Pleural Diseases
GENERAL PRINCIPLES
• The pleural lining is a serous membrane covering the lung parenchyma, chest wall, diaphragm, and mediastinum.
• The pleural membrane covering the surface of the lung is known as the visceral pleura, the parietal pleura covers the remaining structures.
• In between the visceral and parietal pleurae of each lung is the pleural space, a potential space that contains a thin layer of fluid of ∼10 mL in volume.
• The parietal pleura secretes ∼2.5 L of fluid daily, which is reabsorbed by the visceral pleura.
Definition
• A pleural effusion is >10 mL accumulation of fluid in the pleural space.
 A hemothorax refers to a pleural effusion that is comprised mainly of blood.
A hemothorax refers to a pleural effusion that is comprised mainly of blood.
 Chylothorax is a collection of chyle within the pleural space.
Chylothorax is a collection of chyle within the pleural space.
 A parapneumonic effusion is any effusion caused by bacterial pneumonia and occurs in about 40% of cases of bacterial pneumonia.1
A parapneumonic effusion is any effusion caused by bacterial pneumonia and occurs in about 40% of cases of bacterial pneumonia.1
 Uncomplicated parapneumonic effusions do not require chest tube drainage for complete resolution and are presumed to be sterile.
Uncomplicated parapneumonic effusions do not require chest tube drainage for complete resolution and are presumed to be sterile.
 Complicated parapneumonic effusions are accompanied by bacterial invasion of the pleural space and typically do require thoracostomy drainage, although occasionally may improve with antibiotic therapy alone.
Complicated parapneumonic effusions are accompanied by bacterial invasion of the pleural space and typically do require thoracostomy drainage, although occasionally may improve with antibiotic therapy alone.
 Empyema simply refers to a complicated parapneumonic effusion with grossly purulent pleural fluid and is presumed to be infected even though cultures may not always be positive. On occasion, empyema may not be associated with a pneumonic process.
Empyema simply refers to a complicated parapneumonic effusion with grossly purulent pleural fluid and is presumed to be infected even though cultures may not always be positive. On occasion, empyema may not be associated with a pneumonic process.
 Other more complicated classifications of parapneumonic effusions have also been developed.2,3
Other more complicated classifications of parapneumonic effusions have also been developed.2,3
• A pneumothorax is a collection of gas in the pleural space.4,5
 Primary spontaneous pneumothorax occurs when there is no obvious underlying lung disease.
Primary spontaneous pneumothorax occurs when there is no obvious underlying lung disease.
 Secondary spontaneous pneumothorax is a complication of underlying lung disease.
Secondary spontaneous pneumothorax is a complication of underlying lung disease.
Epidemiology
• More than 1 million cases of pleural effusion occur annually in the United States.
• Incidence of pneumothorax varies widely by gender, country, and race.4
Etiology
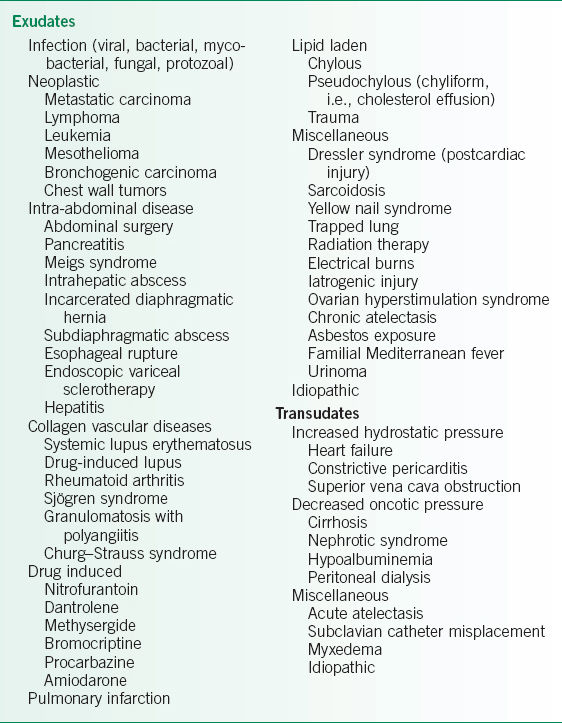
• Pleural effusions have a variety of causes (Table 23-1).
 Empyema is generally caused by extension of an infection of the lung or surrounding tissue.
Empyema is generally caused by extension of an infection of the lung or surrounding tissue.
 Common microbial pathogens are Staphylococcus aureus, Streptococcus species, and Haemophilus influenza.
Common microbial pathogens are Staphylococcus aureus, Streptococcus species, and Haemophilus influenza.
 Empyemas are frequently polymicrobial in cases where aspiration is suspected.
Empyemas are frequently polymicrobial in cases where aspiration is suspected.
 The three major grouped causes of chylothorax are malignancy (50% of cases), trauma (25%), and idiopathic (15%). Other causes account for 10%.6
The three major grouped causes of chylothorax are malignancy (50% of cases), trauma (25%), and idiopathic (15%). Other causes account for 10%.6
 Seventy-five percent of chylous effusions related to malignancy are due to lymphomas related to obstruction of pleural lymphatics.
Seventy-five percent of chylous effusions related to malignancy are due to lymphomas related to obstruction of pleural lymphatics.
 Trauma as a causative factor of chylothorax includes any cardiothoracic surgical procedure. It may take place 1–2 weeks postsurgery for the chylothorax to become apparent.
Trauma as a causative factor of chylothorax includes any cardiothoracic surgical procedure. It may take place 1–2 weeks postsurgery for the chylothorax to become apparent.
 In a number of cases, chylothorax results from transdiaphragmatic leakage of chylous ascites. Causes of chylous ascites include nephrotic syndrome, hypothyroidism, and cirrhosis.
In a number of cases, chylothorax results from transdiaphragmatic leakage of chylous ascites. Causes of chylous ascites include nephrotic syndrome, hypothyroidism, and cirrhosis.
 Hemothorax may result from trauma or iatrogenesis, and rarely can occur spontaneously.7
Hemothorax may result from trauma or iatrogenesis, and rarely can occur spontaneously.7
 When the etiology for the effusion cannot be determined despite appropriate evaluation, a benign course is typical.8
When the etiology for the effusion cannot be determined despite appropriate evaluation, a benign course is typical.8
• Secondary pneumothorax is often seen in chronic obstructive pulmonary disease (COPD), AIDS, cystic fibrosis, TB, sarcoidosis, pulmonary fibrosis, asthma, Marfan disease, lymphangioleiomyomatosis, pulmonary Langerhans cell histiocytosis, trauma, or any disease with pulmonary cavity formation.4 Catamenial pneumothorax is a rare condition of spontaneous pneumothorax occurring in close proximity to menstruation and is often recurrent.4,5 It may also cause hemopneumothorax.
TABLE 23-1 CAUSES OF PLEURAL EFFUSION
Pathophysiology
• Pleural effusions can be categorized as transudates or exudates (Table 23-2).9,10
 Transudates result primarily from passive fluid shifts that occur as a result of changes in the hydrostatic and oncotic pressures of the circulation.
Transudates result primarily from passive fluid shifts that occur as a result of changes in the hydrostatic and oncotic pressures of the circulation.
 Exudates imply an active pleural process such as inflammation of the pleura or underlying lung tissue.
Exudates imply an active pleural process such as inflammation of the pleura or underlying lung tissue.
 There are numerous causes of both transudates and exudates (Table 23-1).
There are numerous causes of both transudates and exudates (Table 23-1).
• Primary spontaneous pneumothorax is thought to result from rupture of subpleural apical blebs.4,5
• Secondary pneumothorax results from rupture of already pathologic lung architecture.4
Risk Factors
• Risk factors for pleural effusion reflect those of the underlying causative disease.
• Primary spontaneous pneumothoraces are more common in tall, thin males, and recur 50% of the time.4
• Smoking also increases the risk of spontaneous pneumothorax.4,5
DIAGNOSIS
Clinical Presentation
• Symptom onset may be chronic, subacute, or acute depending on the rapidity which the pleural pathology developed.
• If the effusion or pneumothorax is very large in nature, it may cause mass effect and even cardiac tamponade, resulting in a life-threatening condition.
• In cases of massive hemothorax requiring surgical intervention, clamping the chest tube may result in tension hemothorax and cardiovascular collapse.
• Chylothorax is nonirritating and bacteriostatic, thus secondary infection is extremely rare.6
History
• Dyspnea is the primary symptom of pleural disease, and pain may also be present.
 Pain is generally pleuritic in nature.
Pain is generally pleuritic in nature.
 Referred pain to the abdomen and ipsilateral shoulder is possible.
Referred pain to the abdomen and ipsilateral shoulder is possible.
• Other symptoms depend on the specific etiology of the pleural disease.
 Empyema may be associated with fevers, chills, and malaise.
Empyema may be associated with fevers, chills, and malaise.
 Hemothorax may present with signs and symptoms of anemia.
Hemothorax may present with signs and symptoms of anemia.
 Chylothorax contains large amounts of fat, protein, and lymphocytes, which accounts for nutritional and immunologic deficiencies observed when they are chronic in nature.
Chylothorax contains large amounts of fat, protein, and lymphocytes, which accounts for nutritional and immunologic deficiencies observed when they are chronic in nature.
Physical Examination
• Decreased expansion on inspiration, dullness to percussion, decreased or absent breath sounds on auscultation, and absent or reduced tactile fremitus are all consistent with a pleural effusion.11,12
• Asymmetric chest wall, decreased breath sounds, decreased tactile fremitus, and hyperresonance to percussion are all consistent with a large pneumothorax.4
Differential Diagnosis
The differential diagnosis for pleural effusion or pneumothorax includes other causes of dyspnea including pulmonary edema, pneumonia, atelectasis, thromboembolic disease, or interstitial lung disease (Table 23-1).
Diagnostic Testing
Laboratories
• Categorization of pleural fluid as transudative or exudative assists with diagnosis and therapeutic management.
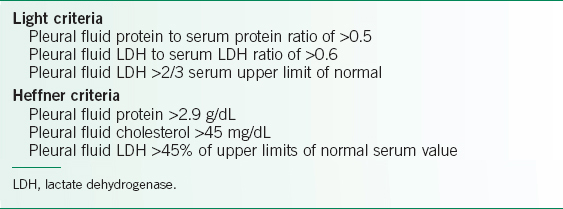
 Light criteria compare levels of protein and lactate dehydrogenase in the effusion with those in the patient’s serum to determine whether inflammation or fluid shift is responsible for the effusion. If one of the three criteria is met, the effusion is defined as an exudate (Table 23-2).9
Light criteria compare levels of protein and lactate dehydrogenase in the effusion with those in the patient’s serum to determine whether inflammation or fluid shift is responsible for the effusion. If one of the three criteria is met, the effusion is defined as an exudate (Table 23-2).9
 Heffner criteria has similar sensitivity for identifying exudative pleural effusions when compared to Light criteria and do not require concomitant serum values for comparison (Table 23-2).10
Heffner criteria has similar sensitivity for identifying exudative pleural effusions when compared to Light criteria and do not require concomitant serum values for comparison (Table 23-2).10
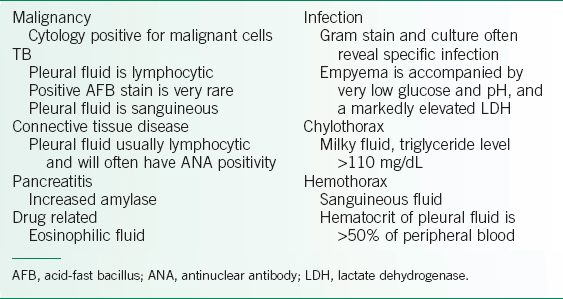
• Other useful studies to differentiate the type of pleural effusion include pH, glucose, cell count, Gram stain, culture, and triglycerides. Hematocrit should be sent if hemothorax is suspected.
 Empyema can be diagnosed by a positive Gram stain or culture. Empyema is also characterized by a low pH and glucose.1
Empyema can be diagnosed by a positive Gram stain or culture. Empyema is also characterized by a low pH and glucose.1
 Hemothorax is defined by a pleural hematocrit/serum hematocrit of >0.5.7
Hemothorax is defined by a pleural hematocrit/serum hematocrit of >0.5.7
 Chylothorax is diagnosed by pleural triglycerides >110 mg/dL or by the presence of chylomicrons. If chylothorax is suspected, and triglycerides are 50–100 mg/dL, a lipoprotein electrophoresis can confirm the presence of chylomicrons.6
Chylothorax is diagnosed by pleural triglycerides >110 mg/dL or by the presence of chylomicrons. If chylothorax is suspected, and triglycerides are 50–100 mg/dL, a lipoprotein electrophoresis can confirm the presence of chylomicrons.6
 Malignant pleural effusion is diagnosed by a positive fluid cytology and though highly specific it is not sensitive.
Malignant pleural effusion is diagnosed by a positive fluid cytology and though highly specific it is not sensitive.
 See Table 23-3 for other pleural fluid laboratory values associated with specific pleural effusions.
See Table 23-3 for other pleural fluid laboratory values associated with specific pleural effusions.
Imaging
• The plain CXR is generally the first imaging study obtained when a patient presents with a suspected pleural effusion or pneumothorax.
 On a posteroanterior chest film, blunting of the costophrenic angle or blurring of the diaphragmatic margin suggests the presence of a pleural effusion. Generally 200–500 mL of fluid is needed to generate this finding.13
On a posteroanterior chest film, blunting of the costophrenic angle or blurring of the diaphragmatic margin suggests the presence of a pleural effusion. Generally 200–500 mL of fluid is needed to generate this finding.13
 A lateral decubitus film of the affected side can reveal an effusion of ∼100 mL and allows for assessment of a free-flowing versus loculated effusion.
A lateral decubitus film of the affected side can reveal an effusion of ∼100 mL and allows for assessment of a free-flowing versus loculated effusion.
 Uncomplicated parapneumonic effusions typically layer <10 mm on a decubitus CXR.1,2
Uncomplicated parapneumonic effusions typically layer <10 mm on a decubitus CXR.1,2
• CT is more sensitive than radiography and can detect the presence of even a very small amount of fluid or air in the pleural space as well as the presence of loculations in the pleural fluid.
• Ultrasound is a modality that is increasingly being used to image the pleural space. Ultrasound can detect fluid or air and provides qualitative information regarding pleural fluid.
 Ultrasound findings such as fluid echogenicity and the presence or absence of septations within the pleural space may change management and predict clinical outcome.
Ultrasound findings such as fluid echogenicity and the presence or absence of septations within the pleural space may change management and predict clinical outcome.
 Ultrasound guidance is often used to direct treatments such as drainage of fluid or chest tube insertion.
Ultrasound guidance is often used to direct treatments such as drainage of fluid or chest tube insertion.
TABLE 23-3 HELPFUL FEATURES OF EXUDATIVE EFFUSIONS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree