Although acute myocardial infarction is the most clinically significant cause of ST-segment elevation, other serious clinical conditions have been reported with this electrocardiographic abnormality. We report a patient with pneumomediastinum who presented with dyspnea and electrocardiographic changes mimicking ST-segment elevation myocardial infarction. Coronary angiography demonstrated no evidence of myocardial injury and the electrocardiographic abnormality promptly resolved with the resolution of the pneumomediastinum.
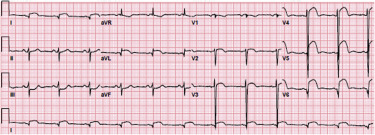
A 46-year-old man presented to the emergency department with chest pain that started approximately 30 minutes before arrival. He was helping his friend move furniture when he started experiencing sharp retrosternal chest pain that radiated to his left arm and was associated with nausea, vomiting, and dyspnea. On arrival at the emergency department, the patient was still complaining of chest pain. On examination, he was pale and in distress. His oral temperature of 98.4°F, a heart rate of 75 beats/min, blood pressure 140/90 mm Hg in all 4 extremities, respiratory rate 18 breaths per minute, and oxygen saturation of 94%. Chest examination did not reveal any abnormalities. The heart sounds were normal, and there were no murmurs, gallops, or rubs. Repeat 12-lead electrocardiogram (ECG) demonstrated sinus rhythm with evidence of ST-segment elevation in the anterolateral leads (V 2 to V 6 , I, and aVL) with reciprocal changes in the inferior leads ( Figure 1 ). Coronary angiography did not demonstrate any significant narrowings ( Figure 2 , Supplementary Video 1 ). Chest radiograph then showed subcutaneous emphysema in the neck ( Figure 3 ). Emergent chest computed tomography with contrast demonstrated extensive pneumomediastinum extending into the lower neck, air-fluid level collection within the mediastinum, and subcutaneous emphysema ( Figure 4 ), all related to lower esophageal perforation based on the large amount of extraluminal oral contrast. He was taken emergently to the operative room for chest tube and esophageal stent placement. An ECG obtained after surgery showed resolution of the ST-segment elevation without the development of T-wave inversion or abnormal Q waves ( Figure 5 ). Antibiotic therapy was administered to prevent mediastinitis. During the following days, his condition improved with progressive decrease of the subcutaneous emphysema and pneumomediastinum making it possible for him to be discharged to an acute rehabilitation facility. At 1- and 3-month follow-up, no relapse or complications were observed.