Airway epithelium
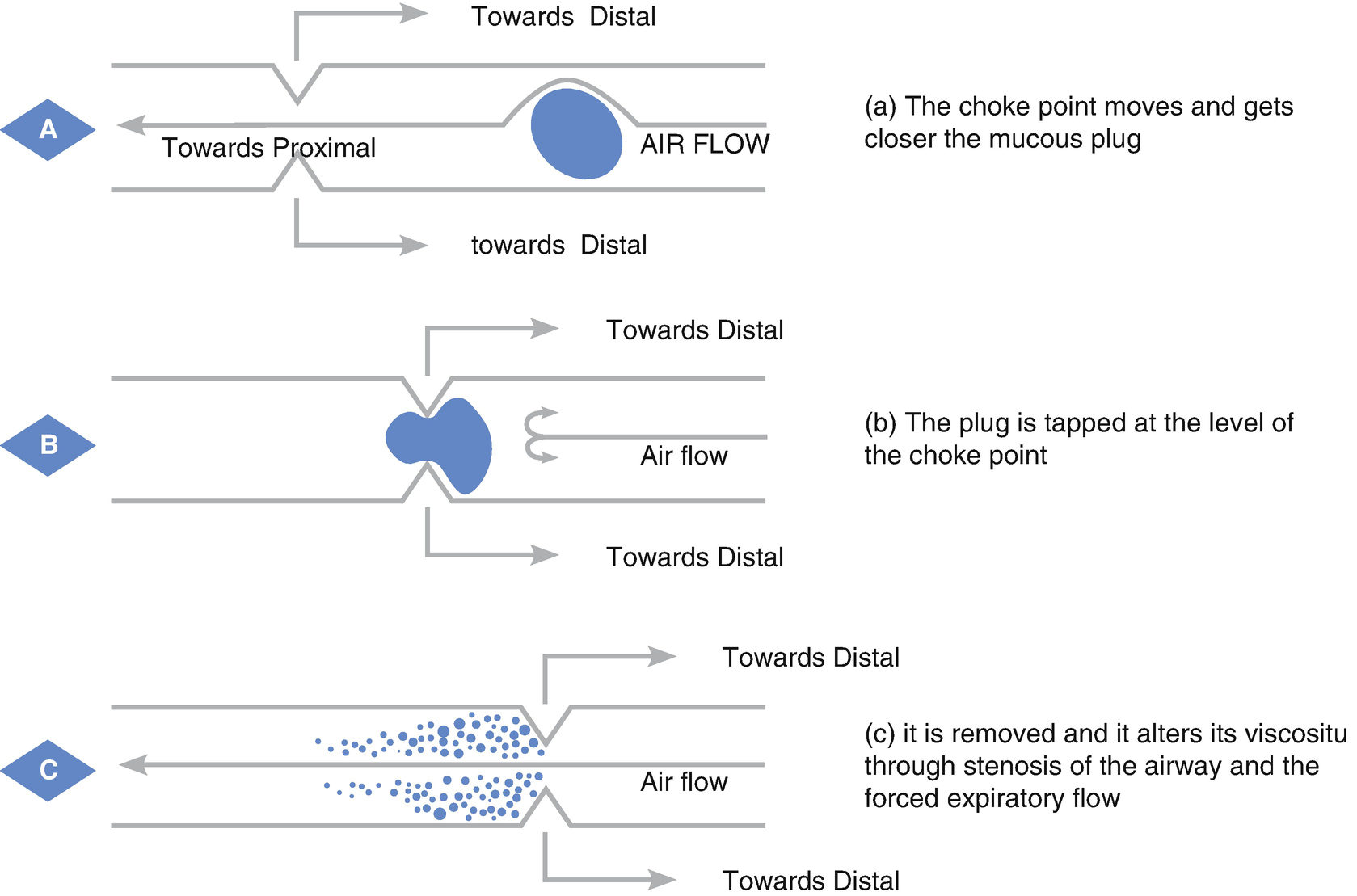
Forced expiration and choke point. (a) The choke point moves and gets closer to the mucous plug. (b) The plug is tapped at the level of the choke point. (c) It is removed and it alters its viscosity through stenosis of the airway and the forced expiratory flow
At more distal levels, the two-phase flow (interaction between the airflow and the mucus layer over the ciliary epithelium) has a central role in the hygiene of the middle airways, and even the more peripheral ones. It has been described that at this level, slow and prolonged expiratory flows that aim to obtain flows with laminar characteristics enhance the natural action of the two-phase flow, producing a significant effect in the mobilization of secretions from the distal airways to the proximal airways.
Considering that airway compromise is not homogeneous, it is very important to focus on the compromised area by auscultation, as well as setting therapeutic objectives in proportion to the findings, to be able to choose the correct technique that results in the most benefit for the patient.
When there are areas with loss of air content (e.g., atelectasis), techniques that contribute to increase the inspired volume should be favored, to recruit collapsed zones. It is necessary to stress that lung recruitment will also favor the permeabilization of the middle airway and even the distal one, because there will be a higher lung volume that will allow an increment of the expired volume, which will favor the depurative action of the two-phase flow.
Therapeutic Intervention
- 1.
Determine the physiopathological disorder
- 2.
Identify the degree of collaboration from the patient
- 3.
Establish the level of compromise
- 1.
Physiopathological disorder: Refers to the identification of a determined ventilation function syndrome (obstructive, restrictive or mixed) present at the moment of the evaluation of the patient. The obstructive physiopathological disorder is characterized by the decrease of the diameter of the central or peripheral airways, with an increment of the airflow resistance and flow decrease, especially expiratory flows, which will result in a significant increase in the work of breathing and the following hypoxemia (partial breathing insufficiency) and even hypercarbia (global breathing insufficiency) in some severe cases, such as in acute severe bronchiolitis.
The restrictive physiopathological disorder encompasses a group of diseases in which the most important physiopathological disorder is a restriction of expansion that limits the pulmonary volumes, with the consequent possibility of losing recruited alveolar units, as in atelectasis.
In any type of functional disorder there is a possibility of loss of effectiveness of coughing, which will result in higher secretion retention and the possibility of creating a feedback loop that will determine the recovery of the functional level of the child.
- 2.
Level of cooperation: It refers to the level of potential cooperation of the patient inasmuch as they can follow the instructions of the physiotherapist when a particular technique is being performed. One classification is the cooperative patient is able to follow instructions of the treating therapist, to cooperate, help and perform active and assisted-active techniques without problems. On the other hand, it is the uncooperative patient who doesn’t have the physical, cognitive or psychomotor abilities to follow the instructions of the physiotherapist to perform a certain technique.
- 3.
Level of compromise: It has to do with the zone of the respiratory system affected by the physiopathological or biomechanical disorder, which may be the thoracic cavity, respiratory musculature, lung parenchyma, or the proximal, mid or distal airway. Each one of these levels has different functions regarding thoracic mobility, ventilation, conduction, and air conditioning.
Techniques of Respiratory Physical Therapy
The techniques of respiratory physical therapy can be classified into two main groups: manual and instrumented.
Manual Physical Therapy Techniques
Thoracic vibration: Oscillatory movement produced by the isometric muscle contraction of the upper limbs which is transmitted by one or both hands of the therapist to the chest of the patient during expiration. The oscillation frequency must not be less than 3 Hz. The goal is to obtain a maximum expiratory flow at least 10% more than the maximum inspiratory flow, which would allow increasing the two-phase flow and loosen and decrease the viscosity of the secretions of the bronchial walls, allowing their mobilization to proximal airways.
Thoracic percussion (clapping): Rhythmic tapping performed with cupped hands on the ventral, dorsal, and lateral zones of the chest in both phases of breathing. It is generally applied while the patient maintains a specific position of postural drainage. It is contraindicated under clinical evidence of bronchospasm. Both vibrations and percussions have the goal of generating an oscillatory effect of the chest wall that will be transmitted to the lungs and airways, aimed at increasing ciliary activity and loosening and mobilizing secretions adhered to the bronchial wall, which would depend of the value of the oscillation frequency transmitted through the thorax. This frequency is close to 15–25 Hz, but it is limited in these manual techniques that only reach 2–8 Hz frequencies.
Postural drainage: Consists in easing secretion transport through the action that gravity has on them. In order to obtain this, it is necessary to place the bronchial segment to drain as vertical as possible; placing the patient in different positions, many of them will be Trendelenburg positions. It is traditionally advised to simultaneously apply percussions and vibrations while the postures are sustained. One of its main limitations is the appearance of adverse effects associated with technique execution (gastroesophageal reflux, desaturation, or elevation of intracranial pressure).
Forced Expiration Technique: The forced expiration technique (FET) consists in making forced expirations with open an open glottis starting with different lung volumes:
Low, mid, and high, interspersed with still breathing at tidal volume. The aim is to mobilize the bronchial secretions to the central airway where they can be swallowed or expectorated. In the specialized literature in English it is also known as the Huffing technique, and it is justified from the physiological concept of point of equal pressure and must be applied cautiously in chronic patients (e.g., cystic fibrosis) where stability of the bronchial walls is so altered that compression during the application of this technique results in the collapse of the airway and the following impact of secretions at a distal level of the collapse. This collapse warrants the avoidance of the forced expiration technique in these patients or its use only later in the bronchial hygiene process, when the secretions have been mobilized to the central airways.
Prolonged slow expiration: Passive technique of expiratory aid applied to the uncooperative patient (from infancy to 8 years), through slow manual thoraco-abdominal pressure that starts at the end of a spontaneous expiration and continues toward a residual volume. Its aim is to obtain a greater expiratory volume than in a normal expiration, to promote the two-phase low and thus contribute to the mobilization of secretions in the periphery of the respiratory tree to the central airway.
Autogenic draining: This technique for the cooperative patient combines slow inspiratory and expiratory flows with forced expirations and coughs in a three-phase sequential cycle:
First phase, loosening of secretions: Slow inspirations/expirations must be performed, with breathing located in the diaphragm, mobilizing small volumes from the functional residual capacity to later gradually increase the inspiratory and expiratory volume, achieving a gradually increased pulmonary capacity, with the aim of unsticking and mobilizing secretions from the periphery to the central airway.
Second phase, collection of secretions: In higher volumes than the normal current volume, but maintaining slow expiratory flows, the secretions are accumulated in the central airways.
Third phase, evacuation: Three to four expirations are performed until the total pulmonary capacity is reached, to conclude with a forced expiration with open glottis or a voluntary cough.
Slow expiration with glottis opened in lateral posture (ELTGOL): It is an active–assisted technique, in which the patient is in the lateral decubitus position with the lung to be treated specifically in the support plane (dependent) and thus making the superolateral lung and the mediastinum help with is maximum exsufflation during expiration. Owing to the position adopted, the pressure of the abdominal viscera will raise the diaphragm of the support lung. In this position, with an open mouth (or kept open by a cylindrical mouth accessory), the physiotherapist presses the abdomen with one hand at the level of the lung and eases the rise of the diaphragm, and applies pressure with the other hand on the superolateral chest wall, producing a pressure against the contralateral shoulder which will ease the reduction of the transversal diameter that favors a complete exsufflation of the inferolateral lung, always controlling that the expiration is slow and prolonged. Applying the maneuver in a slow manner avoids bronchial collapsing and allows a greater displacement of the inferolateral diaphragm toward the proximal end. The narrowing of the bronchial lumen in the inferolateral lung and the increase of its ventilation, due to the adopted position, creates a higher friction of particles of air over mucus (two-phase flow) and thus favors its movement toward the proximal end.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


