.37 An indwelling bladder catheter is connected to a pressure transducer. A defined volume of fluid (25 to 50 mL of normal saline) is instilled into the catheter and used to distend the bladder and eliminate bladder wall coaptation.36 Volumes greater than 50 mL falsely elevate IAP values. IAP is then measured at end-expiration with the patient in the supine position and the manometer or other pressure measuring system at the level of the symphysis pubis. Another technique of IAP measurement uses a nasogastric or orogastric tube.38 This technique involves a lower risk for sepsis secondary to iatrogenic urinary tract infection as a result of catheter manipulation, but it is a more cumbersome method and rarely used. The timing of IAP monitoring and the frequency of monitoring are not standardized, but the highest risk for the development of abdominal compartment syndrome is during and shortly after resuscitation. The main reason for monitoring of IAP is that early recognition and treatment of abdominal compartment syndrome appear to improve survival.36
Cardiovascular Complications
Hypertension
Hypertension is common after surgery and may be caused by hypoxia, hypercapnia, hypervolemia, hypothermia, gastric or bladder distention, agitation, and pain. Furthermore, a common cause of postoperative hypertension is simply neglecting to restart preoperative antihypertensive medications. Sedation, analgesia, and rewarming often resolve most cases of mildly elevated blood pressure. However, hypertension increases myocardial oxygen consumption and can potentially cause myocardial ischemia. In addition, in the immediate postoperative period, it may contribute to increased bleeding from raw surfaces or through vascular anastomoses. After all possible causes have been evaluated and addressed, drug treatment may be considered. In general, blood pressure treatment targets should center on systolic blood pressure values 20 mm Hg above or below preoperative pressure.39 Deviations in MAP greater than 20% from preoperative values should also be treated.40,41 Several agents may be used, and the surgeon should become familiar with a few for an effective and safe approach to hypertensive patients in the postoperative period. Nitrates, beta blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers, and vasodilators are the most common classes of drugs used (see Chapter 30).42
Hypertensive crisis is acute end-organ damage (heart, brain, retina, and kidney) associated with systolic blood pressure higher than 179 mm Hg or diastolic blood pressure higher than 109 mm Hg. In the absence of evidence of end-organ damage, these elevations in blood pressure constitute what are called hypertensive emergencies.43 When hypertensive emergencies are diagnosed, short-acting intravenous antihypertensive agents should be used; the reduction in blood pressure should occur within 1 hour in hypertensive crisis and within 24 hours in hypertensive emergencies.9 The goal is to reduce the patient’s diastolic blood pressure to less than 110 mm Hg during a period of 30 to 60 minutes.44 Hypertensive patients in these circumstances will manifest natriuresis, which causes intravascular fluid depletion requiring fluid administered along with antihypertensive medications. Several agents can be used in hypertensive emergencies; one of the most common and effective is labetalol because it is a combined α1-adrenergic and nonselective β-adrenergic receptor blocker.45
Hypotension
Hypotension is dangerous and is associated with an increased risk for end-organ dysfunction (MI, cerebrovascular events, and renal failure) and possibly bypass graft thrombosis. Common causes of hypotension after surgery are hypovolemia, cardiac dysfunction, and a diffuse vasodilatory state with or without sepsis. The two management strategies for correction of hypotension involve administration of fluids and vasoactive agents. A fluid challenge should be the first line of treatment of postoperative hypotension. Surgical bleeding should be excluded as a cause to prevent delays in returning the patient to the operating room.46
When administering fluids for resuscitation, one must determine whether the patient is on the ascending portion of the Frank-Starling curve and will benefit from a fluid challenge. If the patient is on the flat portion of the curve, fluid loading will only increase tissue edema and worsen tissue dysoxia with little effect on cardiac output.15 A large pulse pressure–stroke volume ratio (>10%:15%) is indicative of hypovolemia and predictive of volume responsiveness.15 A fluid challenge in these circumstances will increase preload and subsequently increase stroke volume.47 Similarly, in patients with a pulse pressure variation greater than 12%, fluid challenge is likely to have a positive effect on cardiac output.48 If the hypotension does not respond to fluid resuscitation, cardiac output must be optimized through pharmacologic means. Short-acting peripheral vasoconstrictors, such as phenylephrine and dopamine, are readily available on crash carts and can be given peripherally and titrated to effect. Once patients have adequate central intravenous access, dopamine should be switched to more definably titratable vasopressors.
In cardiogenic shock, peripheral vasoconstrictors may increase myocardial workload and dysfunction. In this setting, inotropic agents may be necessary to increase cardiac output. Patients in cardiogenic shock secondary to acute MI have mortality rates higher than 50%.49 In these situations, volume must be optimized, rhythm must be controlled, and beta agonists should be administered to enhance contractility.50 Finally, intra-aortic balloon pump counterpulsations may be necessary to aid the heart in generating cardiac output when pharmacologic agents fail. Beta blockers and calcium channel blockers have a negative inotropic effect and are relatively contraindicated in this setting.
Arrhythmias
Patients with preexisting structural heart disease are at highest risk for postoperative arrhythmias.51 Common triggers for postoperative arrhythmias are hypoxia, hypercapnia, acid-base imbalances, electrolyte abnormalities, and myocardial ischemia. Treatment must focus on predisposing factors, and the goal should be hemodynamic stabilization, control of the ventricular response, and restoration of rhythm.51
Tachyarrhythmias
The most common tachyarrhythmias are sinus tachycardia, atrial fibrillation (AF), ectopic atrial tachycardia, junctional tachycardia, multifocal atrial tachycardia, atrioventricular (AV) nodal reentry tachycardia, ventricular tachycardia (VT), and ventricular fibrillation. Tachyarrhythmias that traverse the AV node can often be controlled pharmacologically by altering conduction through the AV node.51 Tachyarrhythmias that are conducted by accessory pathways and ventricular tachyarrhythmias are more difficult to control pharmacologically than those that transverse the AV node. Supraventricular tachyarrhythmias are common after surgery, with an incidence of approximately 4% to 13%,51 and after AAA repair, with an incidence of 3.2%.52 Short bursts of atrial tachycardia do not require treatment. It is important, however, to correct any underlying causes, such as electrolyte imbalances. For sustained atrial tachyarrhythmia in a hemodynamically stable patient, the rate may be slowed with beta blockers or calcium channel blockers. Caution should be exercised with these agents, however, when they are used in patients with poor left ventricular function or congestive heart failure. Alternatively, in monitored settings, treatment can be switched to intravenous amiodarone. In stable patients with nodal reentrant rhythms, adenosine (6 to 12 mg intravenously) can also be used instead of beta blockers or calcium channel blockers. If patients are hemodynamically unstable, they should be electrically cardioverted regardless of the type of atrial tachyarrhythmia.
Ventricular tachyarrhythmias are also managed according to their duration and hemodynamic consequences. In the presence of coronary artery disease, these rhythms are ominous. Furthermore, the presence or absence of structural heart disease has prognostic significance,51 and it is important when treatment of runs of premature ventricular contractions and nonsustained VT is being considered. Prompt evaluation and treatment of predisposing factors, such as hypokalemia, hypomagnesemia, hypoxia, and myocardial ischemia, are important to prevent sudden death. In addition, unstable VT is an indication for immediate electrical defibrillation. In contrast, hemodynamically stable monomorphic VT should be treated with antiarrhythmics such as intravenous amiodarone followed by prompt cardiac evaluation.
Polymorphic VT and ventricular fibrillation occur most commonly in the setting of acute MI and can rapidly lead to hemodynamic instability. These arrhythmias are also treated with urgent defibrillation and intravenous antiarrhythmics. Polymorphic VT with prolonged QT intervals is called torsades de pointes. The most common cause of this rhythm is drug related or QT prolongation secondary to electrolyte abnormalities. Intravenous magnesium should be given empirically for suspected torsades de pointes. Positive chronotropic agents such as isoproterenol or temporary overdrive pacing to shorten the QT interval can also be used.
Atrial Fibrillation
AF is the most common arrhythmia encountered in the postoperative period; it affects 10% of patients undergoing major noncardiothoracic operations.53,54 Onset is often within the first few days after the operation, and AF is associated with increased 30-day postoperative mortality, increased ICU stay, and increased overall hospital length of stay. Common risk factors for the development of AF include advanced age, male gender, valvular heart disease, and previous history of AF.53 AF can be precipitated by hypokalemia, hypomagnesemia, volume overload, withdrawal of beta blockers or angiotensin-converting enzyme inhibitors, COPD, obesity and obstructive sleep apnea, and infections, especially pulmonary infections.53,55,56 A rapid heart rate limits ventricular filling, and loss of the atrial component of the cardiac cycle, the so-called atrial kick, decreases left ventricular stroke volume by 20% to 35%.57 This is especially important in patients with diastolic dysfunction and dilated left ventricles, whose cardiac output is volume dependent.58
Treatment focuses on controlling the heart rate, restoring normal sinus rhythm, and preventing thromboembolic complications.58 Patients who are hemodynamically unstable, who have pulmonary edema, or who have ongoing chest pain should undergo urgent electrical cardioversion. Hemodynamically stable patients should have their heart rate pharmacologically controlled with beta blockers, amiodarone, digitalis, or calcium channel blockers. Chemical cardioversion can also be used in hemodynamically stable patients, and a third of patients will convert to normal sinus rhythm with amiodarone loading alone.59
Before electrical cardioversion, one must consider the patient’s risk for thromboembolic complications. If the patient has been in AF for longer than 48 hours or for an unknown period, intracardiac thrombus must be excluded.60 This is obviously not feasible in the event of acute hemodynamic instability, and one should proceed with electrical cardioversion to stabilize the patient and subsequently monitor for thromboembolic complications. If an intracardiac thrombus cannot be excluded and the patient is hemodynamically stable, the safest course of action is anticoagulation with unfractionated heparin before cardioversion.53
Bradyarrhythmias
Bradyarrhythmias are not generally a diagnostic challenge, and treatment options are straightforward. Those associated with sinus node dysfunction are sinus bradycardia, sinus pause, sinoatrial block, and sinus arrest.61 Postoperatively, these rhythms are most often due to increased vagal tone and myocardial ischemia. If the bradyarrhythmia is transient and not associated with hemodynamic instability, it does not require treatment. Treatment of sustained bradyarrhythmias, and hemodynamic compromise, is with antimuscarinic agents such as atropine. If there is no response with continued bolus doses of atropine, the patient must be paced either externally or with a temporary transvenous pacer.
Postoperative Myocardial Infarction
Diagnosis
MI is the most common cause of cardiac complications and mortality in patients with peripheral vascular disease.46,62–65 The three modes of detecting clinically meaningful postoperative cardiac ischemia are symptoms, the electrocardiogram (ECG), and evaluation of myocardial enzymes. Symptoms elicited from the patient, often in the form of anginal chest pain, are not a frequent manifestation of postoperative myocardial ischemia but are more commonly found in those with acute coronary syndrome.66 In the postoperative period, these symptoms are also difficult to distinguish from distracting postoperative pain and are influenced by the concomitant use of analgesia and anesthetics. The presence of ST-segment changes on the ECG may indicate an MI. However, after major vascular surgery, approximately a third of patients will have ST changes on the ECG in the absence of clinically significant myocardial ischemia.67 Regardless, the presence of such changes correlates with an approximately 9- to 16-fold increased risk for MI and death.67 The third method of diagnosing postoperative MI is through the detection of myocardial proteins released into circulation as a result of myocardial cellular injury. The most common enzymes evaluated are the MB isoenzyme of creatine kinase (CK-MB) and the myocardial-specific cardiac protein troponin I.68 In vascular surgery patients, increased cardiac troponin I levels in the absence of clinical symptoms have also been demonstrated to be useful in the risk stratification of postoperative patients for cardiac morbidity.68 Elevated levels after major vascular surgery are associated with increased risk for perioperative MI and increased risk for mortality at 6 months.
ST-Segment Elevation Myocardial Infarction
ST-segment elevation MI (STEMI) is most commonly caused by acute rupture of atherosclerotic plaque and thrombosis of the involved coronary arteries. For this diagnosis to be made, the ECG must show ST-segment elevation of at least 0.1 mV (1 mm) in two consecutive leads.69 In patients with preexisting left bundle branch block, diagnosis of STEMI is difficult. Biochemically, CK-MB levels are elevated 3 to 12 hours after infarction, peak at 24 hours, and can be elevated for 3 days. Cardiac troponin levels can be detected 4 to 12 hours after infarction, peak at 12 to 48 hours, and can remain elevated for 1 week.
Treatment involves rapid resuscitation with administration of supplemental oxygen, afterload-reducing agents, antiplatelet therapy, anticoagulation with unfractionated heparin (if at low risk for bleeding), and urgent reperfusion therapy with either fibrinolysis or primary percutaneous coronary intervention (PCI). Postoperatively, fibrinolysis may be relatively contraindicated, but this decision must be individualized to the patient according to the extent of surgery and time after the operation. For clinically significant ischemia and for patients in cardiogenic shock in the postoperative period, urgent PCI and revascularization are indicated. Primary PCI is associated with primary patency rates of greater than 90%. Emergency coronary artery bypass surgery is reserved for patients who have failed to respond to PCI or fibrinolysis or who have a complication that requires surgery, such as ventricular septal rupture, cardiac rupture, or severe mitral valve insufficiency.70 Beta blockers should also be started unless patients are hypotensive or bradycardic, are in congestive heart failure, have advanced AV block, or have reactive airway disease. In addition, an angiotensin-converting enzyme inhibitor should be started in the first 24 hours after infarction. In the long term, patients also benefit from treatment with statins.
Non–ST-Segment Elevation Myocardial Infarction
Non–ST-segment elevation MI (non-STEMI) is characterized by the presence of biomarkers indicative of myocardial injury in the absence of ST elevation on the ECG. The key difference from STEMI is myocardial ischemia in the absence of significant coronary obstruction, such as occurs with acute plaque rupture. The myocardial ischemia in this setting is due to a transient reduction in coronary blood flow that causes an imbalance in myocardial oxygen supply and demand, often with shortness of breath and decompensated heart failure. The ECG can demonstrate nonspecific T-wave inversion or ST depression, and the key to diagnosis is the presence of circulating biomarkers (CK-MB, troponin I, troponin T) indicative of myocardial cellular necrosis.71 Mortality risk is directly proportional to troponin levels.72
Treatment is medical and centered on optimizing myocardial oxygen delivery and demand and preventing reinfarction and death.71 Supplemental oxygen should be administered, and pharmacologic agents to decrease preload and cardiac afterload are given. Treatment can be thought of as the ABCs (acetylsalicylic acid, angiotensin-converting enzyme inhibitor, beta blockers, and cholesterol lowering). Administration of unfractionated heparin is also associated with a mortality benefit,71 but its use must be balanced with the risk of bleeding. Statin therapy should also be instituted and treatment continued in the long term. In the setting of ongoing chest pain, the most recent American College of Cardiology/American Heart Association guidelines recommend the use of sublingual nitroglycerin if the systolic blood pressure is higher than 90 mm Hg and the heart rate is not less than 50 beats/min or more than 100 beats/min. If further analgesia is needed after nitroglycerin is given, morphine sulfate or meperidine can be used.73
Pulmonary Management
Respiratory insufficiency can be divided into either oxygenation failure or ventilation failure. Oxygenation failure is typically associated with hypoxia and ventilation failure with hypercapnia. Management of patients with acute respiratory failure and acute respiratory distress syndrome is discussed extensively in Chapter 40. The following comments focus on pulmonary support provided for the mechanically ventilated patient.
Ventilatory Support
Mechanical Ventilation
Mechanical ventilators affect oxygenation by controlling airway pressure and fraction of inspired oxygen and affect ventilation by controlling tidal volume and respiratory rate. Patients are ventilated primarily in two modes: controlled and supported. In controlled ventilation, the ventilator initiates and delivers a set amount of tidal volume; in supported mode, the breath is initiated by the patient and supported by the ventilator. Ventilators may deliver either a fixed tidal volume with variable pressure (volume control) or a variable tidal volume at a fixed pressure (pressure control). The combination of these two general modes of ventilation (controlled versus spontaneous) with either of these two settings (volume control versus pressure control) accounts for the majority of modes with which patients are ventilated. Patients with hemodynamic instability or in severe respiratory distress should be placed on a controlled mode of ventilation to limit the patient’s work of breathing. Either volume control or pressure control ventilation is adequate, and practitioners should select the mode with which they are most familiar. Pressure support mode is generally used in patients who are more stable. Pressure support mode is also used as a weaning mode (discussed in the next section).
It is important to ventilate patients with use of a lung protective strategy to reduce ventilator-induced lung injury, which can occur through two main mechanisms. The first is referred to as volutrauma, which causes overdistention of alveoli due to high tidal volume and high alveolar pressure and can lead to barotrauma (pneumothorax, pneumomediastinum). The second main mechanism is caused by shear forces on alveolar endothelium.74 These shear stresses are created in alveoli by cyclic opening and closing, and the resultant injury is called atelectatic trauma.75 PEEP applied throughout the ventilatory cycle serves to stent alveoli open, which prevents atelectatic trauma and facilitates gas exchange. The ideal level of PEEP is unknown, but an accepted range, depending on the clinical situation, is 5 to 15 cm H2O.
In ventilating patients at increased risk for volutrauma, such as those with acute respiratory distress syndrome, a lung protective strategy using pressure control ventilation to reduce peak airway pressure is most appropriate (Fig. 33-1). In this mode, inspiratory time can also be lengthened to allow increased alveolar recruitment, and alveolar distending plateau pressure and transpulmonary pressure are to be kept below 30 cm H2O by use of tidal volumes that should not exceed 6 to 8 mL/kg ideal body weight.76 However, low tidal volume ventilation causes decreased clearance of carbon dioxide with associated respiratory acidosis, but this “permissive hypercapnia” and acidosis are well tolerated if the patient’s pH is above 7.2.77 One caveat is that permissive hypercapnia is contraindicated in patients with cerebral edema.
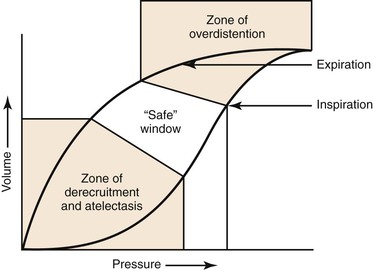
Figure 33-1 Protective ventilation. Ventilation of a patient with parameters on the left side of the pressure-volume curve places the patient at risk for atelectatic trauma, and ventilation of a patient with parameters on the right side of the curve places the patient at risk for barotrauma. (Redrawn from Froese AB: High-frequency oscillatory ventilation for adult respiratory distress syndrome: let’s get it right this time. Crit Care Med 25:906-908, 1997.)
Weaning
There are two main considerations in the weaning process. The first is weaning the support provided by the ventilator, and the second is removing the endotracheal tube (liberation from the ventilator). Patients should be assessed daily for readiness to be weaned, which can be done only after interruption of sedation.78 This method has been called “wake up and breathe.” Several randomized trials have revealed that weaning method influences ventilation duration.79,80 The traditional approach to weaning has been a progressive reduction in ventilatory support over time according to a protocol.81 A second technique is the use of spontaneous breathing trials without progressive withdrawal of ventilatory support, which may be associated with earlier extubation.82 With the traditional approach to weaning, patients are switched from a controlled to a spontaneous mode of ventilation, such as pressure support ventilation. The amount of ventilatory support and PEEP is then decreased according to oxygen saturation, respiratory rate, and tidal volume. If the patient is not ready for weaning, a decrease in tidal volume and an increase in respiratory rate will be noted.83 When a spontaneous breathing trial is used, patients are allowed to breathe spontaneously with little or no assistance. Most often, patients will be placed on minimal support (pressure support at 5 to 8 cm H2O, PEEP at 5 cm H2O) for 30 minutes to 2 hours. In a successful trial, the patient does not demonstrate respiratory distress (respiratory rate >35 for >5 minutes), desaturation (SaO2 <90% for >30 seconds), increase or decrease in heart rate (±20% for >5 minutes), systolic blood pressure higher than 180 mm Hg or lower than 90 mm Hg, or other signs of agitation and distress (paradoxical breathing, use of accessory muscles, diaphoresis).84
Indications for Extubation
Once patients are weaned from the ventilator and have successfully spent a prolonged time with minimal PEEP and on minimal pressure support, they can be assessed for the potential for extubation. If any indication for intubation exists, it is a contraindication to extubation. Contraindications to extubation are sedation, inability to protect the airway, presence of copious secretions, and lack of a cough reflex. Consideration must also be given to how difficult it would be to re-establish the airway if needed. Failure of extubation is associated with increased mortality and need for long-term ventilation.85 The harm of reintubation must be balanced by the harm created by prolonged mechanical ventilation. Reintubation rates of 10% to 15% are within the normal range in most ICUs.86
Tracheostomy
Tracheostomy relieves the patient of the portion of the work of breathing required to overcome the resistance of the endotracheal tube and the upper airway. It also allows better oral hygiene and secretion management and improves patient comfort. The major disadvantages of a tracheostomy are procedure-related complications, stomal complications, formation of a tracheoinnominate fistula, and formation of a tracheoesophageal fistula. Early tracheostomy within the first week in patients who are thought to require ventilation for more than 10 days facilitates weaning and is associated with shorter length of stay in the hospital.86 Jubran et al79 found that in patients who required prolonged mechanical ventilation, unassisted breathing through a tracheostomy resulted in shorter median weaning time compared with pressure support. However, in a retrospective observational study after abdominal and thoracoabdominal repair, Diedrich et al87 found that overall, tracheostomy correlated with worse outcomes but that patients with preexisting COPD who received a tracheostomy had improved survival.
Tracheostomy can be done either by an open surgical procedure or percutaneously. Percutaneous tracheostomy is as safe as open surgical tracheostomy, with the advantage that the patient does not require transport to the operating room, and operating room resources are thus conserved.88 Furthermore, no difference in long-term outcomes between percutaneous and open surgical tracheostomy has been shown.88 However, percutaneous tracheostomy is relatively contraindicated in patients who are hypoxic and have high PEEP requirements, in patients who are obese with short necks, in patients who are coagulopathic, and in those with recent (<10 days) anterior cervical spine fixation.89
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


