INDICATIONS/CONTRAINDICATIONS
The indications for PDT, laser and cryotherapy range from ablation of superficial early cancers in high-risk patients to palliative treatment of malignant dysphagia and bleeding from advanced esophageal cancer. With the advent of RFA (Barrx Medical, Sunnyvale, CA) for dysplastic BE, the indications for laser ablation and PDT are now limited mostly to palliation of bleeding or obstructing esophageal cancers. RFA burns the mucosal layer of the esophagus while PDT using porfimer sodium (Photofrin; Pinnacle Biologics Inc., Bannockburn, IL) penetrates to the submucosal layer, thus resulting in strictures in up to 42% of patients.15 Cryotherapy is becoming increasingly more available and is being used to ablate dysplastic BE and early neoplasms, palliate malignant dysphagia, and control bleeding. Concurrent chemotherapy and radiation therapy are not considered contraindications to these endoscopic laser and freezing treatments. The presence of a tracheoesophageal or bronchoesophageal fistula is a contraindication for all three modalities (PDT, laser ablation, and cryotherapy).
Photodynamic Therapy and Thermal Laser Therapy Indications
 Palliate malignant dysphagia
Palliate malignant dysphagia
 Control superficial bleeding from esophageal cancer
Control superficial bleeding from esophageal cancer
 Used as a primary or adjunct for treatment of BE, HGD, and intramucosal cancers in medically inoperable patients15–17
Used as a primary or adjunct for treatment of BE, HGD, and intramucosal cancers in medically inoperable patients15–17
Cryotherapy Indications
 Ablation of dysplastic BE
Ablation of dysplastic BE
 Primary tumors of the esophagus
Primary tumors of the esophagus
 Definitive treatment of intramucosal tumors
Definitive treatment of intramucosal tumors
 Local control of esophageal cancer in patients deemed high risk for esophagectomy due to comorbidities
Local control of esophageal cancer in patients deemed high risk for esophagectomy due to comorbidities
 Control bleeding from esophageal cancer
Control bleeding from esophageal cancer
Photodynamic Therapy Contraindications
 Porphyria
Porphyria
 Tracheoesophageal or bronchoesophageal fistula
Tracheoesophageal or bronchoesophageal fistula
 Relative: Hepatic or renal impairment
Relative: Hepatic or renal impairment
Cryotherapy Contraindications
 Tumor that is completely obstructing or near-completely obstructing the esophagus.
Tumor that is completely obstructing or near-completely obstructing the esophagus.
 Tracheoesophageal or bronchoesophageal fistula
Tracheoesophageal or bronchoesophageal fistula
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Prior to the selection of endoscopic therapy, the patient is staged and evaluated, and in patients with early-stage or locally advanced cancer the risk for surgical therapy is assessed. An endoscopy is done to evaluate the extent of disease. If the therapy is offered with curative intent, then a CT scan of the chest and abdomen, endoscopic ultrasound to evaluate the depth of the tumor and nodal status, and a PET-CT scan are done before administering endoscopic therapy to confirm that the tumor is early stage. In patients with more advanced disease, endoscopic therapies can be offered as part of palliative treatment.
Photodynamic Therapy
 Before PDT, the surgeon must educate the patient about the systemic photosensitizing risks of the porfimer sodium. Photofrin (Pinnacle Biologics Inc., Bannockburn, IL) is the most widely used photosensitizing agent, and is approved for use in the United States. Aside from the primary risk of a severe sunburn, other potential side effects include an allergic reaction, chest pain, and wheezing. These must be discussed with the patient before injecting them with Photofrin.
Before PDT, the surgeon must educate the patient about the systemic photosensitizing risks of the porfimer sodium. Photofrin (Pinnacle Biologics Inc., Bannockburn, IL) is the most widely used photosensitizing agent, and is approved for use in the United States. Aside from the primary risk of a severe sunburn, other potential side effects include an allergic reaction, chest pain, and wheezing. These must be discussed with the patient before injecting them with Photofrin.
Thermal Laser Therapy (APC; Nd:YAG)
 No specific planning
No specific planning
Cryotherapy
 Cryotherapy involves the use of nitrogen, a rapidly expanding gas, that if not properly evacuated may lead to perforation of a hollow viscus. A decompression tube is placed in the stomach to eliminate the gas and reduce the risk of injury to the enteric viscera. Placement of this tube may result in postoperative oropharyngeal discomfort. Expelling gas after the procedure is expected.
Cryotherapy involves the use of nitrogen, a rapidly expanding gas, that if not properly evacuated may lead to perforation of a hollow viscus. A decompression tube is placed in the stomach to eliminate the gas and reduce the risk of injury to the enteric viscera. Placement of this tube may result in postoperative oropharyngeal discomfort. Expelling gas after the procedure is expected.
 As the cryogen is released into the esophagus, a transmural freeze occurs and may affect surrounding organs, including the heart. Cardiac arrhythmias from these associated temperature changes may occur. A preoperative cardiac assessment including a recent electrocardiogram is recommended.
As the cryogen is released into the esophagus, a transmural freeze occurs and may affect surrounding organs, including the heart. Cardiac arrhythmias from these associated temperature changes may occur. A preoperative cardiac assessment including a recent electrocardiogram is recommended.
 Risks and side effects should be discussed with the patient prior to surgery.
Risks and side effects should be discussed with the patient prior to surgery.
 SURGERY
SURGERY
All of these endoscopic modalities can be performed as an outpatient procedure either in the main operating room or in a controlled outpatient endoscopy suite. In the operating room, the patient remains supine and is placed under general anesthesia or under monitored anaesthesia care. In the endoscopy suite, the patient is positioned into the left lateral decubitus position; oropharyngeal anaesthesia is achieved with Lidocaine spray, and intravenous conscious sedation is administered. After the endoscope is inserted (Fig. 32.1), the extent of the tumor is examined, biopsies are obtained if indicated, and the procedure is initiated.
Photodynamic Therapy Technique
 The dose of Photofrin is 2 mg/kg, intravenously administered slowly over 3 to 5 minutes.7,10 We wait for 48 hours before administering endoscopic treatment (from photosensitizer injection to administration of light therapy) because tumor cells need time to selectively retain more photosensitizer than normal tissue. This selective retention is due to differences in cancerous tissue vascular supply and lymphatic drainage.7,10
The dose of Photofrin is 2 mg/kg, intravenously administered slowly over 3 to 5 minutes.7,10 We wait for 48 hours before administering endoscopic treatment (from photosensitizer injection to administration of light therapy) because tumor cells need time to selectively retain more photosensitizer than normal tissue. This selective retention is due to differences in cancerous tissue vascular supply and lymphatic drainage.7,10

Figure 32.1 Patient is in left lateral decubitus position, sedated and the endoscope is inserted transorally.
 The injection can be done in the outpatient setting but more often is indicated when the patient has been admitted for bleeding from the tumor or to treat aspiration from malignant obstruction.
The injection can be done in the outpatient setting but more often is indicated when the patient has been admitted for bleeding from the tumor or to treat aspiration from malignant obstruction.
 5-ALA may be used as a photosensitizing agent in Europe. It is not approved as such in the United States.
5-ALA may be used as a photosensitizing agent in Europe. It is not approved as such in the United States.
 During endoscopic therapy/light administration, protective eyewear is required for all operating personnel (Fig. 32.2).
During endoscopic therapy/light administration, protective eyewear is required for all operating personnel (Fig. 32.2).
 A diffusing tip fiber is introduced through the biopsy channel of the endoscope. Available fiber lengths are 1, 2.5, and 5 cm and are chosen depending on the target area.7,18
A diffusing tip fiber is introduced through the biopsy channel of the endoscope. Available fiber lengths are 1, 2.5, and 5 cm and are chosen depending on the target area.7,18
 A 630-nm wavelength laser light is administered at a dose of 300 J/cm of fiber optic diffuser length (Fig. 32.3).
A 630-nm wavelength laser light is administered at a dose of 300 J/cm of fiber optic diffuser length (Fig. 32.3).
 Since the mucosal folds are not flattened, light delivery may not be uniform, and this may lead to an increased dose in some areas, resulting in stricture, and inadequate dosing in others, resulting in incomplete ablation. The use of balloon centering devices may help address this issue by decreasing the mucosal folds and facilitating more uniform delivery (Fig. 32.4).
Since the mucosal folds are not flattened, light delivery may not be uniform, and this may lead to an increased dose in some areas, resulting in stricture, and inadequate dosing in others, resulting in incomplete ablation. The use of balloon centering devices may help address this issue by decreasing the mucosal folds and facilitating more uniform delivery (Fig. 32.4).

Figure 32.2 PDT laser eyewear is required for ocular safety.
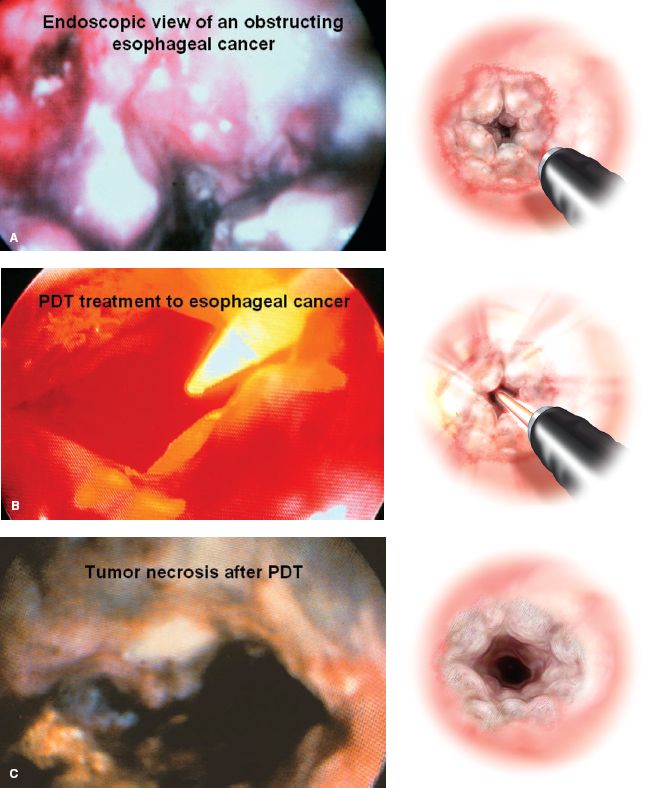
Figure 32.3 Endoscopic view as well as illustration of obstructing esophageal cancer (A) before, (B) during, and (C) after photodynamic therapy (PDT). (From: Abbas G, Pennathur A, Keeley SB, et al. Laser ablation therapies for Barrett’s esophagus. Semin Thorac Cardiovasc Surg. 2005;17(4):313–319, used with permission from Elsevier and the Society of Thoracic Surgeons.).
 A balloon centering device may allow more uniform light exposure resulting in better treatment and fewer strictures. Caution is necessary to avoid overdistention of the esophagus using the balloon as this may decrease blood flow and make the treatment less effective.
A balloon centering device may allow more uniform light exposure resulting in better treatment and fewer strictures. Caution is necessary to avoid overdistention of the esophagus using the balloon as this may decrease blood flow and make the treatment less effective.
 A balloon fiber (Wizard X-Cell PDT balloon, Wilson-Cook Medical, Winston-Salem, NC, USA) has been approved for esophageal PDT. The balloon induces distention of esophageal lumen leading to the flattening of the mucosal folds and is available in three lengths (3, 5, and 7 cm). A pediatric endoscope alongside the balloon can be used to verify the position of the balloon.
A balloon fiber (Wizard X-Cell PDT balloon, Wilson-Cook Medical, Winston-Salem, NC, USA) has been approved for esophageal PDT. The balloon induces distention of esophageal lumen leading to the flattening of the mucosal folds and is available in three lengths (3, 5, and 7 cm). A pediatric endoscope alongside the balloon can be used to verify the position of the balloon.
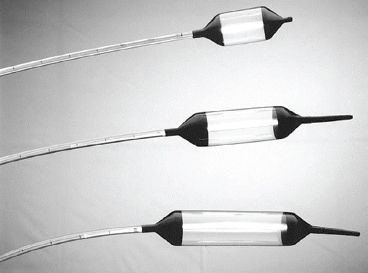
Figure 32.4 Esophageal centering balloons. Reprinted from: Overholt BF, Panjehpour M, Haydek JM. Photo-dynamic therapy for Barrett’s esophagus: Follow-up in 100 patients. Gastrointest Endosc. 1999;49:1–7. Copyright (1999), with permission from Elsevier.



