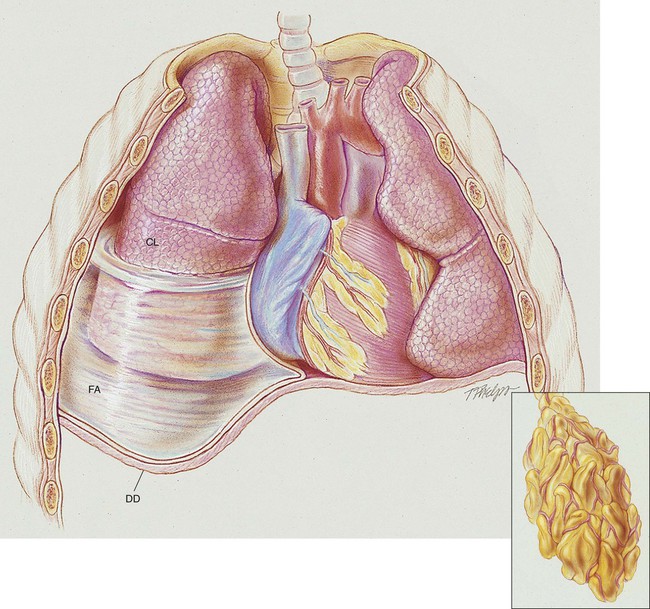
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with pleural diseases. • Describe the causes of pleural diseases. • List the cardiopulmonary clinical manifestations associated with pleural diseases. • Describe the general management of pleural diseases. • Describe the clinical strategies and rationales of the SOAPs presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. A number of pleural diseases can cause fluid to accumulate in the pleural space; this fluid is called a pleural effusion, or if infected, an empyema (see Figure 23-1). Similar to free air in the pleural space, fluid accumulation separates the visceral and parietal pleura and compresses the lungs. In severe cases, atelectasis will develop, the great veins may be compressed, and cardiac venous return may be diminished. Pleural effusion and empyema produce a restrictive lung disorder. • Pleural fluid protein >2.9 g/dL (29 g/L) • Pleural fluid cholesterol >45 mg/dL (1.16 mmol/L) • Pleural fluid lactate dehydrogenase (LDH) >60% of upper limit for serum Pleural effusion may develop from extension of a caseous tubercle into the pleural cavity. It also is possible that the inflammatory reaction that develops in tuberculosis obstructs the lymphatic pores in the parietal pleura. This in turn leads to an accumulation of protein and fluid in the pleural space. Pleural effusion caused by tuberculosis is generally unilateral and small to moderate in size (see Chapter 17).
Pleural Effusion and Empyema
Anatomic Alterations of the Lungs
Etiology and Epidemiology
Common Causes of Exudative Pleural Effusion
Malignant Pleural Effusions
Tuberculosis