Bacterial
Viral
Mycoplasma
Age
Any
Mainly less than 2 years old
3–15 years old
Season
Year-round
Winter
Spring
Presentation
Sudden
Variable
Insidious
Fever
High
Variable
Variable
Tachypnea
Common
Common
Infrequent
Cough
Scarce
Frequent
Frequent and intense
Related symptoms
Chest pain
Acute rhinorrhea
Conjunctivitis
Exanthema
Arthralgias
Otalgia
Pulmonary examination
Condensation syndrome
Wheezing is frequently present
Condensation is sometimes present
Wheezing or condensation syndrome
Bronchial sounds, fine crackles
Bronchophony
Localized fine crackles
Clinical manifestations of pneumonia caused by Mycoplasma
Very frequent | Frequent | Regular frequency | Infrequent |
|---|---|---|---|
Cough | Headache | Myalgias | Conjunctivitis |
Odynophagia | |||
Fever | Lack of energy | Wheezing | Skin rush |
Otalgia | |||
Expectoration | Vomiting | ||
Acute rhinitis | |||
Crackles | Adenopathy | ||
Pharyngitis |
Extrapulmonary Manifestations
According to the subsets of patients studied, a variable percentage (10–20%) may have extrapulmonary compromise, which happens before, during, or after the pulmonary infection caused by MP, even when no symptoms are present. The most common ones are these:
Present in 15–20% of the patients and are self-limited. Among them we have the following skin conditions: maculous eruptions, morbilliform rashes, papulovesicular rash, urticaria, erythema nodosum, erythema multiforme major (Steven–Johnson), and bullous.
The first cause of extrapulmonary pathology. There have been cases of encephalitis, meningitis, aseptic meningoencephalitis, transverse myelitis, Guillain–Barré syndrome, peripheral neuropathy, cerebellar syndrome, and mental confusion. There is evidence that direct invasion and autoimmunity are the pathogenesis of neurological compromise.
- 1.
Hematological: Hemolytic anemia caused by cold agglutinins, autoimmune hemolysis, disseminated intravascular coagulation, thrombocytopenic purpura, and aplastic anemia.
- 2.
Articular: Mono- or polyarthritis (most frequent cause according to our experience in Chile).
- 3.
Cardiac: Myocarditis, pericarditis, arrhythmia, and heart failure.
- 4.
Renal: Acute nephritis, IgA nephropathy.
- 5.
Oculars: Conjunctivitis, anterior uveitis, iritis, hemorrhagic retinitis (very rare).

Interstitial-alveolar pneumonia . Chest X-ray of 9-year-old schoolchild shows a right lower lobe interstitial-alveolar image
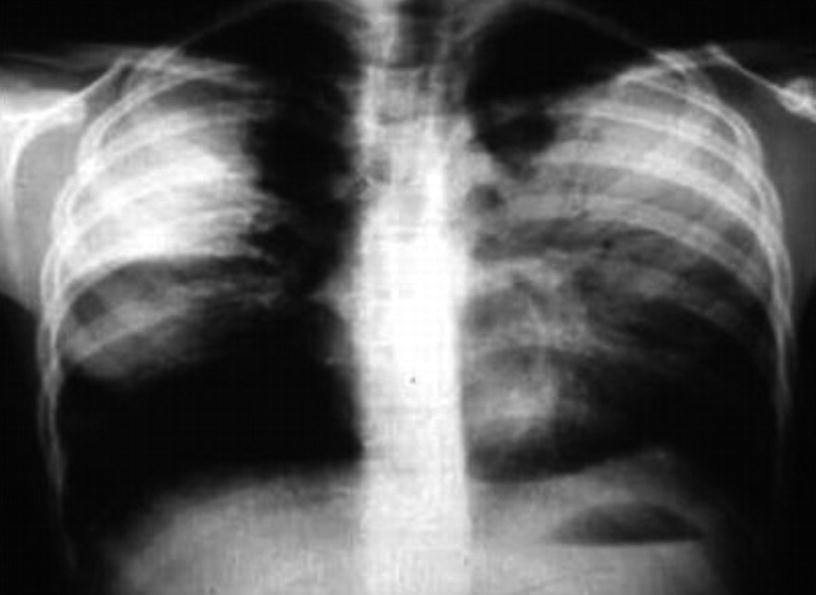
Alveolar pneumonia . Chest X-ray of 6-year-old schoolchild presenting with an extensive bilateral lobar consolidation (similar to that caused by Streptococcus pneumoniae)

Alveolar pneumonia and pleural effusion . Chest X-ray of 7-year-old schoolchild presenting with nasal bilateral condensation and left pleural effusion
Laboratory Diagnosis
Classic Diagnosis Techniques
Culture and serology using the complement fixation (FC) test have their limitations in clinical practice. Complex nutritional sources are required for isolation, and although the specificity of the procedure is total (100%), its sensitivity varies between 60% and 70%. MP grows slowly in culture media; it is a cumbersome microorganism, and visible colonies take from 2 to 6 weeks to appear. Consequently, most laboratories do not conduct this test. FC is a technique that measures a mixture of IgM and IgG. The antigens used are related to several microorganisms and tissues, which causes unspecific reactions and yields false-positives. Because there usually is a high IgG level in the population, caused by previous infections, this technique requires serum-matched samples to prove seroconversion.
Serological Diagnosis
IgM detection is the most common test ordered in general pediatrics to diagnose pneumonia caused by MP. Although its sensitivity depends on the humoral immune response and the time at which the test was taken, generally IgM appears somewhere between 7 to 10 days after the onset of the clinical condition, and it rapidly increases, which makes it a fundamental pillar in the diagnosis of the infection caused by this microorganism, with a sensitivity of 80% or more. Nevertheless, in some patients, especially those under 2 years old, the IgM does not develop until 2 weeks after the beginning of the disease, which limits the sensitivity of this diagnostic procedure. IFI to determine IgM considers as a positive a number of 1/32 titers, and it is a classic technique for the diagnosis, but its reading requires trained personnel. Enzyme immune assays (EIA) are techniques that are easy to implement in clinical laboratories and can detect IgM and IgG separately, which eases the differentiation between an active infection and a previous one. It has been proven that IgM in children can have sensitivity levels as high as 89% to 92%. Also, the specificity of IgM detection done through enzyme-linked immunosorbent assay (ELISA) can vary in about 25% to 90%, depending on the commercial kit being used.
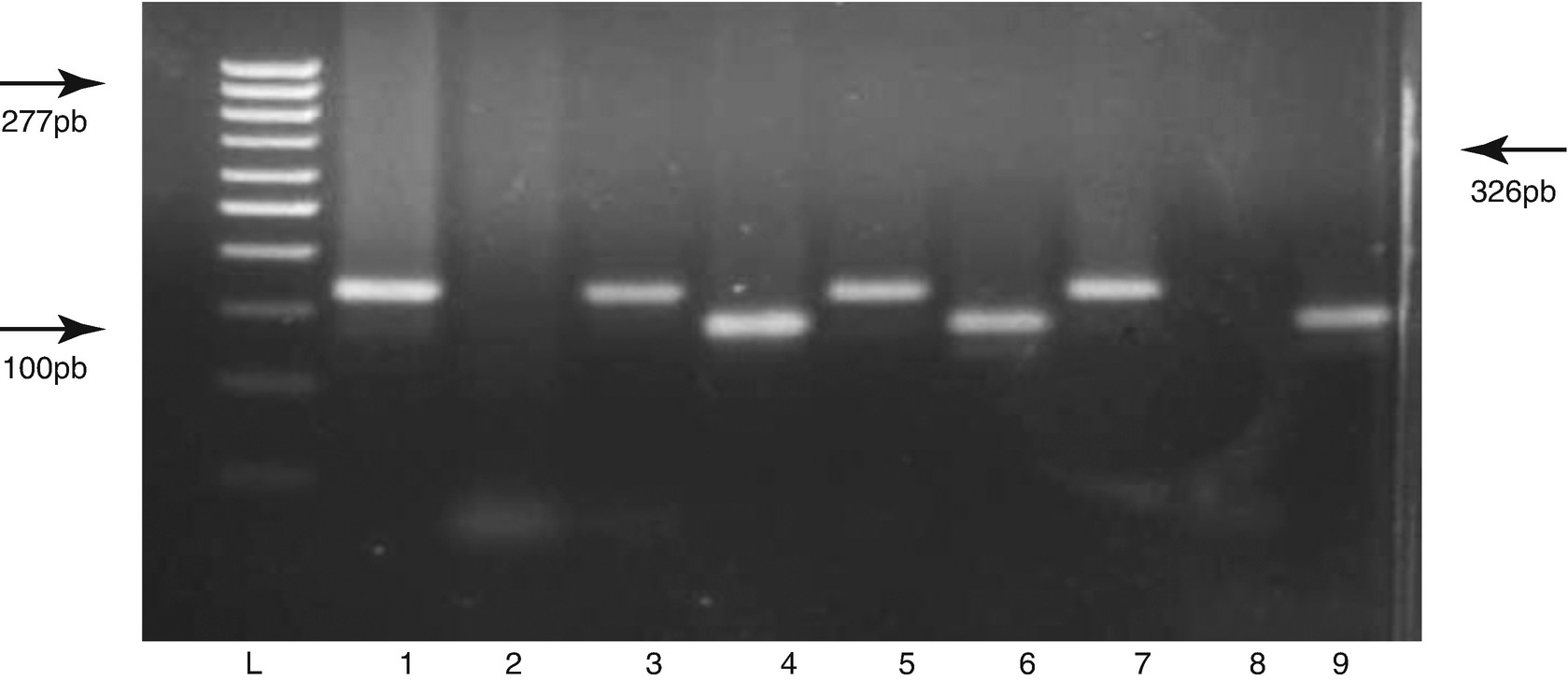
DNA Amplification Polymerase Chain Reaction (PCR)

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


