9 Pharmacology
Note 1: This book is written to cover every item listed as testable on the Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and the WRE, it will simply be shown as: (Code: …). If an item is only testable on the ELE, it will be shown as: (ELE code: …). If an item is only testable on the WRE, it will be shown as: (WRE code: …).
MODULE B
1. Administer medications
2. Bronchodilators
a. Inhaled adrenergic (sympathomimetic) agents
1. Recommend their use (ELE code: IIIG4a) [Difficulty: ELE: R, Ap, An]
2. Administer the prescribed medication (Code: IIIC3, IIID5a, IIID5b) [Difficulty: ELE: R, Ap; WRE: An]
a. Acute bronchospasm with severe shortness of breath.
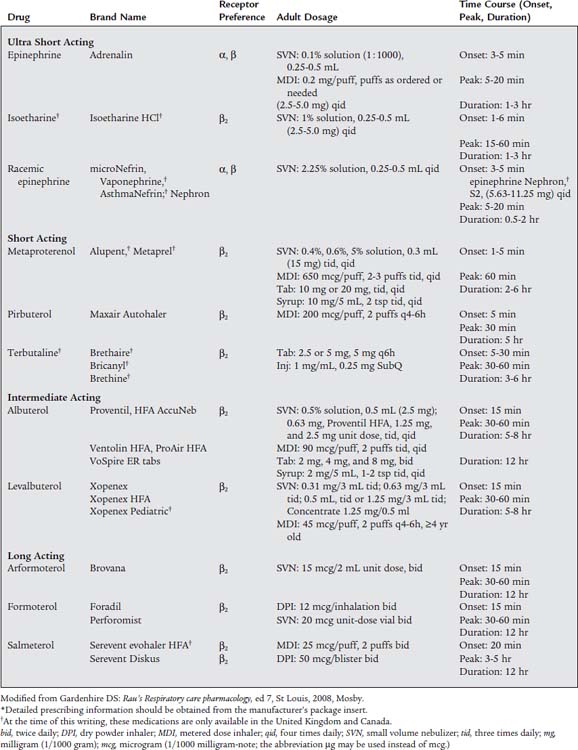
This patient needs rapid relief. Recommend a fast-acting medication such as albuterol. The current asthma-management guidelines list albuterol and similar medications as “rescue” agents. Because these drugs tend to have a shorter duration of action they can be referred to as short-acting beta-agonist (SABA) medications. Table 9-1 lists the peak onset times and duration for the various medications. Avoid drugs with unnecessary α1 and β1 effects or long onset and peak times.
b. Chronic but stable bronchospasm with moderate shortness of breath.
These patients need a dependable medication of longer duration such as salmeterol or formoterol. They are considered to be “controller” agents with a long onset time and a duration of up to 12 hours. Because of their longer duration they can be called long-acting beta-agonist (LABA) medications. Several newer medications also come in both oral and aerosol preparations. The oral forms are especially helpful when taken in the evening to help the patient get a good night’s sleep. It is very important that the patient also have a prescription for a fast-acting drug in case of sudden bronchospasm. Table 9-1 lists information on the administration method, strength, and dosages.
c. Laryngeal edema or bleeding from a bronchoscopy biopsy site.
The laryngeal edema problem requires the administration of a medication that reduces the swelling of the mucous membrane of the larynx and epiglottis. Laryngeal edema can result from a direct injury or irritation of the upper airway, such as postextubation edema or laryngotracheobronchitis (croup). In addition, if the patient has anaphylaxis from an allergic reaction, laryngeal edema and hypotension are often present. If bleeding results from a biopsy during a bronchoscopy, the cut blood vessels must be made to constrict and to form clots. In cases of laryngeal edema or biopsy bleeding, nebulized racemic epinephrine (microNefrin) is given because it stimulates α1-receptors. This results in vasoconstriction of the mucosal and deeper blood vessels. Therefore the laryngeal edema swelling is reduced, and biopsy bleeding stops. In the case of anaphylaxis with hypotension and laryngeal edema, intravenous epinephrine is needed to treat both life-threatening problems. See Table 9-1 for information on specific medications.
Most of the medications listed in this section are chemically derived from adrenaline. They are somewhat different in their structures so that the desired effects and side (unwanted) effects vary. Box 9-1 lists the side effects of the sympathomimetic bronchodilators. Clinically, the most dangerous of these side effects are palpitations, tachycardia, and hypertension.
BOX 9-1 Clinically Observed Side Effects of Sympathomimetic Aerosolized Bronchodilators
(from the Most Commonly Seen to the Least Commonly Seen)
b. Inhaled anticholinergic (parasympatholytic) agents
2. Administer the prescribed medication (Code: IIIC3, IIID5a, IIID5b) [Difficulty: ELE: R, Ap; WRE: An]
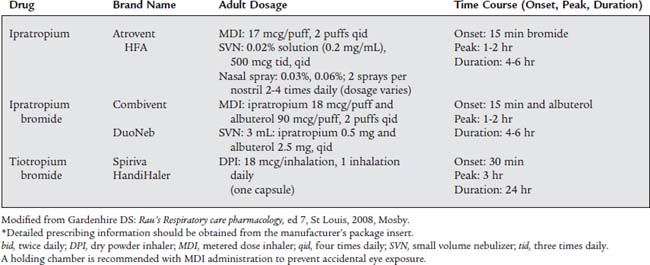
Many patients with COPD and asthma will be treated with nebulized medications from both the sympathomimetic and the parasympatholytic groups. Combivent and DuoNeb combine a sympathomimetic and a parasympatholytic medication. The newest drug in this group, tiotropium bromide (Spiriva), provides the patient with 24 hours of the medication’s benefits. See Table 9-2 for information on the parasympatholytic medications.
3. Antiinflammatory agents
a. Inhaled corticosteroids
1. Recommend use of corticosteroids (ELE code: IIIG4b) [Difficulty: ELE: R, Ap, An]
Corticosteroids affect the respiratory system in two ways: they potentiate the effects of the sympathomimetic agents, and they stop the inflammatory response seen in the airways of asthmatic patients after exposure to an allergen. This prevents mucosal edema from developing. The patient with chronic airflow obstruction, such as asthma or asthmatic bronchitis, should be given inhaled corticosteroids. When they are used as directed, relatively little systemic (bodily) absorption occurs. However, it is best to monitor the patient, especially small children taking inhaled corticosteroids for an extended period, for any side effects. Current guidelines for asthma management classify corticosteroids as “controller” medications that are taken to prevent an asthma attack.
2. Administer the prescribed medication (Code: IIIC3, IIID5a, IIID5b) [Difficulty: ELE: R, Ap; WRE: An]
Table 9-3 shows specific strength and dosage information for the inhaled corticosteroids.
TABLE 9-3 Inhaled Corticosteroids Agents*
| Drug | Brand Name | Formulation and Dosage |
|---|---|---|
| Beclomethasone dipropionate HFA | QVAR | |
| Budesonide | Pulmicort | DPI: 200 mcg/actuation |
| Turbuhaler | Adults: 200-400 mcg bid,† 200-400 mcg bid,† 400-800 mcg bid‡§ | |
| Children ≥6 yr: 200 mcg bid | ||
| Pulmicort | DPI: 90 mcg/actuation, 180 mcg/actuation | |
| Flexhaler | Adults: 180-360 mcg bid usual dose range, 720 mcg bid maximum Children ≥6 yr: 180 mcg bid usual dose, 360 mcg bid maximum | |
| Pulmicort | SVN: 0.25 mg/2 mL, 0.5 mg/2 mL, 1 mg/ml | |
| Respules | Children 1-8 yr: 0.5 mg total dose given once daily, or twice daily in divided doses;*† | |
| 1 mg given as 0.5 mg bid or once daily§ | ||
| Budesonide and formoterol fumarate HFA | Symbicort | MDI: Adults ≥12 yr: 80 mcg budesonide with 4.5 mcg formoterol/actuation, 2 puffs bid; and 160 mcg budisonide with 4.5 mcg formoterol/actuation, 2 puffs bid |
| Maximum daily dose: 640 mcg budisonide and 18 mcg formoterol | ||
| Flunisolide hemihydrate HFA | Aerospan | MDI: 80 mcg/puff |
| Adults ≥12 yr: 2 puffs bid, adults no more than 4 puffs daily | ||
| Children 6-11 yr: 1 puff daily, no more than 2 puffs daily | ||
| Flunisolide | AeroBid, AeroBid-M | MDI: 250 mcg/puff |
| Adults and children ≥6 yr: 2 puffs bid, adults no more than 4 puffs daily Children ≤15 yr: no more than 2 puffs daily | ||
| Fluticasone propionate | Flovent HFA | MDI: 44 mcg/puff, 110 mcg/puff, 220 mcg/puff |
| Adults ≥12 yr: 88 mcg bid,* 88-220 mcg bid,† or 880 mcg bid§ | ||
| Children 4-11 yr: 88 mcg bid | ||
| Flovent Diskus | DPI: 50 mcg, 100 mcg, 250 mcg | |
| Adults: 100 mcg bid*100-250 mcg bid,† 1000 mcg bid§ | ||
| Children 4-11 yr; 50 mcg twice daily | ||
| Fluticasone propionate/salmeterol | Advair Diskus | DPI: 100 mcg fluticasone/50 mcg salmeterol, 250 mcg fluticasone/50 mcg propionate/salmeterol, or 500 mcg fluticasone/50 mcg salmeterol salmeterol |
| Adults and children ≥12 yr: 100 mcg fluticasone/50 mcg salmeterol, 1 inhalation twice daily, about 12 hr apart (starting dose if not currently on inhaled corticosteroids) | ||
| Maximum recommended dose 500 mcg fluticasone/50 mcg salmeterol twice daily | ||
| Children ≥4 yr: 100 mcg fluticasone/50 mcg salmeterol, 1 inhalation twice daily, about 12 hr apart (for those who are symptomatic while taking an inhaled corticosteroid) | ||
| Advair HFA | MDI: 45 mcg fluticasone/21 mcg salmeterol, 115 mcg fluticasone/21 mcg salmeterol, or 230 mcg fluticasone/21 mcg salmeterol salmeterol, | |
| Adults and children ≥12 yr: 2 inhalations twice daily, about 12 hr apart | ||
| Mometasone furoate | Asmanex | DPI: 220 mcg‡ actuation, 110 mcg actuation for children 4-11 |
| Twisthaler | Adults and children ≥12 yr: 220-440 mcg daily,† 220-440 mcg daily,* 480-880 mcg daily§ | |
| Triamcinolone acetonide | Azmacort | MDI: 75 mcg/puff |
| Adults ≥12 yr: 2 puffs tid or qid | ||
| Children ≥6 yr: 1-2 puffs tid or qid |
bid, twice daily; qid, four times daily; tid, three times daily.
* Detailed prescribing information should be obtained from the manufacturer’s package insert.
† Recommended starting dose if on bronchodilators alone.
‡ Recommended starting dose if on inhaled corticosteroids previously.
§ Recommended starting dose if on oral corticosteroids previously.
Modified from Gardenhire DS: Rau’s Respiratory care pharmacology, ed 7, St Louis, 2008, Mosby.
b. Cromolyn sodium
1. Recommend the use of cromolyn sodium (ELE code: IIIG4b) [Difficulty: ELE: R, Ap, An]
Cromolyn sodium (Intal) and nedrocromil sodium (Tilade) are indicated to prevent an asthma attack. They accomplish this by coating the mast cells found in the airways so that they do not degranulate and rupture. Without pretreatment, the mast cells of asthmatic patients would rupture when exposed to immunoglobulin E (IgE) from their allergen(s). This mast cell rupture would result in the spilling of leukotriene agents, histamine, and other chemical mediators that cause the bronchospasm, airway edema, and increased airway secretions of an asthma attack.
2. Administer the prescribed medication (Code: IIIC3, IIID5a, IIID5b) [Difficulty: ELE: R, Ap; WRE: An]
When cromolyn sodium, or nedrocromil sodium, is inhaled at least 1 week before exposure to the allergen, the asthmatic reaction is prevented or reduced. Cromolyn was first made available through a dry powder inhaler and is now only available by metered dose inhaler or small volume nebulizer (SVN). Nedrocromil sodium is similar to cromolyn in its use and effects. It is available in a metered dose inhaler. See Table 9-4 for detailed information on both medications.
TABLE 9-4 Inhaled Nonsteroidal Antiasthma Agents*
| Drug | Brand Name | Formulation and Dosage |
|---|---|---|
| CROMOLYN-LIKE (MAST CELL STABILIZERS) | ||
| Cromolyn sodium† | Intal | MDI: 800 mcg/actuation |
| Adults and children ≥5 yr: 2 inhalations 4 times daily | ||
| SVN: 20 mg/amp or 20 mg/vial | ||
| Adults and children ≥2 yr: 20 mg inhaled 4 times daily | ||
| Nasalcrom | Spray: 40 mg/mL (4%), gives 5.2 mg of drug | |
| Adults and children ≥2 yr: 1 spray each nostril, 3-6 times daily every 4-6 hr | ||
| Nedocromil sodium | Tilade | MDI: 1.75 mg/actuation |
| Adults and children ≥6 yr: 2 inhalations 4 times daily | ||
| ANTILEUKOTRIENES | ||
| Montelukast | Singulair | Tablets: 10 mg, 4 mg, and 5 mg cherry-flavored chewable; 4 mg packet of granules |
| Adults and children ≥15 yr: one 10 mg tablet daily in evening | ||
| Children 6-14 yr: one 5 mg chewable tablet daily | ||
| Children 2-5 years: one 4 mg chewable tablet or one 4 mg packet of granules daily | ||
| Children 6-23 months: one 4 mg packet of granules daily | ||
| Zafirlukast | Accolate | Tablets: 10 and 20 mg |
| Adults and children ≥12 yr: 20 mg (1 tablet) twice daily, without food | ||
| Children 5-11 yr: 10 mg twice daily | ||
| Zileuton | Zyflo | Tablets: 600 mg |
| Zyflo CR | Adults and children ≥12 yr: one 600 mg tablet 4 times a day | |
| MONOCLONAL ANTIBODY | ||
| Omalizumab | Xolair | Adults and children ≥12 yr: subcutaneous injection every 4 weeks; dose dependent on patient’s weight and serum IgE level |
* Detailed prescribing information should be obtained from the manufacturer’s package insert.
† Note: Cromolyn sodium is also available in an oral concentrate giving 100 mg in 5 mL (Gastrocrom) for treatment of systemic mastocytosis, and as an ophthalmic 4% solution (Opticrom, 40 mg/mL) for treatment of vernal keratoconjunctivitis.
Modified from Gardenhire DS: Rail’s Respiratory care pharmacology, ed 7, St Louis 2008, Mosby.
c. Recommend the use of leukotriene modifiers (ELE code: IIIG4b) [Difficulty: ELE: R, Ap, An]
Leukotrienes are chemicals found in mast cells that are released during an asthma attack. These released leukotriene chemicals stimulate bronchospasm, airway edema, and increased airway secretions. The leukotriene-modifier (also called leukotriene antagonists) medications work to reduce the number of leukotriene chemicals that are released or to block the effect of leukotrienes on the airways. By accomplishing this, the patient’s asthma symptoms are reduced or eliminated. See Table 9-4 for detailed information on all four medications in this group.
4. Mucolytics or proteolytic agents
a. Acetylcysteine
2. Administer the prescribed medication (Code: IIIC3, IIID5a) [Difficulty: ELE: R, Ap; WRE: An]
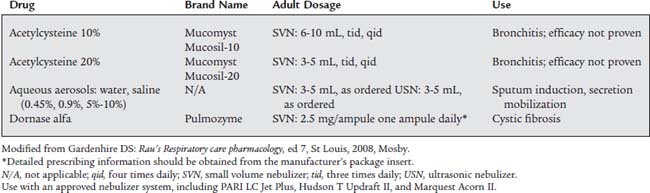
Mucomyst is usually administered with a small volume nebulizer (SVN) or with intermittent positive-pressure breathing (IPPB). Most adult patients are given up to 3 to 5 mL of the 20% solution or up to 6 to 10 mL of the 10% solution. The 20% solution is often diluted with an equal volume of normal saline solution. Direct instillation of 1 to 2 mL of the drug into the trachea also helps to liquefy secretions. The manufacturer recommends that all medication in a vial be used within 96 hours or discarded. It should be stored in the refrigerator. A slightly purple color is commonly seen after the vial has been opened, but it can still be used safely. See Table 9-5 for specific information.
b. RhDNAse
2. Administer the prescribed medication (Code: IIIC3, IIID5a) [Difficulty: ELE: R, Ap; WRE: An]
Usually a single daily dose of 2.5 mL of solution (containing 2.5 mg of dornase alfa) is inhaled by SVN. Store the drug in a refrigerator, and protect it from strong light. It has no serious side effects. See Table 9-5 for detailed information.
c. Hypertonic saline
1. Recommend the use of hypertonic saline (ELE code: IIIG4c) [Difficulty: ELE: R, Ap, An]
The various saline solutions (and sterile water) are known collectively as “bland” aerosols, because they have no direct pharmacologic effect on the lungs and airways. When they are inhaled as aerosols, however, a vagal nerve–mediated reflex causes the bronchial/submucosal glands to release more watery secretions. Therefore a saline aerosol is commonly used to help liquefy secretions and induce a patient to expel sputum. Recent clinical experience has shown hypertonic saline to be an effective mucolytic in cystic fibrosis patients.
2. Administer the prescribed medication (Code: IIIC3, IIID5a) [Difficulty: ELE: R, Ap; WRE: An]
The various saline solutions are given through an SVN or IPPB treatment or, more commonly, mixed with a bronchodilator medication. See Table 9-5 and Box 9-2 for information on the various saline solutions.