9 Pneumoconioses
Overview and General Considerations
The toxicity and corresponding fibrogenicity of inorganic particulates are related to both the nature of the dust and the nature of the host response.1 One important feature of particle toxicity is the aerodynamic diameter, with particles in the size range of 1 to 5 μm having the highest probability of deposition and retention within the respiratory tract. In addition, the total inhaled dose and intrinsic properties of the dust are important determinants of fibrosis. For example, crystalline silica is highly fibrogenic, whereas carbon is an innocuous “nuisance” dust. Host factors include efficiency of clearance mechanisms and individual susceptibility. Many of the dusts have a characteristic reaction pattern or appearance in histologic sections, which permits an accurate diagnosis. The silicotic nodule and the asbestos body are familiar examples. Others are associated with a reaction pattern that may suggest the diagnosis, but a careful occupational history or use of supplemental analytic techniques may be required to confirm the diagnosis, such as with berylliosis, in which the histologic findings closely resemble those in sarcoidosis.
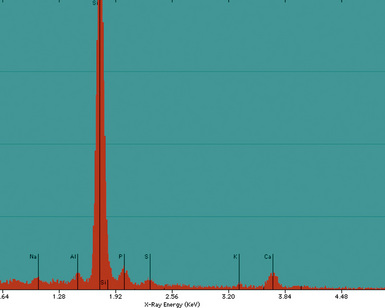
Analytic electron microscopy provides a powerful tool for identification of dusts in lung tissue samples, and these methods are emphasized when appropriate.2 An analytic electron microscope consists of a scanning or transmission electron microscope equipped with an energy-dispersive spectrometer. Electron microscopic techniques may permit the detection of particles too small to be observed by light microscopy. Furthermore, energy-dispersive x-ray analysis (EDXA) identifies the elemental composition of individual particulates, which can be critical to the identification and, in some cases, the source of the inhaled dust. It must be emphasized, however, that the identification of a particular xenobiotic in lung tissue is in and of itself not proof of disease and must be correlated with the pathologic response (if any) to the dust in routine histologic sections.
Types of Pneumoconiosis
Silicosis
Silicosis results from the inhalation of particles of crystalline silica. It is characterized by circumscribed areas of nodular fibrosis that tend to have the greatest profusion in the upper lung zones. Occupations with exposure to crystalline silica are summarized in Box 9-1.3 In the past, very heavy exposures occurred from sandblasting. This type of exposure has been banned in most places. Soil in the extreme eastern and western portions of the United States is rich in alpha quartz (the most common form of crystalline silica). Silicotic nodules may be found in the thoracic lymph nodes and even within the lung parenchyma in farmers and agricultural laborers working in these regions.
Pathologic Findings
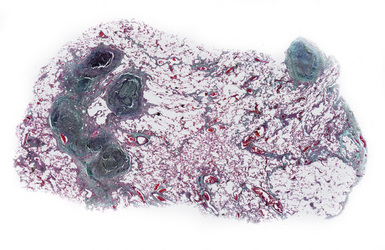
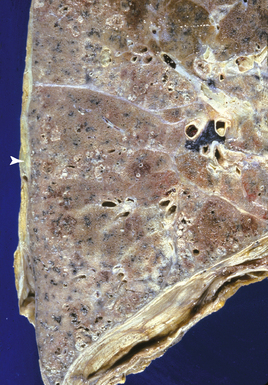
Silicotic nodules are of firm consistency and typically slate gray in appearance, measuring from a few millimeters to approximately 1 cm in diameter (Figs. 9-1 and 9-2). As the disease progresses in severity, the nodules may become confluent (Figs. 9-3 and 9-4). Areas of confluent fibrosis greater than 2 cm in maximum dimension are the defining feature of conglomerate silicosis. Cavitation may occur within areas of confluent fibrosis and, when present, suggests the possibility of superimposed tuberculosis.
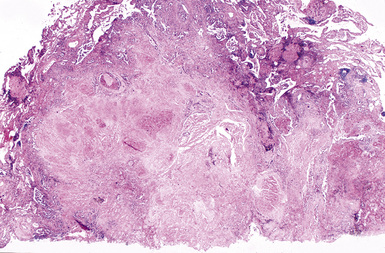
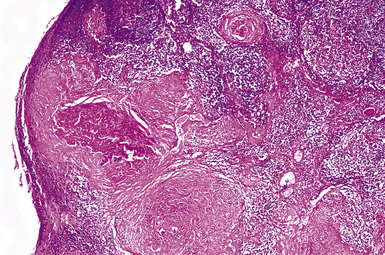
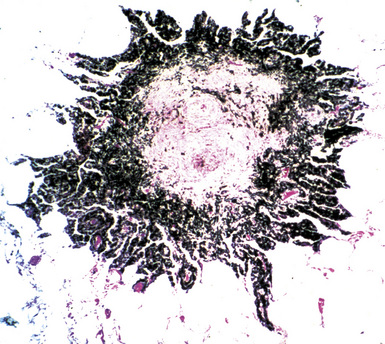
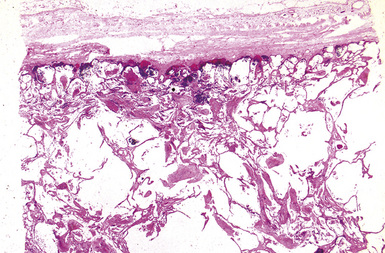
The histologic hallmark of silicosis is the silicotic nodule.4,5 This lesion is a sharply circumscribed nodule consisting of dense, whorled hyalinized collagen (Fig. 9-5). More loosely arranged collagen bundles are typically found at the periphery of the nodule. In recently formed lesions, macrophages form a mantle around the fibrotic center. Longstanding lesions may be calcified or even ossified (Fig. 9-6). The nodules may be present anywhere within the lung parenchyma but typically are most numerous in the upper lung zones. Not uncommonly, they are concentrated beneath the pleura (Fig. 9-7). There may also be extensive pleural fibrosis6 (Fig. 9-8). Nodules are frequently also present within hilar lymph nodes (Fig. 9-9). In patients with extremely high exposures to very fine silica particles, the pattern of resultant lung injury may closely resemble that in pulmonary alveolar proteinosis, characterized by the presence of granular eosinophilic material filling the alveoli, alveolar ducts, and bronchioles (Fig. 9-10). Cholesterol clefts may be prominent within the intra-alveolar material. The granular proteinaceous exudate typically stains strongly positive with periodic acid/Schiff with diastase (D-PAS).
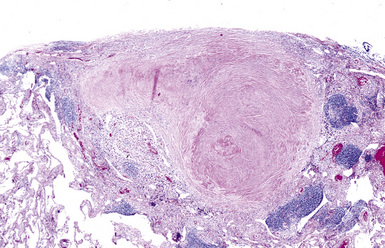
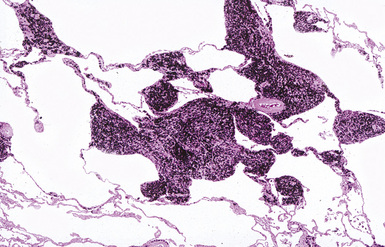
Figure 9-7 Silicosis. The lung parenchyma underlying the pleura is a common location for silicotic nodules.
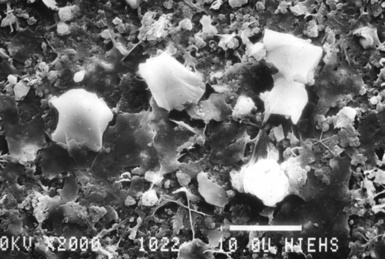
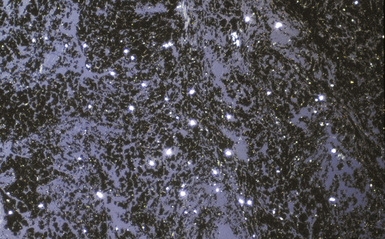
Examination with polarizing microscopy shows faintly birefringent particulates within the fibrotic nodules (Fig. 9-11). Larger, brightly birefringent particles, which represent silicates, may also be seen, but these should not predominate (see later section on silicatosis).7 On scanning electron microscopy the particles appear angulated (Fig. 9-12). Analytic electron microscopy with EDXA reveals peaks for silicon only (Fig. 9-13).
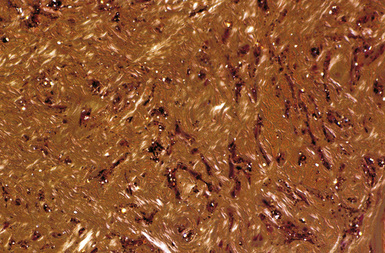
Figure 9-11 Silicosis. Partial polarization of a silicotic nodule demonstrates faintly birefringent silica particles.
Differential Diagnosis
Silicotic nodules must be distinguished from the fibrotic nodules of healed or “burned-out” sarcoidosis, as well as healed mycobacterial or fungal infections, a classic example being the so-called histoplasmoma. The presence of multinucleate giant cells and the absence of significant dust deposits favor sarcoidosis. Sarcoid granulomas may contain fine needle-like or large, platy birefringent particles, which represent endogenous calcium carbonate or oxalate, respectively (Fig. 9-14). These particles should not be confused with the foreign material of pneumoconiosis. The presence of necrosis in association with giant cells favors an infectious etiology. Patients with silicosis are at increased risk for acquiring tuberculosis.8 Both processes may be present simultaneously. Concurrent tuberculosis infection is most likely to occur with conglomerate silicosis.
Extrathoracic location does not rule out a silicotic origin of a fibrous nodule, because silicotic nodules have been found in the liver, spleen, bone marrow, and abdominal lymph nodes.9 Extrathoracic involvement, when present, usually occurs in the setting of advanced pulmonary silicosis. The diagnostic yield of transbronchial biopsy in silicosis is low, probably because the firm circumscribed nodules are pushed aside by the biopsy forceps.
Coal Worker’s Pneumoconiosis
Clinical Presentation
Patients exhibit a range of clinical presentations, from asymptomatic with simple CWP to markedly dyspneic with PMF. The latter is associated with hypoxemia and cor pulmonale and may be fatal.10,11
Pathologic Findings
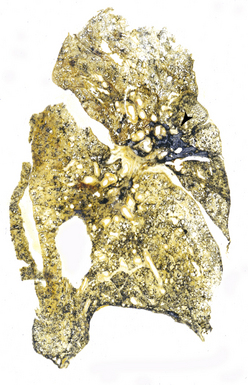
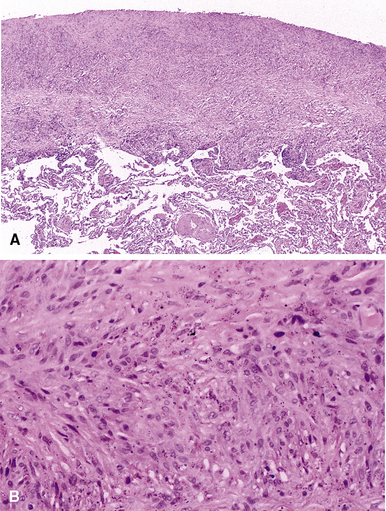
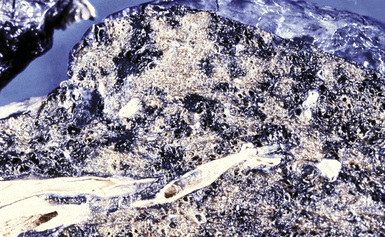
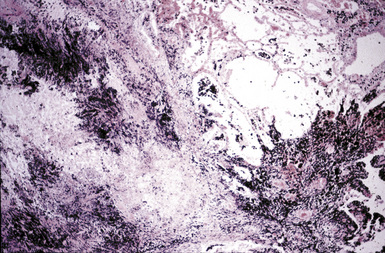
CWP is characterized by increased pigmentation in the lungs resulting from the deposition of coal dust (Figs. 9-15 to 9-17). Foci of accentuated pigmentation, superimposed on a background of diffusely increased pigment, are present on the pleura and within the lung parenchyma. In some cases, palpable nodules are present within the lung parenchyma and usually are most numerous in the upper lung zones. These nodules are grossly similar to silicotic nodules, except for being black rather than slate gray (Fig. 9-18). The most advanced cases of CWP feature greater than 2 cm in maximal dimension confluent areas of irregular fibrosis with the consistency of vulcanized rubber, typically in the upper to mid-lung zones (Fig. 9-19). These are the lesions of PMF. Cavitation may occur in areas of PMF and, when present, suggests superimposed tuberculosis.12
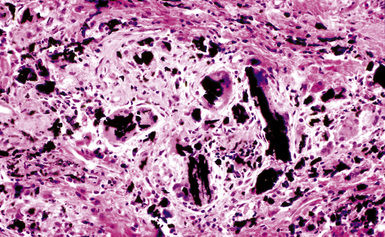
The histologic hallmark of CWP is the coal dust macule (Fig. 9-20). Coal dust macules consist of discrete collections of interstitial pigment deposition in the vicinity of respiratory bronchioles. Areas of emphysematous destruction, referred to as focal emphysema, are typically present at the periphery of macules. Pigment-laden macrophages may be present within alveolar spaces, and pigment deposits may occur anywhere along the lymphatic routes of the lung, including the secondary lobular septa, as well as in the pleura. Lymph nodes frequently contain numerous pigmented macrophages and may also demonstrate silicotic nodules. Silicotic nodules may also be present within the lung parenchyma, but unlike cases of pure silicosis, a collarette of pigmented macrophages often surrounds the nodules, imparting a “Medusa head” appearance (Fig. 9-21). Areas of massive fibrosis (Fig. 9-22) consist of collagen bundles that are arranged in a haphazard distribution and intermixed with abundant pigment (Figs. 9-23 and 9-24). Vascular obliteration is common within areas of PMF, and ischemia may be the cause of cavitation in some cases.
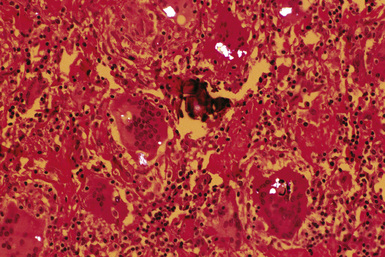
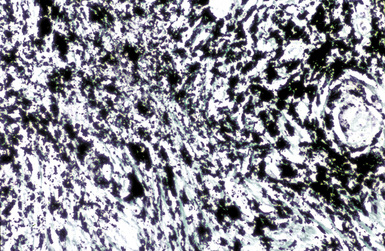
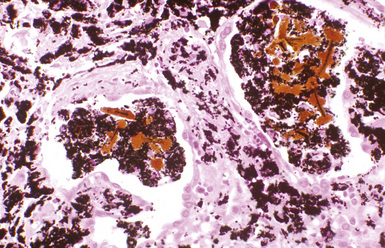
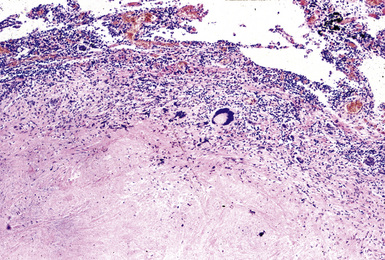
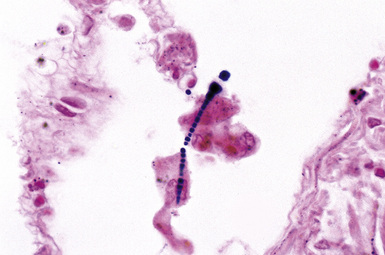
Examination with polarizing microscopy typically shows numerous faintly to brightly birefringent particulates within a background of black pigment (Fig. 9-25). This appearance reflects the mixed nature of coal dust, which is composed of amorphous carbon, silicates, and silica. The presence of silica in coal dust is responsible for the formation of silicotic nodules and is an important factor in the pathogenesis of PMF.13 Ferruginous bodies are sometimes seen in the lungs of coal workers, typically within the alveolar spaces (Fig. 9-26). These may be distinguished from true asbestos bodies by virtue of their black carbonaceous cores14 (Fig. 9-27). Tuberculosis may also complicate CWP (Fig. 9-28).
Differential Diagnosis
CWP must be distinguished from the anthracotic pigment deposition that occurs in urban dwellers and cigarette smokers, and from graphite worker’s pneumoconiosis. The extent of pigmentation in normal persons is a function of environmental exposure to carbon-containing dust and the natural ability of the lung to rid itself of particulates. Distinction from CWP is somewhat a matter of degree, but the presence of true coal dust macules, as described earlier, is indicative of CWP. The finding of anthracotic pigment-laden macrophages within alveoli is also a useful feature, but such macrophages may be absent in miners who have been retired for many years. Graphite worker’s pneumoconiosis appears similar to CWP, but graphite is crystalline, whereas the carbon present in coal is amorphous (Fig. 9-29). A giant cell reaction to the crystalline carbon of graphite assists in this distinction.3 Transbronchial biopsy may be useful in the diagnosis of CWP, showing the typical changes described earlier. However, areas of nodular fibrosis or PMF may be missed by such sampling. Therefore, transbronchial biopsy is not useful for assessing disease severity.
Asbestosis
Asbestosis is defined as pulmonary interstitial fibrosis caused by the inhalation of asbestos fibers.15,16 Substantial and significant exposures to asbestos can occur in a variety of occupational settings, including the mining and milling of asbestos, the manufacture of asbestos-containing products, and the use of products containing asbestos. Occupations that involve the use of asbestos-containing products include insulators, shipyard workers, railroad workers, power plant workers, U.S. Navy or Merchant Marine seamen, oil or chemical refinery workers, construction workers, steel and other molten metal workers, and paper mill workers (Box 9-2). A few cases of asbestosis have also occurred among household contacts of asbestos workers, apparently as a consequence of exposure to asbestos brought home on the workers’ clothing.
Pathologic Findings
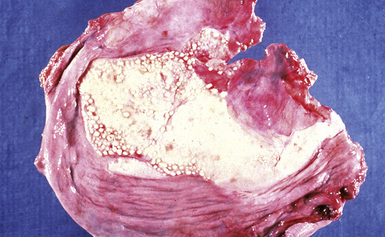
The fibrosis in asbestosis demonstrates a fine, reticular pattern, and the macroscopic appearance of the lungs ranges from normal to severely scarred and shrunken (Fig. 9-30) with evidence of honeycombing.17,18 Diffuse visceral pleural fibrosis is frequently present and is usually most severe over the lower lung zones. Parietal pleural plaques, which are frequently bilateral (Fig. 9-31), are present in the vast majority of cases and may be calcified. Although diffuse pleural fibrosis and plaques serve as a suggestive indicator of an asbestos etiology of pulmonary fibrosis, the term “asbestosis” should not be applied to these pleural abnormalities when they occur in the absence of parenchymal disease.
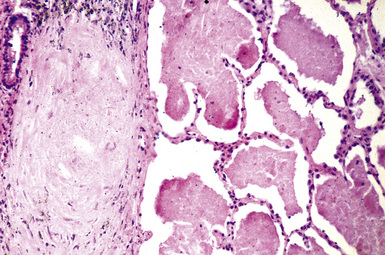
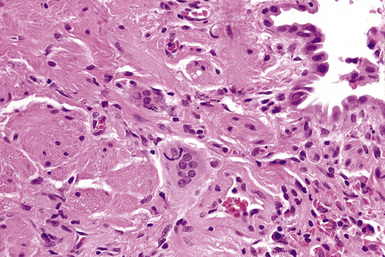
Histologically, asbestosis is characterized by discrete foci of fibrosis in the walls of respiratory bronchioles accompanied by asbestos bodies17 (Box 9-3 and Fig. 9-32). As the fibrotic process progresses, it extends distally to the alveolar ducts and proximally to the membranous (terminal) bronchioles. The fibrosis also extends radially to involve alveolar septa distant from the respiratory bronchiole (Fig. 9-33). In the most advanced cases, honeycomb fibrosis is present (Fig. 9-34), characterized by 0.5- to 1-cm–diameter fibrotic-walled cysts that are lined by bronchiolar epithelium and often contain pools of mucus. Alveolar macrophages are sometimes so prominent as to suggest a diagnosis of desquamative interstitial pneumonia (DIP). In some cases, multinucleate giant cells may be identified, within either the interstitium or the alveolar spaces (Fig. 9-35). Rarely, hyperplastic alveolar type II pneumocytes may contain cytoplasmic hyaline (Fig. 9-36) reminiscent of that found in the cytoplasm of hepatocytes in alcoholic liver disease.
Box 9-3 Histologic Grading of Severity of Fibrosis in Asbestosis*
From Roggli VL, Gibbs AR, Attanoos R, et al. Pathology of asbestosis—an update of the diagnostic criteria. Report of the Asbestosis Committee of the College of American Pathologists and Pulmonary Pathology Society. Arch Pathol Lab Med. 2010;134:462–480.
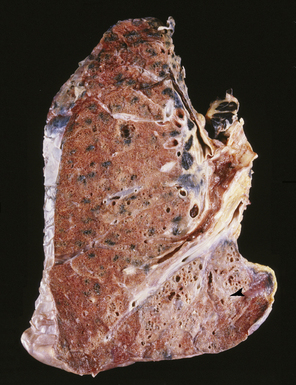
Figure 9-34 Asbestosis. In a more advanced case, honeycombing (arrowhead) is seen, in addition to lower lobe fibrosis.
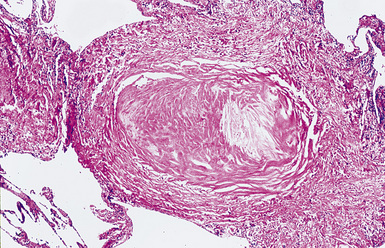
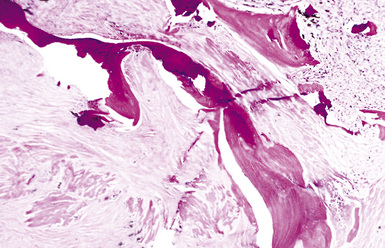
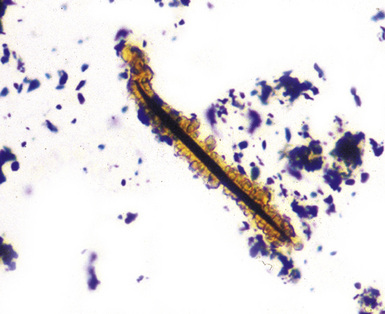
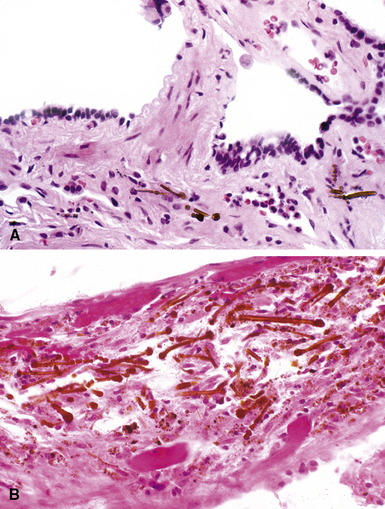
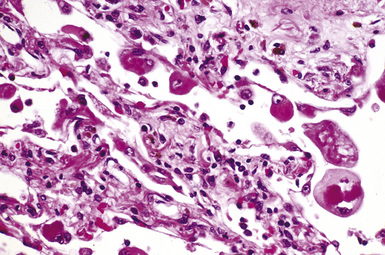
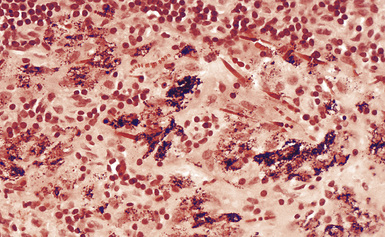
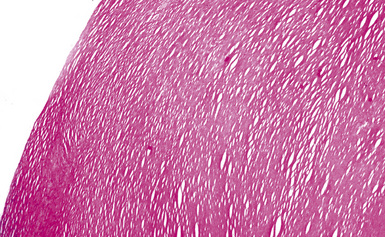
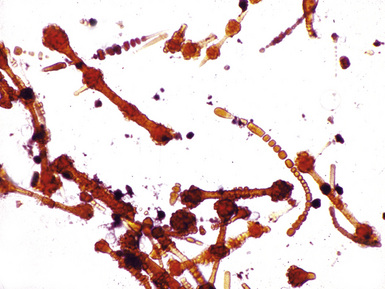
The hallmark of asbestos exposure is the asbestos body, a rod-like, beaded, or dumbbell-shaped structure with golden brown coating and a thin, translucent core.19 Asbestos bodies are typically found in the peribronchiolar interstitium (Fig. 9-37), but, with heavy exposure, may be seen in the alveolar spaces (Fig. 9-38). Detection of asbestos bodies may be facilitated by the use of iron stains, which impart a deep blue color (Fig. 9-39). Asbestos bodies may also be seen in sputum (Fig. 9-40) and in thoracic lymph nodes (Fig. 9-41) of patients with heavy exposure to asbestos. Pleural plaques consist of layers of acellular hyalinized collagen, arranged in a “basketweave” pattern (Fig. 9-42). Visceral pleural fibrosis may show this basketweave pattern or appear as compact layers of collagen. A mild lymphocytic infiltrate sometimes accompanies the fibrosis.
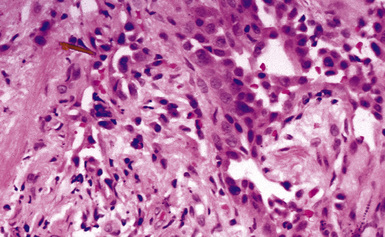
Figure 9-37 Asbestosis. In a transbronchial biopsy, interstitial fibrosis and an asbestos body (upper left) can be seen.
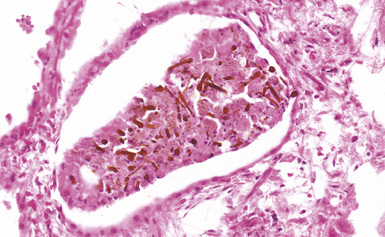
Figure 9-38 Asbestosis. Asbestos bodies are present within an alveolar space in this case of severe asbestosis.
Digestion procedures have been developed for quantifying the content of asbestos in lung tissue (Fig. 9-43). Any of the commercial forms of asbestos (chrysotile and amphiboles) may be identified in lung tissue from patients with asbestosis by means of analytic electron microscopy20 (Figs. 9-44 and 9-45). In cases in which asbestos bodies are not identified in histologic sections, the fiber burden is typically always more than 2 standard deviations below the mean value in cases with bona fide (histologically confirmed) asbestosis.21 Polarizing microscopy is not useful for the detection of asbestos in histologic sections.